Review Article Open Access
Bacterial Spores and its Relatives as Agents of Mass Destruction
Sebastián Cogliati, Juan Gabriel Costa, Facundo Rodriguez Ayala, Verónica Donato and Roberto Grau*
Departamento de Microbiología, Universidad Nacional de Rosario, Argentina
- *Corresponding Author:
- Grau R
Departamento de Microbiología
Universidad Nacional de Rosario
Argentina
E-mail: robertograu@fulbrightmail.org
Received Date: December 15, 2015; Accepted Date: March 03, 2016; Published Date: March 10, 2016
Citation: Cogliati S, Costa JG, Ayala FR, Donato V, Grau R (2016) Bacterial Spores and its Relatives as Agents of Mass Destruction. J Bioterror Biodef 7: 141. doi: 10.4172/2157-2526.1000141
Copyright: © 2016 Cogliati S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Bioterrorism & Biodefense
Abstract
The term bioterrorism has acquired full force for the planetary consciousness from the very beginning of the new century. Indeed, from the events that occurred during October and November of 2001 with the intentional contamination with spores of pathogenic Bacillus anthracis, of letters distributed by the US public postal service and the terrorist attacks in the last months of 2015 in Egypt, France, Mali, Afghanistan, Turkey, USA and other countries have warned again about the reality of the bioterrorist threat and its immeasurable cultural and undesirable economic and political consequences. In this review we summarize the main structural characteristics that make the spores of Bacilli and Clostridia as the ideal agents for use in bioterrorism. In addition, we discuss the properties of non-sporulating Coxiella burnetii, the causative agent of Q fever, because of its peculiar resistance, high infectivity and environmental persistence that resembles true spores.
Keywords
Spores; Anthrax; Botulism; Gas gangrene; Diarrhoea; Q fever; Prevention response to bioterrorism
Introduction
Bioterrorism in the world today
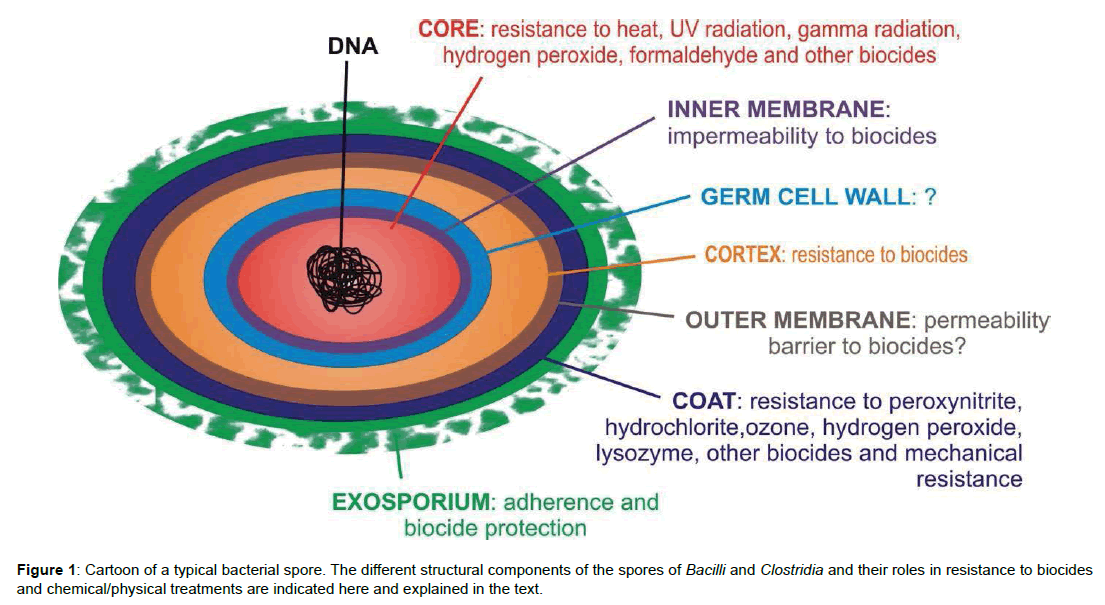
Biological weapons, as opposed to nuclear weapons, are easier to produce and require far less investment in money and human resources [1-8]. It is believed, that if an attacker (a country, a sect or an individual) wanted to harm another (people of a country) the economic cost to affect the enemy territory using a nuclear weapon will be considerably much higher than using a biological weapon [8]. Therefore due to its low cost, ease of production and fearful danger it is that biological weapons pose a real threat to modern societies [2,4,6]. Unlike a biological warfare (between countries) or a biocrimen (against one person) in a bioterrorist attack the general civilian population is the target. In this sense, an act of bioterrorism can be defined as the intentional use of live biological agents (mainly bacteria and viruses) or their derivatives (mainly toxins) to cause panic, illness and / or death in the population. Because of the relative ease of developing biological weapons not only states or nations are able to sponsor bioterrorist attacks but also sects, fundamentalists and even individuals, i.e. a lone wolf terrorist, who wish to do so [1,4]. Today all mankind is threatened of a possible attack with a weapon of mass destruction. Even in cases of false alarm the economic costs to the threatened country to originate prevention and implementation of response plans are repeatedly millionaires in terms of national budgets [9-14], not to mention the psychological damage on the civilian population that hurts the society narcissism in the depths of his being [2-4,9-14]. If what is sought is the biggest physical and / or psychological damage with the lowest economic cost then: what should be the ideal characteristics of a biological agent as a weapon of mass destruction? Well, it should comply with as much of the following characteristics: be cheap, easy to hide and to produce in large quantities, should have no smell, taste or characteristic colour that reveal its presence before unleashing its toxic and/or lethal effect, should be able to be aerosolized, must survive as long as possible to its exposure to sunlight, should be as resistant as possible to drying and heat, it should be capable of producing massive death or serious illness (i.e. have a high infectivity rate even in a low dose), must be contagious from person to person, and there should not be available (at least in a timely manner) medical treatment or prophylaxis once warned the attack [2- 4,9]. Among all these features perhaps aerosolization deserves a further comment due to its importance in case of a bioterrorist attack [1,2]. This term refers to the particle size that the microbial agent should have (1 to 10 micrometres in diameter) to effectively spread through the air. For comparison, a particle of 1 mm of diameter is able to travel through the air along a distance of 1 meter before falling, whereas a particle of 0.5 microns of diameter travels through the air over 1,000 (thousand) kilometres before “settle” on a surface or be unnoticed inhaled (breathed) by a person, reaching the deepest parts of the lungs (the alveoli) from where the infectious agent spreads to cause disease and / or death [15-17]. Precisely, in the microbial world, bacteria and viruses are the infectious agents that perfectly meet the sized requirement to be compacted into fine powders feasible to spread through the air. The infective powder will access the human alveoli and will start the disease that in all cases will go unnoticed as a simple cold or flu during the first days until to show up as it really is (Anthrax, Botulism, Gas gangrene, Q fever, etc.). Unfortunately, by that time, the medical treatment would in most cases go fruitless. When cells of certain Gram-positive bacteria encounter environmental stresses such as nutrient starvation, they form a dormant structure termed a spore [18,19]. Bacterial spores can survive in this dormant state for many years. Faced with the challenge of surviving prolonged periods of dormancy, spores have evolved many mechanisms to protect themselves from damage, which also serve to protect them from modern disinfection/sterilization procedures [20- 23] (Figure 1).
Microbial agents of mass destruction
Biological agents that could or have been used as biological weapons of destruction or mass panic can be divided into two types:
- Live microorganisms (bacteria, fungi and viruses).
- Poisons or toxins derived from microorganisms (mainly bacteria and fungi), plants, snakes, etc.
Evidently, microbes play a central role as agents of bioterrorist utilization. Perhaps the most useful classification is given by the Centre for Infectious Disease Control (CDC) which ranks microorganisms in three Categories or Classes (A to C) according to the suitability for their use in bioterrorism acts, on how easily can be spread and the severity of illness or death they cause (www.emergency.cdc.gov/bioterrorism) (Table 1). Following these criteria, category A agents are considered the highest risk and category C agents are those that are considered emerging threats for disease (Table 1).
| Category A (natural or engineered organisms or toxins that represent the highest risk to the public and national security) |
Category B (moderately highest priority) |
Category C (emerging pathogens) |
| ◊They can be easily spread or transmitted from person to person, ◊They result in high death rates and have the potential for major public health impact ◊They might cause public panic and social disruption ◊They require special action for public health preparedness |
◊They are moderately easy to spread ◊They result in moderate illness rates and low death rates ◊They require specific enhancements of CDC’s laboratory capacity and enhanced disease monitoring |
◊They are easily available ◊They are easily produced and spread ◊They have potentiality for high morbidity and mortality rates |
Table 1: Main characteristics used by CDC to classify bacterial agents in function of the probability of their utilization and the danger would produce after a bioterrorist attack.</`
In Class A there are the most dangerous microbes, i.e. those who meet the highest number of “desirable” properties of a bioterrorist agent (bacteria or virus) mentioned before and listed in (Table 1). In category B are included those agents who have been assigned a low priority and those in category C are of relative priority, including hypothetical or emerging pathogens. Examples of Class A microorganisms and diseases caused by them are Ebola virus, Bacillus anthracis (anthrax), Yersinia pestis (plague), Clostridium botulinum (botulism toxin), Francisella tularensis (tularemia), and Variola virus (smallpox). Examples of Class B microorganisms are Burkholderia sp. (melioidosis, glanders), Brucella sp. (brucellosis or undulant fever), Coxiella burnetii (Q fever), Chlamydia psittaci (psittacosis), Clostrifium perfringens (epsilon toxin) and Hepatitis A virus.
