Bacteriological Study of Unilateral Maxillary Sinusitis
Received: 24-Apr-2023 / Manuscript No. JIDT-23-96856 / Editor assigned: 27-Apr-2023 / PreQC No. JIDT-23-96856 (PQ) / Reviewed: 05-May-2023 / QC No. JIDT-23-96856 / Revised: 12-May-2023 / Manuscript No. JIDT-23-96856 (R) / Published Date: 19-May-2023 DOI: 10.4172/2332-0877.1000541
Abstract
Odontogenic maxillary sinusitis is predominantly a unilateral maxillary sinus lesion. On examination, a purulent nasal discharge in the middle meatus that occurs unilaterally can be observed. A cone-beam CT can be used to confirm a unilateral maxillary sinus lesion. In this study, periapical lucency, oroantral fistula, aberration of dental material to the maxillary sinus, and aberration of implant tip to the maxillary sinus revealed by CT were diagnosed as odontogenic maxillary sinusitis. In each reported case, pus was aspirated and aerobic and anaerobic cultures were performed.
Keywords: Odontogenic maxillary sinusitis; Bacteria; F. nucleatum; Otolaryngology
Introduction
The bacterial culture results showed that 59 (81.9%) of the 72 isolates in 50 cases were obligate anaerobes [1].The detection rate of Fusobacterium nucleatum (F. nucleatum), a gram-negative rod, was extremely high at 37.5%. This was followed by Prevotella at 25%. Gram-negative rods accounted for 78% of the isolates. Gram-positive coccus, Parvimonas, was detected at 22%. Storage of samples in an anaerobic porter immediately after pus collection is important for the accurate detection of anaerobic bacteria.
Case Presentation
We here present two of our cases.
Case 1
A 43-year-old man presented with chief complaints of right nasal obstruction, and abnormal odor. History of present illness; the patient experienced unilateral nasal obstruction and an unpleasant odor (e.g., rotten fish) for the past one year. A local otolaryngologist diagnosed him with sinusitis. The patient was prescribed clarithromycin, but the nasal discharge and unpleasant odor persisted. Bacterial cultures were not performed.
Endoscopically, purulent nasal discharge from the right middle meatus, resulting in postnasal drip, was observed. Clinically, the patient did not have any buccal pain. The purulent nasal discharge was aspirated into a sterile test tube using an Ishigami aspirator and immediately inoculated into an anaerobic porter. The porter was kept below 4 C until the inspection center came to collect the sample in the evening. At the same time, the collected pus was tested for the presence of spindle-shaped Gram-negative rods by Gram staining in the outpatient laboratory of the clinic. The anaerobic bacteria cultures were observed for up to 14 days for bacterial growth. The culture confirmed that there were spindle-shaped Gram-negative bacilli.
Intraoral findings: Significant caries was noted.
Cone-beam CT findings: Diffuse opacities in the right maxillary sinus were observed. Bordering the maxillary sinus, a periapical radicular cyst associated with the right maxillary permanent second molar (tooth 27) was detected.
Bacterial culture results: Fusobacterium nucleatum (F. nucleatum)
Treatment: CVA/AMPC 1000 mg+AMPC 500 mg, twice daily, for 7 days were prescribed. Subsequently, the unpleasant odor subsided, and the purulent nasal discharge also decreased. Since the effect was insufficient, new respiratory quinolone 75 mg, once daily, was administered orally for 7 days. Consequently, the symptoms disappeared (Figure 1).
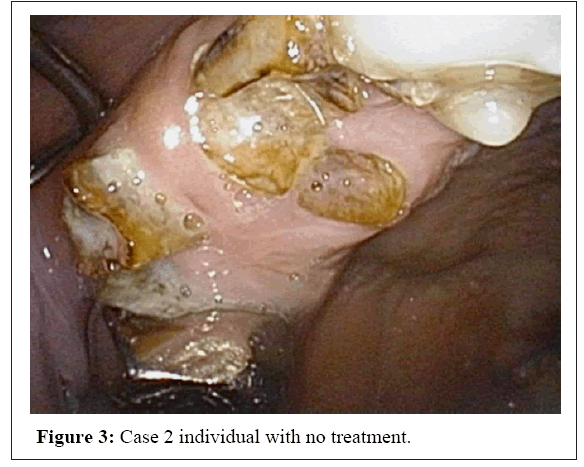
A 55-year-old female housewife presented with chief complaints of right nasal odour from 3 years prior. The unpleasant odour is especially noticeable when the patient bows or looks down (Figures 2 and 3).
Detected bacteria: F. nucleatum, Prevotella buccae, and Prevotella intermedius
Gram stain: Gram-negative spindle-shaped rod confirmed.
Cone beam CT: The right maxillary sinus was diffusely filled with soft tissue. Odontogenic maxillary sinusitis spilling over from marginal gingivitis was diagnosed.
