Awareness and Associated Factors towards Neonatal Danger Signs among Mothers Attending Public Health Institutions of Mekelle City, Tigray, Ethiopia, 2015
Received: 14-Dec-2017 / Accepted Date: 26-Dec-2017 / Published Date: 30-Dec-2017 DOI: 10.4172/2375-4494.1000365
Abstract
Background: Neonatal mortality and morbidity are the greatest challenges in the current health care scenario. Majority of newborns die because mothers fail to identify danger signs of illness, and inappropriate/delayed care seeking. The most common identified newborn danger signs are fever, lethargy, inability to feed, low temperature, fast breathing, persistent vomiting, convulsions, pus draining/bleeding from umbilical area, lack of consciousness, yellow palm/sole/eye and eye discharge/redness. Objective was to assess the awareness level and factors associated towards neonatal danger sign among mothers who attend public health institutions of Mekelle City, Tigray, Ethiopia, 2015.
Method: A cross sectional study design was conducted from December 2014 to June 2015 among mothers who attend public health institutions of Mekelle city, Simple random sampling technique was used to select the study participants. The data were collected using interviewer administered structured questionnaire. Pre-test was done on 5% of the sample two weeks before the actual data collection period at Qui ha health center based on the result of the pre-test necessary corrections were made to the questionnaire. After the data was collected it was entered, cleaned and analyzed using SPSS version 20 statistical software. Descriptive statistics were employed. Binary logistic regression was used to see the association between the dependent and various independent variables. Finally, data are presented using text, tables and graphs.
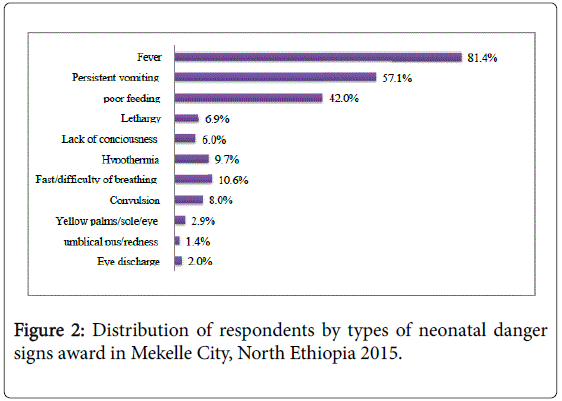
Result: This study found that half (50.6%) of mothers had an awareness of at least three neonatal danger signs. Fever, persistent vomiting and poor sucking was the three most commonly reported neonatal danger signs. To the reverse, umbilical redness, eye discharge, yellow palms/soles/eyes were found to be the least known neonatal danger signs which was reported by less than 5% of the study subjects. Birth preparedness by, at least in two ways [AOR=2.5; 95% CI (1.35, 4.66)] and post-natal care and advice [AOR=3.4; 95% CI (2.01, 5.77)] were the independent variables that show significant association with awareness of mothers toward neonatal danger signs in this study.
Conclusion and recommendations: Majority of mothers had low awareness of the majority of neonatal danger signs. Strengthening educational programs at a health facility or community level is highly recommended.
Keywords: Neonate; Danger signs; Awareness
Introduction
The neonatal period is the first 28 days of life. It is the most vulnerable time for a child’s survival. Globally, the main causes of neonate deaths are preterm birth complications, complications during labour and delivery (intrapartum-related complications), and sepsis. Together, these three causes account for almost three quarters of all neonatal deaths [1]. In low and middle income country settings, approximately three-quarters of neonatal deaths occur in the first week of life and nearly half occur in the first 24 hours, of which more than half occur at home. This time is critical to providing neonates with appropriate care at the onset of illness and delays in the decision to seek care can have significant consequences [2]. Most newborn morbidity and mortality could be averted if mothers and newborns receive appropriate care during pregnancy, childbirth and during the postpartum period. The essential newborn cares include thermal care, exclusive breastfeeding, and clean cord and eye care. In addition, resuscitation of neonates with asphyxia and prevention and early treatment of infections can save many newborns' lives [3]. Additionally, to deliver successful neonatal health care interventions, health care facilities and providers must not only be available and accessible, but illness must first be recognized and care desired by the neonate’s caregiver, often a parent or other family member. As such, understanding care-seeking practices become essential for health interventions have a positive impact [4].
Management of Neonatal and Childhood Illness (IMNCI) developed by the World Health Organization (WHO) identified the newborn danger signs of severe illness as history of difficulty feeding, movement only when stimulated, temperature below 35.5 oc, temperature above 37.5°C, respiratory rate over 60 breaths per minute, severe chest in drawings and, history of convulsions. Assessment of these signs will result in a high overall sensitivity and specificity for predicting the need for hospitalization of a neonate in the first week of life [5].