In this review we want to emphasize those microorganisms capable of forming the strongest living structure that the human knows: the spore cell (Figure 1) [18-20]. Bacterial spores could represent bioterrorist agents of spectacular concern in case of used by the wrong hands. In this sense, the Class A microorganisms C. botulinum and B. anthracis and the Class B microorganism C. perfringens belong to the select group of spore-forming bacteria indicated by the CDC. It is important to consider that in the case of C. botulinum (Class A) and C. perfringens (Class B), the CDC only takes into consideration the bioterrorist use (in food and water) of the botulism toxin and epsilon toxin, produced by C. botulinum and C. perfringens, respectively, and not the bioterrorist utilization of aerosols containing spores of these bacteria as it is the case for B. anthracis [24-26]. Therefore, we want to analyse here the potential use of aerosolized C. botulinum and C. perfringens spores in bioterrorism.
In addition, we also consider the potential use of the aerosolized pathogens C. difficile and Coxiella burnetii. C. dificcile is responsible for the production of deadly diarrhoea in humans but is not considered by the CDC as a biological agent of potential bioterrorist use. However, recently emerged strains of this spore-forming bacterium, considered as “superbug”, are multi resistant to antibiotics and more virulent and therefore we hypothesize that C. difficile spores might be successfully used in a bioterrorist attack [27,28]. By other side, the class B agent Coxiella burnetii (Table 1) is the etiological cause of Q fever in animals and humans [29] but it doesn´t sporulate. However, although C. burnetii doesn’t produce real spores we include this pathogen in the present review because produces a unique cell (small cell variant, SCV) of high robustness, persistence and infectivity that resemble a bacterial spore [30].
The bacterial spore: structural features for its high resistance and virulence
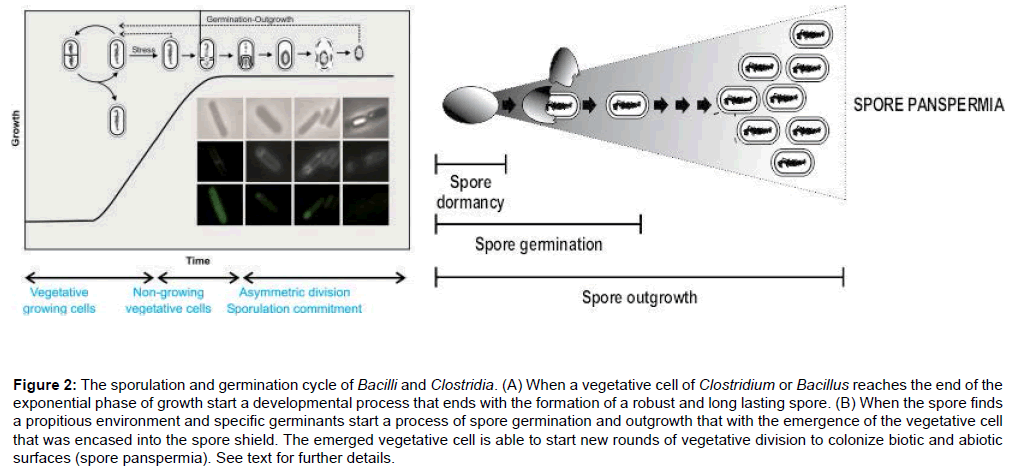
Some spore-forming bacteria, belonging to the Clostridium and Bacillus genera, are associated with diseases [20]. Examples of these illnesses are tetanus (Clostridium tetani), botulism (Clostridium botulinum), gas gangrene (Clostridium perfringens), CDI (Clostridium difficile infections) and anthrax (Bacillus anthracis). Many of these diseases are not frequent developed countries because the use of appropriate hygienic practices, vaccines and right antibiotics. Nevertheless, highly virulent variants of these pathogens have emerged, because of the overuse/misuse of antibiotics, as well as the genetic modification of spore-forming strains [31-35]. In addition to this clinical notoriety, these two bacterial genera (Bacillus and Clostridium) have also been very successful to survive in the environment, due at least in part to their ability to form spores (Figures 1 and 2). Spores and spore-forming bacterial species have been found in nearly every habitat on earth, including as part of the normal flora of animals and human beings. Due to their inherent resistance to decontamination as well as unique biology, bacterial spores pose a particular challenge to infection control, food storage and safety and traditional clinical interventions [18-21] (Figure 1). Understanding the role that spores play in the environment as well as in disease will be an important step towards mitigating the threat posed by these bacteria [20-23].
Figure 2: The sporulation and germination cycle of Bacilli and Clostridia. (A) When a vegetative cell of Clostridium or Bacillus reaches the end of the exponential phase of growth start a developmental process that ends with the formation of a robust and long lasting spore. (B) When the spore finds a propitious environment and specific germinants start a process of spore germination and outgrowth that with the emergence of the vegetative cell that was encased into the spore shield. The emerged vegetative cell is able to start new rounds of vegetative division to colonize biotic and abiotic surfaces (spore panspermia). See text for further details.
The differentiation of actively growing (vegetative) Bacillus and Clostridium organisms into spores is a multistep process that occurs in response to environmental and metabolic clues (Figure 2A) [18,19]. The sporulation process is a carefully orchestrated cascade of events at both the transcriptional and post-translational levels involving several sigma factors of the RNA polymerase, transcription factors, proteases, phosphatases and quorum sensing molecules [18,19]. Upon completion of the process, the spore is released into the extracellular milieu by autolysis of the mother cell (Figure 2A). The entire developmental program takes, in the laboratory under optimal conditions, approximately 8 h to complete [18]. Dormant spores can remain viable for extremely long periods of time in the environment, and are highly resistant to adverse conditions [15,21-23]. The concentric series of structures that formed the spore are responsible for its resistance and longevity (Figure 1).
Spores have evolved to germinate (or reactivate) inside a host (in response to the presence of nutrients or germinants) causing disease because of toxin production (Figure 2B) [20].
Bacterial spores are likely the most resistant and durable form of life on Earth. The spore’s structure and chemical composition play major roles in spore resistance. Spores are resistant to a variety of antimicrobial and biocide compounds, extremes of temperature and pH, UV and ionizing radiation, and can survive for extreme lengths of time without water or nutrients [22,23]. Furthermore, the spore’s core is dehydrated with a concomitant increase in Ca2+ and dipicolinic acid (DPA) concentrations which jointly protect against heat stress (Figure 1) [22,23]. In addition, the spore’s DNA is enveloped by a specialized class of proteins called small acid-soluble proteins (SASPs), which protect the DNA from UV and gamma radiations during dormancy [22,24-37]. Since spores are metabolically dormant, they bacteria have the advantage to pass unharmed and unnoticed through diverse environments before germination (Figure 2A). Starting from the outside of the spore, the spore layers include the exosporium, coat, outer membrane, cortex, germ cell wall, inner membrane and central core (Figure 1) [18,22,23].
Structural analyses of spores have revealed that they possess a flexible balloon-like structure (Figure 1). The exosporium is the outermost structure of many bacterial spores, in particular those of the B. cereus group, which also includes B. anthracis and B. thuringiensis, but is also found in some other Bacilli and Clostridia, including the pathogenic C. difficile and C. botulinum [20-23]. The exosporium, which has been shown to protect the spores, facilitates the adherence to biotic and abiotic surfaces, allowing the spores to spread between infected individuals and between contaminated and uncontaminated surfaces [20,23,38-40] (Figure 1). Therefore, adherence of spores to host-cells has been suggested to be a critical virulence factor. Adherence plays a key role in the spore infectious potential. This is of particular concern in the hospital setting, where walls, floors, appliances and other surfaces, as well as healthcare workers themselves, can become a reservoir of infectious particles [40]. Spores of Bacillus anthracis adhere to cells of the airway and intestinal epithelia, a property that potentiate the virulence of this pathogen [41,42]. A collagen-like protein of the B. anthracis exosporium (BclA) has been implicated in the binding to the Mac-1 cell surface receptor of macrophages, inducing its own phagocytosis by those host cells [43]. In addition, the immuneinhibitor A protein (InhA) of Bacillus cereus, a metalloprotease found in the exosporium, has also been found to be involved in escape from the macrophage endosome after spore internalization [39-44].
The spore coat is a complex structure composed of several layers and is made up mainly of proteins, most of which are spore-specific gene products. The coat is important in spore resistance to exogenous lytic enzymes that can degrade the spore cortex and to predation by protozoa and to some chemicals, especially oxidizing agents such as hydrogen peroxide, ozone, peroxynitrite, chlorine dioxide and hypochlorite, all of which kill spores more rapidly when the coat layer is absent, but has little or no role in spore resistance to heat, radiation and some other chemicals [22,23,45].
The precise function of the outer membrane that lies under the spore coats is not clear, although this membrane is an essential structure in spore formation [18,19,22]. The cortex is composed of peptidoglycan (PG) with a structure similar to that of vegetative PG but with several spore-specific modifications [18,19,22,46]. The cortex is essential for formation of a dormant spore and for the reduction of the water content of the spore core. The inner spore membrane is a strong permeability barrier that plays a major role in spore resistance to many chemicals, in particular those that could damage the spore DNA [21-23,36,37].
