Axillary Lymph Node Metastases on the Contralateral Side in Primary Breast Cancer Development
Received: 25-Jul-2022 / Manuscript No. bccr-22-72169 / Editor assigned: 27-Jul-2022 / PreQC No. bccr-22-72169 / Reviewed: 10-Aug-2022 / QC No. bccr-22-72169 / Revised: 15-Aug-2022 / Manuscript No. bccr-22-72169 / Accepted Date: 20-Aug-2022 / Published Date: 22-Aug-2022 DOI: 10.4172/2572-4118.1000167
Abstract
A 71-year-elderly person visited our emergency clinic in the wake of seeing a mass in her right bosom. A mass of 5 cm in measurement with skin penetration was discernible on the average side of the right bosom. She went through a needle biopsy and was determined to have obtrusive ductal carcinoma. On different imaging modalities, there were no far off metastases except for reciprocal axillary lymph hub metastases were found. She went through preoperative chemotherapy and showed a clinical fractional reaction. After careful conversation, she decided on a medical procedure and went through incomplete mastectomy of the right bosom and two-sided axillary lymph hub analyzation. Histopathological assessment uncovered remaining bosom growth and one metastatic axillary lymph hub on each side. Postoperative radiotherapy and chemical treatment were performed. The patient is alive and repeat free starting around 1 year after the beginning of treatment.
Keywords
Breast cancer; Contralateral axillary lymph node metastasis; Locoregional extension
Introduction
The spread of sentinel lymph hub biopsy for clinically hub negative bosom disease has prompted sensational advances in how we might interpret the lymphatics of the bosom [1]. Most lymph streams into the ipsilateral axillary lymph hubs, however a few streams into the supraclavicular, cervical, and inward thoracic lymph hubs. Stream to the contralateral axillary lymph hubs [1] can happen yet is incredibly interesting. Contralateral axillary lymph hub metastasis (CAM) is uncommon in bosom disease patients. CAM has expectedly been viewed as far off metastasis and has in this way been treated with foundational treatment. CAM can be partitioned into simultaneous CAM at the analysis of essential bosom malignant growth [2] and metachronous CAM at repeat after therapy for bosom disease. In past reports, most instances of CAM are metachronous and few are simultaneous. Most announced instances of CAM are because of repeat following bosom a medical procedure or axillary medical procedure. Here we report an instance of a 71-year-elderly person with genuine essential bosom malignant growth who had CAM and ipsilateral axillary lymph hub metastasis.
Case presentation
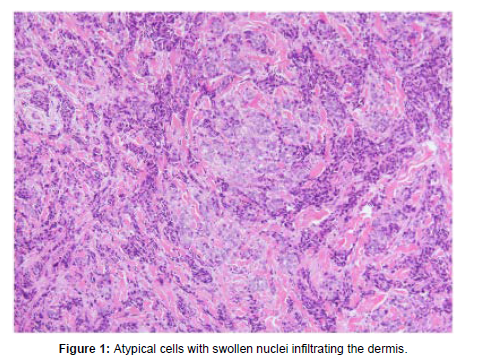
A 71-year-old postmenopausal lady visited our bosom facility subsequent to seeing a mass in the upper average quadrant of her right bosom. A mass of 5 cm in measurement with skin penetration was tangible in the right bosom. Bosom ultrasound affirmed a 5-cm width mass in the right bosom, and axillary ultrasound uncovered different extended lymph hubs with a most extreme measurement of 3 cm on both the ipsilateral and contralateral sides. Ultrasound-directed center needle biopsy was performed on the mass of the right bosom [3]. Histopathological assessment uncovered obtrusive ductal carcinoma with Grade 3 atomic atypia. The growth was estrogen receptor-positive, progesterone receptor-negative, and HER2-negative. Contrastupgraded CT showed the mass in the right bosom with skin penetration and the amplified two-sided axillary lymph hubs, however no far off metastases to different organs. The left finish of the growth had attacked the contralateral bosom. Bone scintigraphy showed no bone metastases [4]. The preoperative conclusion was cT4bN1M1 (LYM) (Figure 1). The patient was treated with chemotherapy comprising of 4 patterns of epirubicin and cyclophosphamide at regular intervals followed by 4 patterns [5] of docetaxel like clockwork. She showed a clinical fractional reaction. After careful conversation, the patient selected fractional mastectomy of the right bosom and two-sided axillary lymph hub analyzation. The postoperative course was good.
Histopathological assessment uncovered that the cancer in the right bosom was obtrusive lobular carcinoma with a measurement of 4.2 cm. Lymphatic attack (LVI) was positive. The histological restorative impact was Grade 2a. Altogether, 15 lymph hubs were eliminated from the right axilla and 10 from the left axilla. There was 1 metastatic hub on each side, which estimated 6 mm and 2 mm, separately. After medical procedure, she got nearby radiation treatment [6] to the excess right bosom out portion of 60 Gy in day to day parts of 2 Gy. The supraclavicular and parasternal lymph hub regions were additionally remembered for the radiation field. Subsequent to talking about the dangers and advantages of adjuvant chemical treatment, she was begun on letrozole. The patient is alive without repeat starting around 1 year after the beginning of this multimodal treatment.