Increasing the awareness about danger signs among parents is therefore considered as one of the most important components of the strategy to reduce mortality among newborn babies. It was envisaged that this would help by ensuring that medical assistance is obtained at the earliest in case of an illness, thereby reducing the chances of mortality [6]. The care seeking behavior among the mothers underlines an urgent need to generate awareness among them to be able to recognize the danger signs in the newborns. Early identification of any danger signs of illness can ensure that mothers approach the health facility in time. It is also important that the mothers approach qualified health providers for treatment [3]. Sustaining the momentum on neonate survival requires a renewed effort to build stronger health services to provide high-quality prenatal care, skilled birth attendants and postnatal care for babies and mothers, as well as other cost effective interventions. Effective strategies to improve survival from neonatal infections in LMICs require a clear understanding of neonatal care- seeking behaviors and patterns by caregivers [1,2].
Globally 4 million neonates die every year before they reach the age of one month. In 2013, almost 1 million neonates died on the day they were born, accounting for 16 per cent of all under-five deaths. Between 1990 and 2013, 86 million neonates died worldwide within their first seven days of life. Together, low-income and lower-middle-income countries account for 85 per cent of all neonatal deaths. Approximately two thirds of all neonatal deaths worldwide occur in only 10 countries. Even though Ethiopia is among the countries with the largest percentage decline in the neonatal mortality rate from 1990–2013, 3% of the global neonatal deaths (84,000 in 2013) occurred in the country which places the country among the top six countries with the highest number of neonate deaths. Moreover, the most recent progress reports on global trends in neonate mortality have shown alarmingly slow progress, if any, in curbing mortality rates among neonates, the slowest being in sub-Saharan Africa [1].
According to an analysis based on data from middle income countries (MICs) and demographic and health survey (DHS) from about 60 countries, awareness of neonate’s danger signs are particularly dependent on income, maternal education and place of birth. Lower household wealth, an uneducated mother and birth in a rural area lower a neonate’s chance of survival within the first seven days of life, mostly in Africa and Asia. Educating women is crucial for reducing neonatal neonate. Neonatal mortality rates of babies born to mothers with no education are nearly twice as high as those of babies born to mothers with secondary education or higher. The family’s wealth and geographic location (urban/rural) also remain powerful determinants of inequities in awareness of neonate danger signs [7].
There are some who are of the view that the current effort at reducing neonate mortality is hindered by poor understanding of the social determinants of health as well as danger signs of neonate and putting in place appropriate strategies to reduce its impact [8]. It was suggested that most of the neonate deaths in high-mortality regions are due to preventable and behavioral modifiable causes (Such as neonate danger sign awareness). However, the level awareness of the neonate danger sign is not well known. Low utilization of available health services, such as supervised deliveries and postnatal care continue to persist even where financial and geographic access is deemed adequate [9]. As people attribute high neonate deaths to low utilization of neonatal care services at crucial stages of pregnancy, delivery, postpartum and post-natal periods, neonatal complications during birth or after the birth of a child greatly contribute to neonate mortality in developing nations [10]. If those factors affecting neonate danger sign are not well known and identified by the mothers, neonatal mortality and morbidity might continue and a challenge to the community as well as the government in the future. This research study is therefore aimed to assess awareness and associated factors toward neonatal danger signs among mothers attending in public health institutions of Mekelle city.
Methods and Materials
Study area and period
The study was conducted in Mekelle city, Tigray regional, state, Ethiopia, which is found at 783 Km north of Addis Ababa with latitude and longitude 130 29’N39’E13.4830N39.4570E and at an elevation of 2084 meters above sea level. Regarding health infrastructure of the city, it has nine governmental health centers, one referral hospital and one military hospital and two general hospitals and there are also 4 general hospitals, 38 clinics owned by private organizations. Mekelle has a total population of 264,907, of these 135,103 are female, 129,804 are male residents, 74,192 women in reproductive age (15-49 years) and 9,060 infants [11]. The study was conducted from January 2014 to June 2015 in Mekelle city.
Study design: An institution based cross–sectional study was employed.
Population: The source population for this study was all mothers with neonate who attend selected public health institutions of the Mekelle city during the data collection period and the study population was all sampled mothers with neonate who attend selected public health institutions in Mekelle city during the data collection period.
Eligibility criteria
Inclusion criteria: All mothers who had neonate during the study period were included and Exclusion Criteria: All Mothers who had neonate but unable to communicate because of seriously ill or impaired cognition.