Finally, the core contains most spore enzymes as well as DNA, ribosomes and tRNAs. The low core water content is likely the major factor in the spore’s enzymatic dormancy, and is the most important factor determining the spore’s resistance to wet heat. As mentioned before, a core small molecule important in spore resistance is DPA [36,37]. This molecule comprises 5–15% of the dry weight of spores of both Bacillus and Clostridium species and is located only in the core, where it is most likely chelated with divalent cations, largely Ca2+. DPA plays a significant role in the UV photochemistry of spore DNA [36,37]. Another type of core molecules that play an important role in spore resistance is the SASPs. The binding of these proteins alters DNA’s structure and properties dramatically, and these proteins are significant factors in spore resistance to heat and many chemicals, and a major factor in spore resistance to UV radiation [21-23,36,37]. In addition to preventing DNA damage, the spore has another mechanism to minimize damage: it has a rapid and efficient DNA repairing mechanism of any DNA damage that could happened during spore dormancy that is activated during spore outgrowth before takes place the first division cycle of the emerged cell (Figure 2B) [22,37]. It has been suggested that superoxide dismutase (SOD), an enzyme associated with the exosporium or spore coat of B. cereus and B. anthracis, is involved in the formation of the spore coat, may also serve to detoxify potentially damaging chemicals at the spore surface [23,47]. Other role also exhibited by the activity of SOD enzymes is to evade host responses. Spores of B. anthracis contain several superoxide dismutases, which provide resistance to the oxidative burst produced by macrophages after the phagocytosis of B. anthracis [23,47]. In addition, a nitric-oxide synthase activity in B. anthracis spores also provides protection from macrophage-mediated killing, complicating medical treatment [41,42]. Spore resistance can also play a more direct role in disease development by allowing spores to survive attack by the host’s phagocytic cells. In the case of Clostridium difficile, the causative agent of antibiotic-associated diarrhoea, transmission of spores between infected patients and healthy persons or surfaces is common [48,49]. Ingested spores also survive the degradative enzymes and low pH of the stomach, facilitating their passage into the lower gastrointestinal tract where they can germinate and initiate infection [48,49].
One step required for pathogenic spores to initiate an infection (once inside the host) is the transformation of spores into vegetative cells by a process called germination (Figure 2B) [50,51]. Therefore, spores must activate germination only when conditions are favourable for survival of the nascent vegetative cells. To that end, spores have evolved sensitive and specific receptors for sensing molecules present in permissive environments (such as the presence of small molecule nutrients), as well as cortex-digesting enzymes that facilitate spore activation [50-59]. The importance of germination receptors and cortex-lytic enzymes to virulence has been demonstrated in several species. The intricate molecular signalling that enables spores to sense and respond to environments has thus dispelled the notion of bacterial spores as inert entities. An elegant example is provided by B. anthracis, which has evolved to express virulence factors (i.e., toxins) soon after germination. Since germination occurs in host macrophages, toxin production is required for survival in the macrophage [38,39,41,42]. It may seem counterintuitive that spores would evolve to germinate inside phagocytes, but intracellular germination is advantageous since the host immune system can be evaded, allowing free bacterial reproduction. Once the macrophage is killed, the resulting bacterial escape can result in drastic clinical consequences manifesting in overwhelming toxemia and bacteremias [38,39,41,42,60]. Another example of germination playing a role in infection comes from C. difficile spores, which germinate specifically in response to bile salts and glycine present in a gut environment [50,52]. This disruption also provides a niche in which ingested C. difficile spores can reproduce and cause disease. In both these examples (B. anthracis and C. difficile), the spore fully germinates only in an environment that is conducive for the survival of the vegetative cells (either intracellular for B. anthracis or in the anaerobic environment of the gut for C. difficile). Furthermore, and in both cases, the spore responds to germinants that are uniquely present in either the macrophage or the gut to allow germination only in the right and permissive environment [50].
While many of these spore-associated virulence factors were identified in Bacillus spp., it is likely that clostridial spores also possess spore-specific factors to facilitate infection. Many spore-forming species such as C. botulinum are professional pathogens that can cause a specific type of disease (botulism), while others such as B. anthracis or C. difficile can cause a variety of disease manifestations [26-28]. In some cases, more than one species can cause the same or very similar disease (i.e., gas gangrene caused by C. perfringens and Clostridium sordellii). In others such as Clostridium septicum, underlying conditions such as immunodeficiency or cancer are a prerequisite to infection [20-28]. Despite the differences in disease presentation and outcome, infection primarily occurs when spores enter the body, colonize the host, germinate and produce the toxins (along with other virulence factors). In other cases, heat-stable toxins produced in contaminated food (most notably associated with B. cereus and C. botulinum) can cause food poisoning without a concurrent infection. Spore germination involves signalling from small-molecule germinants that diffuse across the outer spore layers and bind to receptors in the cytoplasmic (inner) membrane. The dormant spore takes up water, releases calcium ions, resumes metabolic activity and degrades the cortex to allow the emergence of the vegetative cell that in turn is capable to resume active growth and division (Figure 2B) [50,58,59].
Examples of bacterial spores as agents of mass destruction
In this section we will focus on the characteristics of four previously mentioned spore formers and the diseases that they produce. One of them, B. anthracis, is well recognized as a Class A microorganism by the CDC [1,2,60]. Other two spore-forming, C. perfringens and C. botulinum, are considered by the CDC as Class B and C agents, respectively, because of the potential use, in food and water contamination, of the deadly epsilon and botulism toxins produced by them, respectively [24,25]. The fourth spore-forming microorganism that we consider here is C. difficile, which although not listed by the CDC as a potential agent to be used in a bioterrorist event is considered a recently emerged superbug of public concern (see before). Accordingly with this interpretation, the NIAID catalogue C. difficile as a Class C priority emergen pathogen [61].
B. anthracis
This spore-forming bacterium is the cause of the disease called Anthrax [60,61]. B. anthracis is found naturally in soil samples spread over the entire planet, mainly in its sporulated form. Their spores are highly resistant to environmental, nutritional and chemical stresses (Figure 1). The bacterium contains a capsule that plays a key role in providing resistance of B. anthracis to phagocytosis [41,42]. Anthrax toxins consist of three proteins called protective antigen (PA), edema factor (EF) and lethal factor (LF) [60,61]. Natural Anthrax outbreaks occur on contact of the person with infected animals (cattle, sheep, horses and goats) or products derived therefrom (housings, hair and leather). Intestinal anthrax is due to the ingestion of contaminated undercooked or raw meat and is uncommon in the developed world. The symptoms of intestinal anthrax appear 2-5 days after ingestion of contaminated undercooked meat [60]. Bacteria are transported from the bowels to mesenteric and regional lymph nodes. Oral and oesophageal ulcers can occur
Regional lymphadenopathy and edema may rarely lead to airway compromise [41,60]. Lower intestinal disease includes lesions in the cecum and terminal ileum, haemorrhagic adenitis and occasionally massive ascites [60-62]. Nausea, vomiting, abdominal pain, hematemesis, hematochezia and sepsis are all presenting features. Early diagnosis is difficult and the mortality is high (Table 2). Another situation, different to intestinal anthrax, occurs with the entry of B. anthracis spores into exposed skin through cuts and abrasions to develop in cutaneous anthrax. Spores germinate in the tissue and vegetative cells quickly multiply and produce anthrax toxins resulting in local edema that would ends in a painless black eschar. The eschar normally heals in 1-3 weeks. An estimated 2,000 cases of cutaneous anthrax occur worldwide annually and result from entry of spores through skin abrasions. Of all cases of anthrax reported annually, 95% are cutaneous Anthrax and 4% are intestinal Anthrax. Of them in 20% of cases of cutaneous Anthrax and in 50% of cases of intestinal Anthrax, death of the infected patient occurs [12,62].