Treatment: CVA/AMP+AMPC twice daily for 7 days. Subsequently, the nasal discharge and unpleasant odor disappeared.
Results and Discussion
Bacteria detected in bacterial maxillary sinusitis generally include Streptococcus pneumoniae, Hemophilus influenzae, and Moraxella catarrhalis, which do not produce an unpleasant odour. Puglisi, et al., found that bacteria involved in chronic sinusitis, such as H. influenzae and M. catarrhalis, were not detected in odontogenic maxillary sinusitis [2].
Two other reports of odontogenic maxillary sinusitis in Japan had been published. Muroki and Tamai collected samples from the reservoir of extraction sockets using a syringe needle [3]. Of the 100 samples collected, 59.1% were aerobic and 40.9% were anaerobic. Veillonella, a Gram-positive coccus accounted for the largest proportion at 48%. Peptostreptococcus was also detected. The Gramnegative rods were Bacteroides and accounted for 2%. Interestingly, there were no Fusobacterium.
Recently, Kaneko reported on 99 cases of dental infections [4]. Among the dental infections, odontogenic maxillary sinusitis reported the lowest detection rate of obligate anaerobes and the highest number of facultative anaerobes. The major obligate anaerobes were Provotella at 18.8%, Peptostreptococcus at 16.8% and Fusobacterium at 3.1%, etc.
In another report outside of Japan, Brook investigated 48 cases and found that anaerobic Gram-negative rods, such as F. nucleatum, P. intermedius, and Bacteroides spp. were the main anaerobic bacteria [5]. However, there are no detailed bacteria detection rates. The reasons for the significant difference between the authors’ anaerobic bacteria detection rates and those reportedly previously are discussed below.
Veillonella, and Peptostreptococcus are relatively resistant to oxygen exposure. In contrast, Fusobacterium and Bacteroides are oxygen-sensitive and they cannot n grow unless their required anaerobic conditions are met [6,8]. Moreover, in normal air, F. nucleatum, Provotella and Porphyromonas spp. tend to die within 10-30 minutes. Furthermore, these anaerobes require a long incubation period (about 7 days) for colony formation. If the right conditions are not provided during culturing, a decrease in enumeration is to be expected [7]. In Japan, the low detection rate of anaerobic bacteria, especially F. nucleatum and Bacteroides has been attributed to inappropriate anaerobic conditions during incubation.
Conclusion
In pediatric acute maxillary sinusitis, respiratory bacteria were detected in 65% of the sinus aspirates and both bacteria and viruses in 32%. The most bacteria were Fusobacterium nucleatum, Prevotella buccae, and Prevotella intermedius, Streptococcus pneumoniae, Hemophilus influenzae, and Moraxella catarrhalis, Viral and bacterial Polymerase chain reaction is useful for accurately investigating the microbiology in pediatric sinusitis. Identification of the species causing maxillary sinus infections is essential when specific treatment is required in patients resistant to standard antimicrobial therapy. Different studies have shown that certain species of bacteria isolated from maxillary sinus cultures are more frequently associated with sinusitis. Furthermore, in this type of case, bacterial cultures of aspirates can be useful for clinicians in the differential diagnosis of sinusitis.
References
- Rinya S, Gen S, Eiji Y, Kiyoshi A (2022) Bacteriological clinical studies of 50 cases of dental maxillary sinusitis. J Immunology Allergy Infect Otorhinol 2: 169-177.
- Puglisi S, Privitera S, Maiolino L (2011) Bacteriological findings and antimicrobial resistance in odontogenic and non-odontgenic maxillary sinusitis. J Med Microbiol 60: 1353-1359.
[Crossref] [Google Scholar] [PubMed]
- Muroki T, Tamai K (1986) Clinical bacteriological study of odontogenic maxillary sinusitis. J Jpn Stomatol Soc 35: 826-839.
[Crossref]
- Kaneko A (2015) Bacteriology of dental infections. Pharmacotherapy 34: 85-93.
[Crossref]
- Brook Iz (2008) Anaerobic infection and management. Expert Rev Anti Infect Ther 2: 135-153.
[Crossref]
- de Mecedo Farias L, de Carvalho MAR, Houw H (1999) Atmospheric oxygen sensitivity of Fusobacterium Strains. Anaerobe 5: 157-159.
[Crossref]
- Kawamura T, Nakamura T, Watanabe K, Kaimori M (2002) Clinical bacteriological analysis of 108 cases involving Fusobacterium experienced in 5 years. J Jpn Assoc Infect Dis 76: 23-90.
[Crossref]
Citation: Sugita R, Sugita G, Yanagisawa H, Asakura K (2023) Bacteriological Study of Unilateral Maxillary Sinusitis. J Infect Dis Ther 11:541. DOI: 10.4172/2332-0877.1000541
Copyright: © 2023 Sugita R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2289
- [From(publication date): 0-2023 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 1891
- PDF downloads: 398