Sample size determination: The sample size for this particular study was calculated using a formula for a single population proportion considering the following assumptions. A 95% confidence level, the margin of error (0.05), the proportion of mothers’ knowledge of neonatal danger signs in four regions of Ethiopia was (p=0.293) [12]. Accordingly, the value was substituted in the following single population proportion formula: n=(Za)2 × P (1-P)/d2, n=(1.96)2 × 0.293 (1-0.293)/(0.05)2, n=318. Where n=minimum sample size required, z=critical value for normal distribution at 95% confidence level which equals to 1.96 (z value at a=0.05), P=proportion of mothers’ knowledge on neonatal danger signs (29.3%) from previous study d=Margin of error (precision) which is 5%. with 10% nonresponse rate the total sample size was 350.
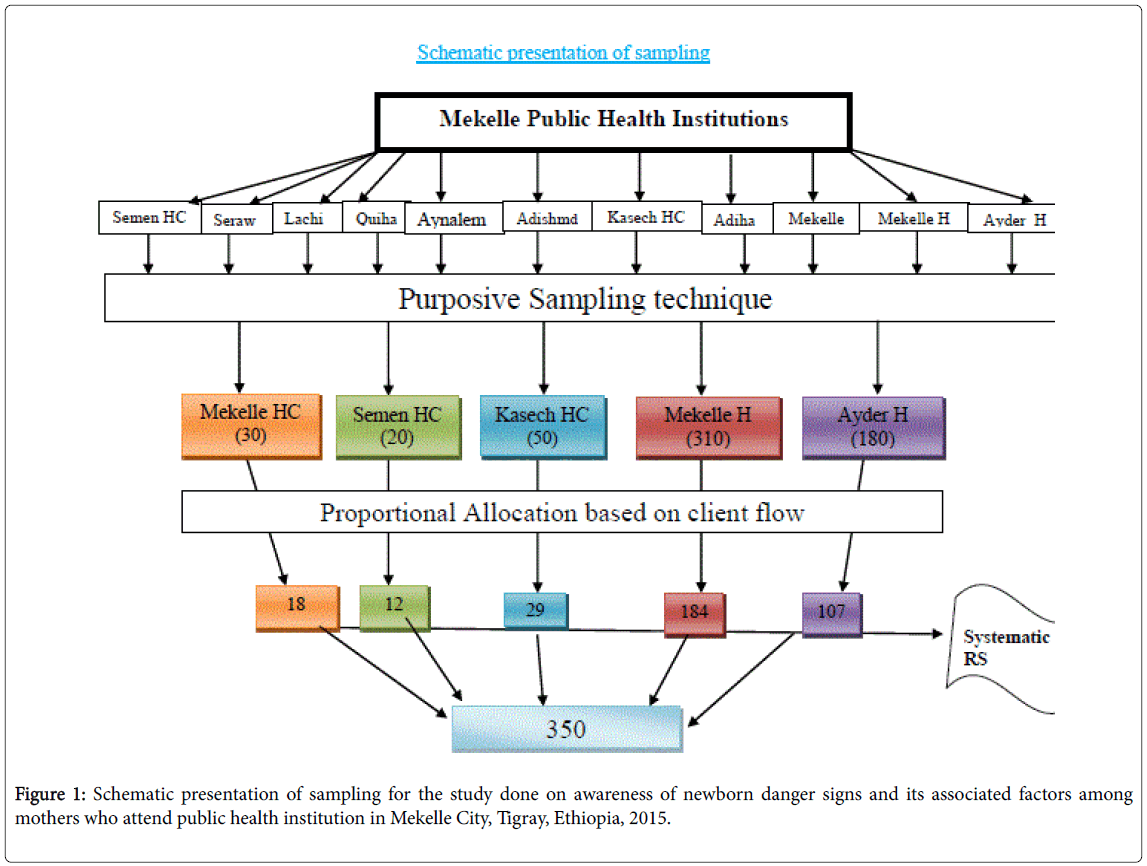
Sampling technique: There are 11 governmental health facilities in Mekelle city administration. From these 11 health facilities, 5 were selected purposely based on their client flow, namely Semien, Kasech, Mekelle Health Centers, Mekelle and Ayder Hospitals. Study subjects were obtained proportionally according to the client flow from each facility; all mothers with their index neonate who attend the selected public health institution (MCH units) during the data collection period were selected using the systematic sampling technique with every other interval (K=N/n, 590/350=1.69) until the predetermined sample size was obtained. The first case was selected using the lottery method (Figure 1).
Data collection tool and procedures
Data collection tool: A structured interviewer administered questionnaire, which is developed after reviewing of different literatures, was used to collect data. The questionnaire was prepared in English and it was translated into the local language Tigrigna and back retranslated into English. The tool has three parts; Part I - socio demographic related questions, Part II - Obstetric related and, Part III was used to collect data awareness level toward neonatal danger signs related questions.