| Microorganism | Bacillus anthracis | Clostridium botulinum | Clostridium difficile | Clostridium perfringens | Coxiella burnetii |
|---|---|---|---|---|---|
| Infective form during aerolization | Spore | Spore | Spore | Spore | Small cell variant (SCV) and “pseudo spores” |
| Infectious aerolized dose | 5.0-10.0 spores (ID10%) | Not known | Not known | Not known | 1.0-3.0 SCV (ID50%) |
| Activation of the infective form | Spore germinant / co-germinant: L-amino acids, proteins, inosine (present in nucleic acids, foods and creams) | Spore germinant / co-germinant: L-amino acids, proteins, L-lactate (present in foods, creams), adenosine (present in nucleic acids) and CO2 | Spore germinant / co-germinant: CO2, biliar salts, L-aminoacids, proteins | Spore germinant / co-germinant: L-aminoacids, proteins, sugars (glucose and fructose), potassium, phosphate, CO2, inosine | Phagocytosis of the SCV form by macrophages and its conversion to LCV |
| Caused disease | Pneumonic and Intestinal Anthrax | Intestinal Botulism (similar to Infant Botulism) | Bloody Diarrhoea | Bloody Diarrhoea and Gas Gangrene | Q fever |
| Incubation period | 1 to 7 days | 1 to 7 days | 1 to 7 days | 1 to 7 days | 1 to 3 weeks |
| Symptoms after bioattack and agent activation | Inhalation of spores: Fever and chills, chest discomfort, shortness of breath, confusion or dizziness, coughing up blood, nausea, vomiting, or stomach pains, headache, sweats (often drenching), extreme tiredness, body aches Ingestion of spores: Fever and chills, swelling of neck or neck glands, sore throat, painful swallowing, hoarseness, nausea and vomiting, especially bloody vomiting, diarrhoea or bloody diarrhoea, headache, flushing (red face) and red eyes, stomach pain, fainting, swelling of abdomen (stomach) | Inhalation of spores: not known Ingestion of spores: Difficulty swallowing or speaking, dry mouth, facial weakness on both sides of the face, blurred or double vision, drooping eyelids, trouble breathing, nausea, vomiting and abdominal cramps, paralysis and life compromise if untreated | Inhalation of spores: not known Ingestion of spores: Watery diarrhoea, up to 15 times each day, severe abdominal pain, loss of appetite and loss weight, fever, patches of raw tissue that can bleed or produce pus (pseudomembranous colitis), kidney failure and death if untreated | Inhalation of spores: not known Ingestion of spores: a- Mild diarrhoea to a life-threatening sequence of severe abdominal pain, vomiting, bloody stool, ulceration of the small intestine with leakage (perforation) into the peritoneal cavity and possible death b- Gas gangrene (intestinal mionecrosis): breakdown of muscles, severe pain, oedema, tenderness and pallor, discoloration and hemorrhagic bullae and production of gas at the site of Wound. Life compromise | Inhalation /ingestion of SCV: High fever, severe headache, general malaise, myalgia, chills and/or sweats, cough, nausea, vomiting, diarrhea, abdominal pain, chest pain. It can developed in pneumonia, granulomatous hepatitis, myocarditis and central nervous system compromise |
| Dissemination | - Aerosol droplets - Contact with infected animals and infected people - Contact with contaminated objects or surfaces - Diarrhoea if the attack is combined with C. difficile and/or C. perfringens |
- Aerosol droplets - Contact with Contaminate objects or surfaces - Diarrhoea if the attack is combined with C. difficile and/or C. perfringens |
- Aerosol droplets - Transmission from person to person - Contact with contaminated surfaces - Diarrhoea |
-Aerosol droplets -Transmission from person to person - Contact with contaminated surfaces - Diarrhoea |
- Aerosol droplets -Transmission from person to person - Contact with contaminated surfaces - Diarrhoea if the attack is combined with C. difficile and/or C. perfringens |
| Contagious from person to person in case of aerosol dissemination | Yes | Not known but plausible if the attack is combined with C. perfringens and/or C. difficile | Yes | Yes | Yes |
| Treatment | Antibiotics, sporocides | Antitoxins, antibiotics and sporocides. Breathing machines (ventilators) in severe cases | Antibiotics, sporocides and / or surgery | Antibiotics, sporocides and / or surgery | Antibiotics, and / or surgery |
| Vaccine availability | Yes, but its efficacy against pulmonary anthrax is controversial | No | No | No | Yes, but its efficacy against a high inhaled dose of SCV is not known |
Table 2: Summary of the main infective properties of pathogenic Bacilli, Clostridia and Coxiella, the bioterrorist linked diseases would provoke and the treatments and preventive actions to be taken to ameliorate illness and deaths.
A less common naturally Anthrax is called inhalator or breathing Anthrax that occurs when a person inhales or breathes Anthrax spores present in the air particles (Table 2). This type of inhalator Anthrax occurs naturally in only 1% of all cases but leads to death of the patient in 90% of cases [60]. This is precisely the kind of Anthrax that a bioterrorist would choose to attack the population of a given city or region [1,2,26,62]. The United States Working Group on Civilian Biodefense [63] and CDC identify Anthrax as one of a limited number of biological agents capable of causing death and disease in sufficient numbers to cripple a developed region or urban setting [1,62-65]. Research into the use of Bacillus anthracis as a bioweapon is at least 100 years old and several nations are believed to have weaponised Anthrax [2,66-68]. The accidental release of aerosolized Anthrax spores from a military microbiology facility in 1979 at Sverdlovsk, of the former Soviet Union, caused at least 68 deaths and demonstrated the lethal potential of aerosolized B. anthracis [69]. A previous event happened during the years 1941 and 1942 when England, more precisely W. Churchill, fearing that Nazi Germany using weapons of mass destruction against the English people decided to develop their own biological weapons to be used in German territory as retaliation. The type of biological weapon developed by the British was aerolized Anthrax (i.e. highly concentrated spores of B. anthracis, packed in fine powders of no more than 5 microns in diameter). For this purpose a series of secret experiments were conducted and to determine the degree of success it was decided to test the secret weapon on the Scottish island of Gruinard which had previously been populated with lots of livestock, especially sheep. After releasing aerosols Anthrax on the island it was noticed that the experiment was very successful and the island was highly colonized by B. anthracis and therefore was unsafe for animals and humans [70]. This situation of high pollution of the island continued until the early 1980s when members of an environmental group travelled to the island clandestinely and “stole” land (still highly contaminated with B. anthracis spores). The environmental group sent letters containing the contaminated soil to several members of the British cabinet requiring decontamination Gruinard Island under threat of spreading greater amounts of land with Anthrax among members of the British government. This “threat-blackmail” produced the desired effect and the Government of His Majesty decontaminated the island flooding it with large amounts of formamide to inactivate and kill spores [71]. Today Gruinard Island can be accessed by anyone without risk of Anthrax and represents perhaps the first example of “bioterrorist attack” but with an “environmentalist” finale. Simulation studies conducted by the World Health Organization and the United States Congressional Office of Technology Assessment jointly with CDC staff and the Pentagon (before the attacks of 2001) led to the conclusion that beginning with the dispersal of 1 Kg of aerosolized B. anthracis spores, a form of lung Anthrax would developed after three months to cover all the US having produced within that time more than 100,000 dead and 3 million patients, as well as producing the collapse of the entire health system of the country as there is no in the US antibiotics enough to supply the entire population at risk of infection [1-3,62-64].
Twenty-two cases of bioterrorism-related Anthrax were identified in the United States during 2001 when tin-covered B. anthracis spores were delivered by mail letters of the US postal service [1-3,64-66]. There were 5 fatalities involving 11 cases of inhalational anthrax and 11 cases of cutaneous anthrax [1-3,64-66]. The mortality from untreated inhalational Anthrax approaches 100% and the costs associated with a real or perceived B.anthracis bioterrorist attack have been estimated at over $26 billion per 100,000 persons exposed [1-7,11-12]. For the three types of Anthrax the selected treatment is antibiotic therapy, the important thing is to discover the disease in its early stages. This is difficult to achieve in cases of inhalator Anthrax because aerosolized spores, that are between 2 and 5 μm in size, reach the alveolar ducts and alveoli [42,60]. Pulmonary macrophages ingest and transport the spores to mediastinal and hilar lymph nodes where germination and toxin production ensues. The toxins are released into the systemic circulation, resulting in edema, haemorrhage, necrosis, septic shock and death [60]. Spore germination in the mediastinum results in haemorrhagic mediastinitis, a hallmark of inhalational anthrax. During the first week symptoms are indistinguishable from those of a common cold but after that time spores already germinated in the lung alveoli, the emerging vegetative cells migrated to the lymph nodes and then invaded the blood to spread throughout the body. At this time appear the most characteristic symptoms in the ill person, bleeding and difficulty breathing (Table 2). The bacterial infection that could be originated by the inhalation of no more than ten spores has spread throughout the body being able to reach titles of 100 million bacteria per mille litre of blood, a fact that probably results all antibiotic therapy fruitless [72-74]. There are at least two types of vaccines, one with an attenuated strain and another cell-free vaccine. In both cases six doses distributed over 18 months are required [75]. These vaccines lose protective effect over time and it is uncertain its efficacy in cases of inhalatory Anthrax, especially in case of bioterrorist attacks wherein the doses of Anthrax spores inhaled would be several times higher than what could be found naturally in the air (Table 2). In a worse situation, B. anthracis strains used for the attack could be genetically modified to further increase their virulence and antibiotic resistance or combined with other bioterrorist agents, see below [31,32,35].
C. botulinum
Although bioterrorism-linked botulism outbreaks has been almost exclusively associated with food -and water- poisoning with the potent botulism toxin [24,76,77], we envision that an intentional release of aerosols containing spores of this pathogen might reach several of the objectives of a biological attack (illness and panic) [2-4,68] (Table 1). In fact, for surveillance purposes the DCD categorizes human botulism cases into four types: foodborne, wound, infant and other. While the first two types of human botulism are associated with the ingestion of the botulism toxin, the other two (infant and other botulisms) include botulism in which the route of contagious is unknown. In this sense, the “other” category of botulism includes the intestinal colonization by the bacterium with the in situ production of botulism toxin. Taking into consideration that in an intentional release (i.e. a bioterrorist attack), exposure may occur by routes in which the bio agent is not transmitted in nature, we think that C. botulinum gut colonization might occur in people that breaths aerosols containing spores of this pathogen.
Botulism is a rare (fewer than 200 cases of all forms of botulism are reported annually in the United States) but serious illness caused by the toxin (neurotoxin) produced by the vegetative form of C. botulinum after spore germination. All forms of botulism result from absorption of botulinum toxin into the circulation from either a mucosal surface (gut, lung) or a wound [78-80]. Botulinum toxin does not penetrate intact skin. Wound botulism and intestinal botulism result from production of botulinum toxin by C botulinum on tissue or in the intestinal lumen. A man-made form that results from aerosolized botulinum toxin or botulinum spores is inhalational botulism. Inhalational botulism has occurred accidentally in humans. All forms of human botulism display virtually identical neurologic signs that may be preceded by abdominal cramps, nausea, vomiting, or diarrhoea [78-80] (Table 2). The extent of paralysis may vary considerably among patients. Some patients may be mildly affected, while others maybe so paralyzed that they appear comatose and require months of ventilatory support. The rapidity of onset and the severity of paralysis depend on the amount of toxin produced and absorbed into the circulation. The toxin blocks excitatory synaptic transmission by inhibiting acetylcholine release causing flaccid paralysis at the neuromuscular junction [78-80]. Recovery in adults, may take weeks or months to complete. Patients with botulism typically present with difficulty seeing, speaking, and/or swallowing. In untreated persons, death results from airway obstruction (pharyngeal and upper airway muscle paralysis).