Discussion
Lymphatic scintigraphy has decisively progressed how we might interpret the lymphatics of the bosom. Essential lymphatic waste of the bosom is to the ipsilateral axillary lymph hubs, however seepage to different locales, for example, the supraclavicular or interior mammary lymph hubs can happen in up to 30% of ladies [7]. Lizarraga et al. revealed that lymphatic stream to the contralateral axillary lymph hubs happens in just 0.3% of ladies. Pasta et al. noticed lymphatic waste [8] to the contralateral axilla in 2.8% of ladies who had recently gone through bosom malignant growth medical procedure. Utilizing various tracers to inspect other potential courses, Haagensen showed the way that cancer cells could spread to the contralateral axillary lymph hubs by entering the profound lymphatic plexus of the chest wall. Taken together, these past investigations demonstrate [9] the way that lymph can stream to the contralateral axilla. Consequently, CAM can happen contingent upon the site of the growth and the life systems of the patient. In our patient, we guess that the lymphatic stream was coordinated contralaterally on the grounds that the growth was situated in the average piece of the right bosom.
Debate stays with respect to whether CAM ought to be viewed as far off metastasis or neighborhood spread. Assuming CAM is available at the underlying analysis, being the consequence of foundational spread is expectedly thought. CAM is excluded from the ongoing adaptation of the AJCC Cancer Staging Manual [10] however was recently named far off metastasis. In Japan too, CAM is viewed as far off metastasis however isn’t obviously depicted in rules. As referenced above, it stays an open inquiry whether CAM ought to be viewed as far off metastasis or neighborhood spread. In any case, lately, there have been a reports where CAM without far off metastasis to different organs was treated with the point of revolutionary fix. A large number of those reports don’t depict CAM with regards to far off metastasis [11]. However, regardless of whether CAM isn’t viewed as far off metastasis, the lymph hub stage would then be N3, which is as yet high level illness, and unfortunate visualization would be normal. Be that as it may, great anticipation has been accounted for at times. To keep away from a weakness to patients, particularly those with essential bosom malignant growth, CAM without far off metastasis to different organs ought to be treated with healing expectation.
Conclusion
We revealed an uncommon instance of coordinated CAM from essential bosom disease in a 71-year-elderly person. This case proposes that CAM without far off metastasis to different organs ought to be treated with healing plan to stay away from a burden to the patient.
Acknowledgement
The authors are grateful to the Centre Hospitalier Régional Universitaire de Tours, for providing the resources to do the research on breast cancer.
Conflicts of Interest
The authors declared no potential conflict of interest for the research, authorship, and/or publication of this article.
References
- Gingerich J,Kapenhas E,Morgani J,Heimann A (2017) Contralateral axillary lymph node metastasis in second primary breast cancer: case report and review of the literature. Int J Surg Case Rep40: 47-49.
- Agha RA,Franchi T,Sohrabi C,Mathew G,Kerwan A (2020) The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg84: 226-230.
- Lizarraga IM,Scott-Conner CEH,Muzahir S,Weigel RJ,Graham MM,et al. (2013) Management of contralateral axillary sentinel lymph nodes detected on lymphoscintigraphy for breast cancer. Ann Surg Oncol 20: 3317-3322.
- Morcos B,Jaradat I,El-Ghanem M (2011) Characteristics of and therapeutic options for contralateral axillary lymph node metastasis in breast cancer. Eur J Surg Oncol 37: 418-421.
- Huston TL,Pressman PI,Moore A,Vahdat L,Hoda SA, et al. (2007) The presentation of contralateral axillary lymph node metastasis from breast carcinoma: a clinical management dilemma. Breast J13: 158-164.
- Strazzanti A,Gangi S,Trovato C,Pacini N,Basile F (2018) Contralateral lymph node metastasis in a woman with new primary breast cancer: systemic disease or locoregional diffusion? Int J Surg Case Rep53: 400-402.
- Namkoong H,Kurashima A,Morimoto K, Hoshino Y, Hasegawa N, et al. (2016) Epidemiology of pulmonary nontuberuculous mycobacterial disease Japan. Emerg Infect Dis22: 1116-1117.
- Griffith DE,Girard WM,WallaceJr RJ (1993) Clinical features of pulmonary disease caused by rapidly growing mycobacteria. An analysis of 154 patients. Am Rev Respir Dis147: 1271-1278.
- Petrini B (2006) Mycobacterium abscessus: an emerging rapid-growing potential pathogen. APMIS114: 319-328.
- Shah SK,McAnally KJ,Seoane L,Lombard GA, LaPlace SG, et al. (2016) Analysis of pulmonary non-tuberculous mycobacterial infections after lung transplantation. Transpl Infect Dis18: 585-591.
- Jarand J,Levin A,Zhang L,Huitt G,Mitchell JD,et al. (2011) Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Clin Infect Dis 52: 565-571.
Citation: Singhal D (2022) Axillary Lymph Node Metastases on the Contralateral Side in Primary Breast Cancer Development. Breast Can Curr Res 7: 167. DOI: 10.4172/2572-4118.1000167
Copyright: © 2022 Singhal D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1290
- [From(publication date): 0-2022 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 947
- PDF downloads: 343