Although commonly botulism is considered intoxication and patients remain afebrile, it is also possible an infection produced by the replication of C. botulinum vegetative cells. Examples of C. botulinum infections are wound botulism (produced by the neurotoxin produced from a wound infected by C. botulinum) and infant botulism caused by consuming honey or powdered milk contaminated with spores of C. botulinum, which germinate and grow in the intestine with the releasing of the neurotoxin. In the case of a bioterrorist attack using aerosolized C. botulinum spores it might be predicted that C. botulinum, after spore germination, could produce an infection with release of the neurotoxin at mucosal sites (i.e. gastrointestinal tract) of injured persons (Table 2). Botulism can be treated with an antitoxin which blocks the action of the circulating toxin and in cases of C. botulism infections, as it might happen in case of a bioterrorist attack, antibiotics, antitoxins and sporocides will be required (Table 2) [24,81-85]. Although there are no reports on the use of C. botulinum spores in bioterrorism events, the spore dormancy makes spores harmless to anyone (a bioterrorist) handling them. Furthermore, the ease of handling spores in comparasión with manipulation of toxins makes spores as the ideal weapons to disseminate C. botulinum (Table 2).
Although in the last decades, the proportion of people with botulism who die has fallen from about 50% to less than 5% (www. cdc.gov/botulism), in the case of a hypothetical bioterrorist attack with aerosolized C. botulinum spores we predict that the medical and nursing care, the stocks of antitoxin, antibiotics and the breathing machines would rapidly turn insufficient and collapse. Besides an uncertain number of deaths in case of a bioterrorist attack with C. botulinum spores, the botulism survivors might require long time of supporting therapy because of the possibility of secondary infections acquired during the breathing therapy using machines and/or problems related to paralysis (Table 2).
C. difficile
Infections caused by this spore-forming bacterium belong to the group of infections called healthcare-associated infections (HAIs). C. difficile causes a spectrum of diseases ranging from diarrhoea to pseudomembranous colitis that would end in death [27,28]. C. difficile caused almost half million infections in the US in 2011, and almost 30,000 died within the first month of the infection [86,87]. In addition C. difficile infections are one of the most costly nosocomial infections, responsible for estimated 3 billion dollars in increased health care cost annually [27,28,86,87]. C. difficile spores spread rapidly because of the aerosols produced with the diarrhoea in addition to the resistance of the bacteria to many drugs used to treat microbial infections and that many of the disinfectants currently used in healthcare environments are inactive against C. difficile spores, mainly when spores are deposited on dirty surfaces [48]. In the present century, stronger strains of C. difficile emerged [88-91]. These strains are resistant to fluoroquinolone antibiotics, which are commonly used to treat clostridia and other infections. The ability to form spores and its acquired resistance to common antibiotics plus toxin overproduction turn C. difficile in a superbug of public concern which has spread throughout North America and Europe producing a 400% increase in deaths since 2000 to 2007 [87-91]. Because of the rapid spore-mediated spreading of C. difficile infections, the antibiotic resistance profile of virulent C. difficile strains and the robustness and persistence of C. difficile spores in the environment, we indicate that if C. difficile is manipulated (i.e. aerosolized) by the wrong hands it might represent, under its sporulated form to protect this anaerobic pathogen from air exposition, an ideal and novel agent of bioterrorist utilization that we must take into consideration (Table 2).
C. perfringens
This spore-forming bacterium can be found in almost any environment. It is able to produce at least thirteen different toxins [92- 96] and a similar number of virulent-associated factors [97-100]. It is considered the most widely distributed pathogen in nature [97]. Two diseases are commonly caused by C. perfringens: food poisoning and gas gangrene [98-100]. C. perfringens is one of the most common causes of foodborne illness in the US because of the production of a potent and sporulation-related enterotoxin named CPE [96-98]. It is estimated that it causes nearly a million cases of foodborne illness each year mainly diarrhoea and abdominal cramps [94-98]. Beef, poultry, gravies and other precooked foods are common sources for C. perfringens infections because they are prepared in large quantities and kept warm before consumed. C. perfringens spores germinate under these conditions and when they, or the newly-formed vegetative cells, start a new round of sporulation, the CPE is produced and release. People consuming this CPE-contaminated food get ill in a few hours [96-98]. A more life-threatening infection due to C. perfringens is gas gangrene, a highly lethal necrotizing soft tissue infection of skeletal muscle caused by toxins (mainly PLC-phospholipase and PFO-perfringolisin) and gas produced by this bacterium [95-97,100]. Clostridial gas gangrene produces the death of body tissues due to a lack of blood flow produced by the bacterial toxins and the concurrent consume of the destroyed tissue as a food-source for the same bacterium. Gas gangrene most commonly affects the extremities, but it can also occur in muscles and internal organs. The chances of developing gas gangrene are higher if underlying conditions that can damage blood vessels affect blood flow, such as diabetes or atherosclerosis [101]. The absence of early radical surgery, antibiotic therapy and (if available) hyperbaric treatment, leads to the spread of toxins in the body causing shock, coma and death [101]. The association of this anaerobic bacterium with a bioterrorist threat has been associated with the production of the epsilon toxin considered to be the third most powerful bacterial toxin [25,102]. However, this pathogen represents a substrate for the production of biological weapons. If aerosolized spores of C. perfringens were dispersed, they could potentially induce outbreaks of food poisoning and lead to increase morbidity of gas gangrene [103]. We envision that the intentional release of aerosols containing C. perfringens spores could permit that affected people inhale the spores that finally would end up in the intestinal tract.
Based on the profile of produced toxins, C. perfringens is classified in different types or toxi-types [95,96]. Type A C. perfringens isolates produce enterotoxin and alpha toxin, responsible for diarrhoea and gas gangrene, respectively, in humans. Type B and D strains usually infect animals (calves, piglets, sheep, lambs, goats, etc) but rarely humans but its use as an aerosolized weapon can change the situation. Type B and D isolates, in addition to alpha toxin, also produce epsilon toxin. Ingestion of epsilon toxin or viable spores would end up in pulmonary edema and neurologic dysfunction [96,102]. Therefore, C. perfringens may be weaponized either as purified epsilon toxin or as viable spores (Table 2). Although a high number of spores, 10,000-100,000 spores/g of contaminated food, are required to produce foodborne illness [94] it is not known the infectious dose for the development of a gas gangrene, diarrhoea or epsilon toxin intoxication in the case of utilization of aerosolized C. perfringens spores (Table 2). However, it might be predicted that the generalized panic that would happen if aerosolized spores responsible for gas gangrene production were disseminated among people would be similar to the prevailing chaos during the pandemic plague that ravaged Europe in the XIV-XVI centuries [4].
A special case: Coxiella burnetii and Q fever
Q fever is a worldwide disease caused by the Gram-negative bacteria Coxiella burnetii [29,104]. Farm animals (cattle, sheep and goats) are the primary reservoirs of C. burnetti that is excreted with the fluids (milk, urine and faeces) of infected animals [104,105]. The bacterium is also able to reach the amniotic fluids and colonize the placenta [29,106,107]. Why is this pathogen included in this revision? The reason is that C. burnetii produces very resistant cellular forms (named small cell variant, SCV) [30] that, without being as robust as the spores, are much more resistant and virulent (infectious dose of one SCV per person) than the vegetative forms of other dangerous bacteria such as the Class A bacterium Yersinia pestis, the causative agent of the Plague [108-110]. The SCV are extremely hardy and resistant to heat, high pressure, drying, osmotic treatment, UV light and many biocides. These properties allow C. burnetii to survive for very long periods in the environment where infection of humans happens by inhalation of SCV [29,108-110].
The fact that this bacterium is an obligate intracellular pathogen prevented for a long time the consideration of C. burnetii as a biological weapon of first choice. However, the development of genetic tools to improve its virulence and the formulation of a host cell free culture medium [111,112] that allowed the free reproduction of C. burnetii with formation of SCVs have placed this bacterium as very attractive for its use in the wrong hands as a biological weapon [29,108]. In humans, the disease may appear in two forms, acute or chronic. Acute Q fever may be asymptomatic or appear as atypical pneumonia or influenza-like illness [106-110]. When the immune system fails to control the acute phase, chronic Q fever emerges as hepatitis, endocarditis, osteomyelitis or aortic aneurisms (Table 2) [106,110]. C. burnetii is highly infectious by the aerosol route and can survive for long periods in the environment [29,105]. The cell cycle of C. burnetii includes the formation of the very infectious SCV of 0.2 to 0.5 μm in length and more pleomorphic large cell variants (LCVs) of more than 1 μm in length [30]. Different reports suggested that C. burnetii is also able to form spores from LCVs but this claim is controversial and is not currently considered because the physical-chemical properties of the SCVs (decreased metabolism, condense chromatin and thick wall) are sufficient to account for the extraordinary stability of the agent and its environmental transmission [29-30,108,110]. It is considered that a biological attack with aerolized SCVs of C. burnetii will affect a large number of persons because this pathogen has been shown to travel over large distances on the winds during natural outbreaks [107,113,114]. In addition, as indicated, its infectious dose for man is extremely low [29,108-110] (Table 2).
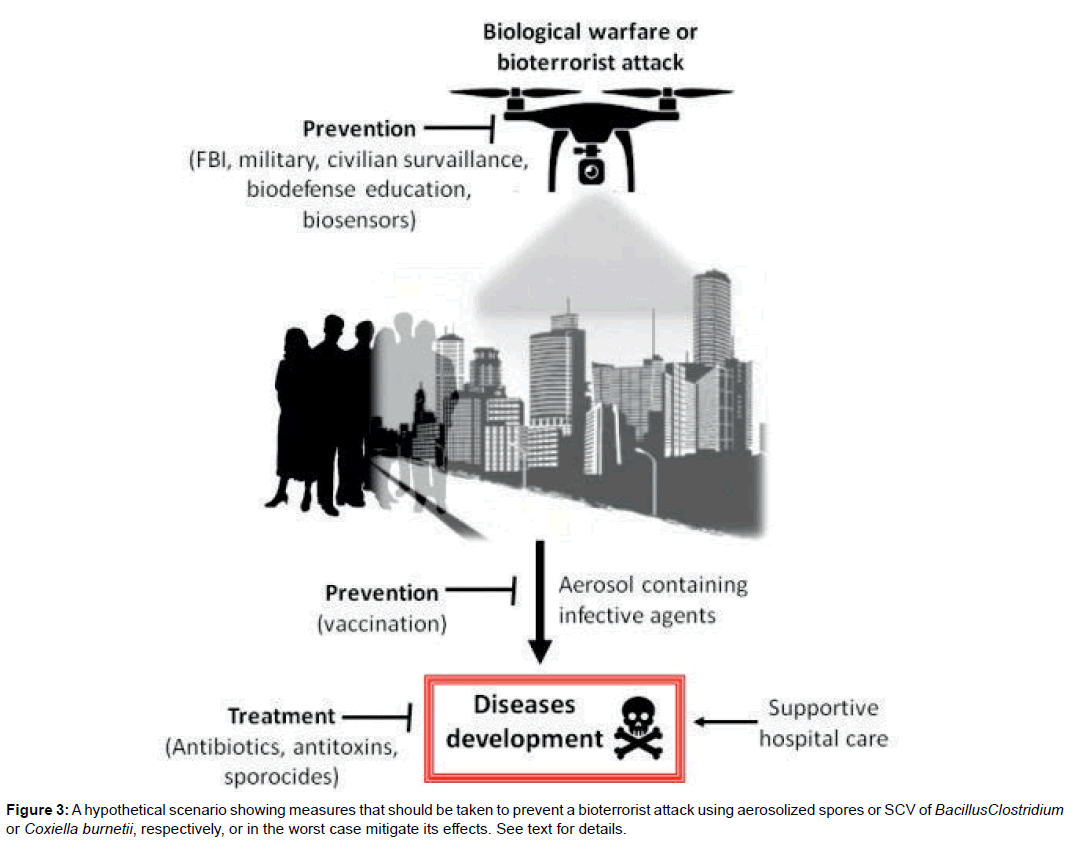
Conclusions
Each of the described pathogens (B. anthracis, C. botulinum, C. difficile, C. perfringens and C. burnetii) is relatively easy to grow in specific culture media to allow the production of high titres of the resistant forms: spores and SCVs for Bacilli-Clostridia and C. burnetii, respectively. High titles of each of these pathogens are feasible to obtain after incubation for 48 h to 96 h at a temperature not lower than 25°C and not higher than 37°C. The clostridia (C. botulinum, C. perfringens and C. difficile), because of their strict anaerobic growth characteristics, could become a little more difficult to grow than B. anthracis and Coxiella but a microbiology laboratory with trained staff should not have major problems in achieving growth and sporulation of Clostridium with high yields and rates of sporulation. In (Figure 3), we depict what would happens if a bioterrorist group would be able to grow and aerosolize the resistant forms (spores and SCVs) of the discussed pathogens at an average title of 4 x108 CFU/mL. The uniformity of the distribution of the aerosolized particles in the air will depend on various factors such as the intensity and direction of the prevailing wind at the time of the attack but we must also remember that while the primary intention of a bioterrorist event is to generate the highest proportion of sick people and possible deaths is also true that an objective of all bioterrorist event is to produce the biggest panic and fear as possible. As an example is enough to remember the panic generated not only in the US but worldwide with the use of B. anthracis spores to contaminate mail letters of the US postal service during October-November 2001 that “only” produced 22 cases of Anthrax and 5 fatalities.
How to react and how to prevent this sort of aggression against humankind? Two actions are essential: efficiency in the prevention and effectiveness in the response [9-10,115-118]. The several days incubation period of the disease produced by the microorganism used in the bioterrorist attack (Table 2) makes accurate diagnosis [115-117] and rapid treatment essentials to save as many lives as possible [8,12,118,119]. Prevention activities should involve areas of military and police intelligence, federal agencies like the FBI [7,9,11]. It is also very important to educate citizens on how to be prevented and how to act early to detect strange behaviours or activities out the ordinary [13,14]. Vaccination campaigns are very useful, especially to protect members of the military, police, civil defence and health care institutions that must act quickly and actively to heal the sick, prevent further deaths and mitigate the chaos and panic [11-12,75]. Adequate stocks and distribution capabilities of antibiotics and medicines are crucial to mitigate the post attack consequences. All these measures of prevention and response must be highly coordinated and must be periodically tested in simulated situations by professionals and by civilians [13,14]. These simulations would allow to know how rapidly a federal, state or local community recognize, respond and recover from a bioterrorist attack (Figure 3). Also important is the responsiveness of general citizens and therefore, education of citizens on how to react and what to do in case of a bioterrorist attack is very important. These programs focused on the general public would not increase their fear but inform and educate on how to manage the problem. Unfortunately, only US government and few other countries face the bioterrorist scenario as a real threat. Finally, scientists have a crucial role [31,32,66] in the development of improved technology [34,35,68] for the early detection of a bio threat (e.g. real-time biosensors) [116-117], effective vaccines [75,120,121] against aerosols containing high amounts of pathogens (e.g. mucosal vaccines), new medicines [119,122-128] and biocides and sporocides [85] working on biotic and dirty surfaces.
References
- Webb GF (2003) A silent bomb: the risk of anthrax as a weapon of mass destruction.Proc Natl Acad Sci USA 100: 4355-4356.
- Arun Kumar R, Nishanth T, Ravi Teja Y, Sathish Kumar D (2011) Bio threats bacterial warfare agents. J Bioterr Biodef 2:1-5.
- Hugh-Jones ME, Rosenberg BH, Jacobsen S (2011) The 2001 Attack anthrax: key observations. J Bioterr Biodef 1: 1-10.
- Simon JD (2011) Why the bioterrorism skeptics are wrong. J Bioterr Biodef 2: 1-3.
- Kuhlman MR (2012) Letter to the editor in response to the 2001 attack anthrax: key observations, by ME Hugh-Jones, BH Rosenberg, and S Jacobsen, Journal of Bioterrorism & Biodefense S3:001. J Bioterr Biodef 3: 1-2.
- Siegrist DW (2005) Cost-effectiveness of biological weapons. Encyclopedia of Bioterrorism, Wiley Online Library.
- Braithwaite RS, Fridsma D, Roberts MS (2006) The cost effectiveness of strategies to reduce mortality from an intentional release of aerosolized anthrax spores. Med Decis Making 26:182-193.
- https://www.reachingcriticalwill.org/resources/fact-sheets/critical-issues/4579- biological-weapons.
- Hamburg MA (2002) Bioterrorism: responding to an emerging threat. Trends Biotech 20: 296-298.
- St John R, Finlay B, Blair C (2001) Bioterrorism in canada: an economic assessment of prevention and postattack response. Can J Infect Dis 12: 275-284.
- Schneider H (2005) Protecting public health in the age of bioterrorism surveillance: is the price right? J Environ Health 68: 9-13.
- Center for disease control and prevention (2000) Surveillance for adverse eventsassociated with anthrax vaccination. US Department of defense Morb Mortal WklyRep 49: 341-345.
- Inglesby TV, O’Toole T, Henderson DA (2000) Preventing the use of biologicalweapons: improving response should prevention fail. Clin Infect Dis 30: 926-929.
- Ziskin LZ and Harris DA (2007) State health police for terrorism preparedness.Amer J Pub Health 97(9).
- Gorbushina AA (2012) Life in Darwin’s dust; intercontinental transport andsurvival of microbes in the nineteenth century. Environ Microbiol 9: 2911-2922.
- Leitenberg M (2004) The problem of biological weapons. The Swedish Nat DefColl pp. 27-29.
- U.S. Congress (1999) Office of technology assessment, proliferation of weaponsof mass destruction assessing the risks OTA-ISC-559 Washington DC U.S.Government Printing Office.
- Piggot PJ, Hilbert, DW (2004) Sporulation of bacillus subtilis. Current Opinion inMicrobiology 7:579-586.
- Al-Hinai MA, Jones SW, Papoutsakis ET (2015) The clostridium sporulationprograms: diversity and preservation of endospore differentiation. Microbiol MolBiol Rev.
- Mallozzi M (2010) Spore-forming bacilli and clostridia in human disease. Future Microbiol 5:1109-1123.
- Russell AD (1999) Bacterial resistance to disinfectants: present knowledge andfuture problems. J Hosp Infect 43: S57-S68.
- Setlow P (2006) Spores of bacillus subtilis: their resistance to and killing byradiation, heat and chemicals. Journal of Applied Microbiology 101: 514-525.
- Leggett MJ, McDonnell G, Denyer SP, Setlow P, Maillard JY (2012)Bacterial spore structures and their protective role in biocide resistance. J ApplMicrobiol 113: 485-498.
- Centres for Disease Control and Prevention (2012). National botulism surveillancesystem overview. atlanta georgia: US Department of Health and HumanServices CDC.
- Gaur K, Iyer K, Pola S, Gupta R, Gadipelli AK, et al. (2014) The clostridiumperfringens epsilon toxin as a bioterrorism weapon. J Microb Biochem TechnolS8: 009.
- https://www.cdc.gov/anthrax/bioterrorism/index.html
- Wilcox MH (2003) Clostridium difficile infection and pseudomembranous colitis.Best Pract & Res Clin Gastroenterology 17: 475–493.
- Gerding DN (2008) Treatment of clostridium difficile infection. Clin InfectDis 46: S32–S42.
- Oyston PC, Davies C (2011) Q fever: the neglected biothreat agent. J MedMicrobiol 1:9-21.
- MC Caul TF, Williams JC (1981) Developmental cycle of Coxiella burnetii: structure and morphogenesis of vegetative and sporogenic differentiations. JBacteriol 147:1063-1076.
- Fraser CM, Dando MR (2001) Genomics and future biological weapons: The needfor preventive action by the biomedical community. Nat Genet 29:253-256.
- Epstein GL (2001) Controlling biological warfare threats: resolving potentialtensions among the research community industry and the national securitycommunity. Crit Rev Microbiol 27:321-354.
- Cello J, Paul AV, Wimmer E (2002) Chemical synthesis of poliovirus cDNA:Generation of infectious virus in the absence of natural template. Science 297:1016-1018.
- Petro JB, Plasse TR, McNulty JA (2003) Biotechnology: Impact on biologicalwarfare and biodefense. biosecurity and bioterrorism: biodefense strategypractice and science.
- Epstein GL (2012) Preventing biological weapon development through thegovernance of life science research. biosecurity and bioterrorism: biodefensestrategy practice and science.
- Setlow P (2001) Resistance of spores of bacillus species to ultraviolet light. EnvironMol Mutagen 38: 97-104
- Setlow P (2007) I will survive: DNA protection in bacterial spores. TrendsMicrobiol 15: 172-180.
- Weaver J (2007) Protective role of bacillus anthracis exosporium inmacrophage-mediated killing by nitric oxide. Infect Immun 75:3894-3901.
- Stewart GC (2015) The exosporium layer of bacterial spores: a connection to theenvironment and the infected host.
- Calfee MW, Choi Y, Rogers J, Kelly T, Willenberg Z, et al. (2011) Lab scaleassessment to support remediation of outdoor surfaces contaminated withbacillus anthracis spores J Bioterr Biodef 2: 1-8
- Cote CK, Welkos SL (2015) Anthrax toxins in context of bacillus anthracisspores and spore germination. Toxins7:3167-3178.
- Guidi-Rontani C (2002) The alveolar macrophage: the trojan horse of bacillusanthracis. Trends Microbiol 10: 405-409.
- Oliva CR, Swiecki MK, Griguer CE, Lisanby MW, Bullard DC, et al. (2008) The integrin Mac-1 (CR3) mediates internalization and directsBacillus anthracis spores into professional phagocytes. PNAS 105: 1261-1266.
- Guillemet E, Cadot C, Seav-LyT, Guinebretiére MH, Lereclus D, et al.(2010) The InhA metallo proteases of bacillus cereus contribute concomitantly tovirulence. J Bacteriol 192:286-294.
- Drinks A (1999) Bacillus subtilis spore coat. Microbiol Mol Biol Rev 63: 1.
- Popham DL (2002) Specialised peptidoglycan of the bacterial endospore: the innerwall of the lockbox. Cell Mol Life Sci 59: 426-433.
- Henriques AO (1998) Involvement of superoxide dismutase in spore coatassembly in bacillus subtilis. J Bacteriol 180: 2285-2291.
- Wilcox MH, Fraise AP, Bradley CR, Walker J, Finch RG (2011)Sporicides for clostridium difficile: the devil is in the detail. J Hosp Infect 77: 187-188.
- Paredes-Sabja D (2014) Clostridium difficile spore biology: sporulationgermination and spore structural proteins. Trends in Microbiology.
- Paredes-Sabja D (2011) Germination of spores of bacillales and clostridialesspecies: mechanisms and proteins involved. Trends in Microbiology 19:85-94.
- Setlow P (2003) Spore germination. Curr Opin Microbiol 6: 550-556.
- Sorg JA (2008) Bile salts and glycine as co-germinants for clostridium difficilespores. J Bacteriol 190: 2505-2512.
- Paredes-Sabja D (2009) SleC is essential for cortex peptidoglycan hydrolysisduring germination of spores of the pathogenic bacterium clostridium perfringens.J Bacteriol191: 2711-2720.
- Heffron JD (2009) Roles of germination-specific lytic enzymes CwlJ and SleBin bacillus anthracis. J Bacteriol 191: 2237-2247.
- Carr KA (2010) The role of bacillus anthracis germinant receptors in germination and virulence. Mol Microbiol75: 365-375.
- van der Voort M, García D, Moezelaar R, Abee T (2010)Germinant receptor diversity and germination responses of four strains ofthe bacillus cereus group. Int J Food Microbiol 139:108-115.
- Abee T, Groot MN, Tempelaars M, Zwietering M, Moezelaar R, et al. (2011)Germination and outgrowth of spores of bacillus cereus group members: diversityand role of germinant receptors. Food Microbiol 28:199-208.
- Setlow P (2013) Summer meeting 2013 when the sleepers wake: the germinationof spores of Bacillus species. J Appl Microbiol 115:1251-1268.
- Setlow P (2014) Germination of spores of bacillus species: what we know and donot know. J Bacteriol 196:1297-1305.
- Watson A, Keir D (1994) Information on which to base assessments of risk fromenvironments contaminated with anthrax spores. Epidemiol Infect 113: 479-490.
- Inglesby TV, O’Toole T, Henderson DA (2002) Anthrax as a biologicalweapon. JAMA 287: 2236-2252.
- Fowler RA, Shafazand S (2011) Anthrax Bioterrorism: prevention diagnosis andmanagement strategies. J Bioterr Biodef 2: 1-5.
- Center for Civilian Biodefense Studies, Johns Hopkins University Schools ofMedicine, Baltimore, MD 21202, USA.
- Wein LM, Craft DL, Kaplan EH (2003) Emergency response to an anthrax attack. Proc Natl Acad Sci USA 100: 4346-4351.
- Dudley JP (2005) Review and analysis of reported anthrax related military mailsecurity incidents in washington DC metropolitan area during march. JBioterr Biodef pp: 1-6.
- Hugh-Jones ME, Rosenberg BH, Jacobsen S (2012) Evidence for the source of the2001 attack anthrax. J Bioterr Biodef 3: 1-8.
- Unal B, Aglani S (2016) Use of chemical biological radiological and nuclearweapons by non-state actors. Lloyd’s emerging risk report Chatham House TheRoyal Institute of International Affairs.
- Herdman R (1993) US Congress, office of technology assessment proliferation of weapons of mass destruction, assessing the risk OTA ISC 559Washington DC US government printing office.
- Meselson M, Hugh-Jones M, Langmuir A, Popova I, Shelokov A, et al.(1994) The sverdlovsk anthrax outbreak of 1979. Science 266: 1202-1208.
- Manchee RJ, Broster MG, Melling J, Henstridge RM, Stagg AJ (1981) Bacillusanthracis on Gruinard island. Nature 294:254-255.
- Manchee RJ, Broster MG, Stagg AJ, Hibbs SE (1994) Formaldehyde solutioneffectively inactivates spores of bacillus anthracis on the scottish island of gruinar.Appl Environm Microbiol 60:4167-4171.
- Glassman HN (1966) Discussion (industrial inhalation anthrax). Bacteriol Rev30:657-659.
- Peters CJ, Hartley DM (2002) Anthrax inhalation and lethal human infection.Lancet 359: 710-711.
- Fennelly KP, Davidow AL, Miller SL, Connell N, Ellner JJ (2004) Airborneinfection with bacillus anthracis from mills to mail. Emerg Infect Dis.
- Chen S, Zeng M (2012) Anthrax bioterrorism and current vaccines. J Bioterr Biodef 4: 1–5.
- Wein LM, Liu Y (2005) Analyzing a bioterror attack on the food supply: The caseof botulinum toxin in milk. PNAS 102: 9984-9989.
- Liu Y, Wein LM (2008) Mathematically assessing the consequence of foodterrorism scenarios. J Food Sci. 73: M346-M353.
- Dezfulian M, Dowell Jr VR (1980) Cultural and physiological characteristics andantimicrobial suspectibility of Clostridium botulinum isolates from foodborne andinfant botulism cases. Journal of Clinical Microbiology 11: 604-609.
- Davis LE (1993) Botulinum toxin: from poison to medicine. Western Journal of Medicine 158: 25-29.
- Sobel J (2005) Botulism. Clinical Infectious Diseases 41: 1167-1173.
- Arnon SS, Schechter R, Maslanka SE, Jewell NP, Hatheway CL (2006) Humanbotulism immune globulin for the treatment of infant botulism. N Engl J Med 354:462-471
- Arnon SS, Barzilay EJ (2009) Clostridial infections: Botulism and infant botulism.In: Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. The Red Book: report ofthe Committee on Infectious Diseases. Elk Grove Village: American Academy of Paediatrics 259-62.
- CDC (2010) Investigational heptavalent botulinum antitoxin (HBAT) to replacelicensed antitoxin AB and investigational botulinum antitoxin E. MMWR 59:299.
- Fraise A (2011) Currently available sporicides for use in healthcare and their limitations. J Hosp Infect 77: 210-212.
- Humphreys PN (2011) Testing standards for sporicides. J Hosp Infect 77: 193-98.
- Dubberke ER, Wertheimer AI (2009) Review of current literature on the economicburden of Clostridium difficile infection. Infect Control Hosp Epidemiol 30: 57-66.
- Banaei N, Anikst V, Schroeder LF (2015) Burden of clostridium difficile infectionin the United States. New Engl J Med 372: 2368-2370.
- Coia JE (2009) What is the role of antimicrobial resistance in the new epidemic ofclostridium difficile? Int J Antim Agents 33(suppl. 1): S9-S12.
- Loo VG, Poirier L, Miller MA (2005) A predominantly clonalmultiinstitutional outbreak of clostridium difficileassociated diarrhoea with highmorbidity and mortality. N Engl J Med 353: 2442-2449.
- Warny M, Pepin J, Fang A, Killgore G, Thompson A, et al. (2005) Toxin production by an emerging strain of clostridium difficileassociated with outbreaks of severe disease in North America and Europe. Lancet366: 1079-84.
- Goorhuis A, Bakker D, Corver J, Debast SB, Harmanus C, et al. (2008) Emergence ofclostridium difficileinfection due to a new hyper virulent strain polymerase chain reaction ribotype. ClinInfect Dis 47: 1162–1170.
- Dubberke E (2012) Clostridium difficile infection: the scope of the problem. J HospMed Suppl 3:S1-4.
- Jones AM, Kuijper EJ, Wilcox MH (2013) Clostridium difficile: a europeanperspective. J Infec 2013 66: 115-28.
- Lund BM (1990) Foodborne disease due to bacillus and clostridium species.Lancet 336: 982-986.
- McDonel JL (1980) Clostridium perfringens toxins (type A, B, C, D, E). PharmacolTher 10: 617-655.
- Popoff M, Bouvet P (2009) Clostridial toxins. Future Microbiol 4: 1021-1064.
- Shimizu T, Ohtani K, Hirakawa H, Ohshima K, Yamashita A, et al. (2002)Complete genome sequence of clostridium perfringens, an anaerobic flesheater.PNAS 99: 996-1001.
- Philippe V, Méndez M, Huang I, Orsaria L, Sarker M, et al. (2006) Inorganicphosphate induces spore development and enterotoxin production in the intestinalpathogen clostridium perfringens. Infection and Immunity 74: 3651-3656.
- Méndez M, Huang I, Ohtani K, Grau R, Shimizu T, et al. (2008) Carboncatabolite repression of Type IV pilus-dependent gliding motility in the anaerobicpathogen clostridium perfringens. Journal of Bacteriology 190: 48-60.
- Méndez M, Goñi A, Ramirez W, Grau R (2011) Sugar inhibits theproduction of the toxins that trigger clostridial gas gangrene. MicrobialPathogenesis 52:85-91.
- YangZ, Hu J, Qu Y, Sun F, Leng X, et al (2015)Interventions for treating gas gangrene. Cochrane Wounds editorial Group
- Payne D (1997) The clostridium perfringens epsilon toxin. Rev MedMicrobiol S28-S30.
- Omernik A, Plusa T (2015) Toxins of clostridium perfringens as a naturaland bioterroristic threats. Pol Merkur Lekarski 39: 149-152.
- Bielawska-Drózd A, Cieslik P, Mirski T, Bartoszcze M, Knap J, et al. (2013) Q fever selected issues Annals Agri Environl Med 20: 222-232.
- Speelman R (2010) The largest Q fever outbreak ever reported. Neth J Med68: 380-381.
- van der Hoek W, Dijkstra F, Schimmer B, Schneeberger PM, Vellema P,et al. (2010) Q fever in theNetherlands: an update on the epidemiology and control measures. Euro Surveill 15: 19520.
- Welsh HH, Lennette EH, Abinanti FR, Winn JF (1958) Air-bornetransmission of Q fever: the role of parturition in the generation of infectiveaerosols. Ann N Y Acad Sci 70: 528-540.
- Madariaga MG, Rezai K, Trenholme GM, Weinstein RA (2003) Q fever: abiological weapon in your backyard. Lancet Infect Dis 3: 709-721.
- Russell JB, Kretzschmar MEE, Mutters NT, Teunis PFM (2013) Humandose response relation for airborne exposure to Coxiella burneti. BMC Infec Dis13:488
- Russel JB, Mutters NT, Péter O, Kretzschmar MEE, Teunis PFM (2015)Exposure to low doses of coxiella burnetii caused high illness attack rates: insightsfrom combining human challenge and outbreak data. Epidemics 11:1-6.
- Omsland A, Cockrell DC, Howe D, Fischer ER, Virtaneva K, et al. (2009)Host cell free growth of the Q fever bacterium coxiella burnetii. Proc Natl AcadSci 106: 4430-4434.
- Omsland A, Hackstadt T, Heinzen RA (2013) Bringing culture to theuncultured: coxiella burnetii and lessons for obligate intracellular bacterialpathogens. PLoS Pathog 9: e1003540.
- O’Connor BA, Tribe IG, Givney R (2015) A windy day in a sheep saleyard:an outbreak of Q fever in rural South Australia. Epidemiol Inf 143: 391-398.
- Schack M, Sachse S, Rödel J, Frangoulidis D, Pletz MW, et al. (2014) Coxiella burnetii (Q fever) as a cause of communityacquiredpneumonia during the warm season in Germany. Epidemiol Inf 142: 1905-1910.
- Robinson-Dunn B (2002) The microbiology laboratory’s role in response tobioterrorism. Arch Pathol Lab Med 126: 291-294
- Jones SW, Dobson ME, Francesconi SC, Schoske R, Crawford R (2005)DNA assays for detection identification and individualization of select agentmicroorganisms. Croat Med J 46: 522-529.
- Zasada AA, Gierczynski R, Rzeczkowska M, Forminska K, Zacharczuk K,et al. (2011) Detection and identification of highly pathogenic within theframework of the EQADeBa project part I: samples containing living pathogens. Przeql Epidemiol 65: 401-407.
- Turingan RS, Thomann HU, Zolotova A, Tan E, Selden RF (2013) Rapidfocused sequencing: a multiplexed assay for simultaneous detection and straintyping of bacillus anthracis francisella tularensis and yersinia pestis. PLoS Onee56093.
- Froude JW, Stiles B, Pelat T, Thullier P (2011) Antibodies for biodefensemAbs 3: 1-11.
- Smith LA (2009) Botulism and vaccines for its prevention vaccine 27: D33-D39.
- Friedlander AM, Little SF (2009) Advances in the development of nextgenerationanthrax vaccines Vaccine 27: D28-D32.
- Popov SG, Popova TG, Hopkins S (2005) Effective anti-proteaseantibiotictreatment of experimental anthrax BMC Infect Dis 5: 25.
- Shoop WL, Xiong Y, Wiltsie J (2005) Anthrax lethal factor inhibitionPNAS 102: 7958-7963.
- Alvarez Z, Abel-Santos E (2007) Potential use of inhibitors of bacteria sporegermination in the prophylactic treatment of anthrax and clostridium difficileassociateddisease. Expert Rev Anti Infect Ther 5: 783-792.
- McKevitt MT, Bryant KM, Shakir SM (2007) Effects of endogenousD alanine synthesis and autoinhibition of bacillus anthracis germination on in vitroand in vivo infections Infect Immu 75: 5726-5734.
- Cegelski L, Marshall GR, Eldridge GR (2008) The biology and futureprospects of antivirulence therapies. Nat Rev Microbiol 6: 17-27.
- Roxas Duncan V, Enyedy I, Montgomery VA (2009) Identification andbiochemical characterization of small molecule inhibitors of clostridium botulinumneurotoxin serotype E. Antim Agents Chemother 53: 3478-3486.
- Oie S, Obayashi A, Yamasaki H, Furukawa H, Kenri T, et al.(2011) Disinfection methods for spores of bacillus atrophaeus,b. anthracis, clostridium tetani, c. botulinum and c. difficile. Biol PharmBull 34:1325-1329.
Relevant Topics
- Anthrax Bioterrorism
- Bio surveilliance
- Biodefense
- Biohazards
- Biological Preparedness
- Biological Warfare
- Biological weapons
- Biorisk
- Bioterrorism
- Bioterrorism Agents
- Biothreat Agents
- Disease surveillance
- Emerging infectious disease
- Epidemiology of Breast Cancer
- Information Security
- Mass Prophylaxis
- Nuclear Terrorism
- Probabilistic risk assessment
- United States biological defense program
- Vaccines
Recommended Journals
Article Tools
Article Usage
- Total views: 23889
- [From(publication date):
March-2016 - Jul 16, 2025] - Breakdown by view type
- HTML page views : 22552
- PDF downloads : 1337