Collection procedure: Four diploma nurses were trained for two days by the principal investigator about the purpose of the study and how to interview as well as fill the questionnaire properly. Data collectors were collected the data through interviewing the mothers throughout the data collection period after tracing based on their infant's medical record number.
Data quality control: Two days training was given to data collectors and supervisors on how to collect data. Pre-test was done on 5% of the sample population two weeks before the actual data collection period at Qui ha health center and necessary corrections were made to the questionnaire. Adequate supervision was undertaken by a supervisor and principal investigator during the data collection period. Spot checking for the collected questionnaire was done on a daily basis. In order to avoid errors during data entry 15% of the collected data was entered and checked randomly. Besides this, the principal investigator was cleaned and entered carefully to SPSS version 20.
Study variables: Dependent variable was Awareness of neonatal danger signs and Independent variables were Socio-demographic variables: maternal age, neonate age, religion, monthly income, educational status, ethnicity and marital status. Maternal health related factors; ANC attendance, birth preparedness, place of delivery, parity.
Data management and analysis: The collected data were entered and cleaned and analyzed using SPSS version 20. Frequencies and percentages were done for categorical variables. The normality of the population distribution was checked for continuous variables. The frequency, measure of central tendency and measures of dispersion (inter-quartile range) is reported. Binary logistic regression analysis was carried out to determine the magnitude, direction and strength of association between a set of independent and the dependent variable and finally those variables with P value <0.2 in the bivariate analysis were selected for multi variable analysis. Finally, the data presented using text, tables, and graphs.
Ethical considerations: This study was started after obtaining ethical clearance from Mekelle University College of Health Sciences ethical review committee (IRC). Support letter was obtained from Mekelle University College of Health Sciences to Tigray Regional Health Bureau and from Tigray regional health bureau for respective health institutions. In addition, informed consent was obtained from respondents to confirm their willingness to participate in the study after explaining the objective of the study. The respondents were notified that they have the right to refuse or terminate at any point of the interview. The information provided by each respondent was kept confidential. Beneficence and respect to the respondents was maintained throughout the study.
Operational definition: Neonatal danger sign: Danger signs of the neonate which may include either of difficulty in feeding, lethargy, hypothermia, convulsions, fever and fast or difficulty breathing, persistent vomiting, lack of consciousness, yellow palms/soles/eyes, umbilical pus/redness and eye discharge/redness Neonate - at least one baby whose age is less than 28 days. Level of awareness: High - if the mother of newborn answered more than three out of the eleven neonatal danger signs, Low-If the mother of the newborn answered less than three out of the eleven newborn danger signs [12].
Result
Socio demographic characteristics
In this study, a total of 350 mothers whose neonate aged 28 days and less were interviewed making the response rate to be 100%. The mean (+SD) age of mothers was 26.21 (+5.13). More than a third, 127 (36.3%) of mothers were in the age range 25-29 years. A majority, 332 (94.9%) were orthodox by religion and the largest ethnic group was Tigray, 340 (97.1%). Concerning the educational status of mothers, two hundred eighty three (80.99%) had attended formal school and 90 (25.7%) had accomplished college and higher. The majority of mothers were married, 346 (98.9%) and house wife by occupation, 211 (60.3%). Out of the total study subjects, 110 (31.4%) of mothers earn an average monthly income of higher than 1000 Birr. Study subjects were also asked about their husband’s educational status, 274 (78.3%) have attended formal education (Table 1).
| Variables | Categories | Frequency | Percent |
|---|---|---|---|
| Mother’s age | 15-19 | 25 | 7.1 |
| 20-24 | 107 | 30.6 | |
| 25-29 | 127 | 36.3 | |
| 30-34 | 60 | 17.1 | |
| 35+ | 31 | 8.9 | |
| Total | 350 | 100 | |
| Marital status | Married | 346 | 98.9 |
| Unmarried | 4 | 1.1 | |
| Total | 350 | 100 | |
| Religion | Orthodox | 332 | 94.9 |
| Muslim | 17 | 4.9 | |
| Catholic | 1 | 0.3 | |
| Total | 350 | 100 | |
| Ethnicity | Tigray | 340 | 97.1 |
| Amhara | 8 | 2.3 | |
| Others | 2 | 0.6 | |
| Total | 350 | 100 | |
| Residence | Urban | 298 | 85.1 |
| Rural | 52 | 14.9 | |
| Total | 350 | 100 | |
| Mother’s educational level | Unable to read and write | 60 | 17.1 |
| Able to read and write only | 7 | 2 | |
| Primary school | 88 | 25.1 | |
| Secondary school | 105 | 30 | |
| College and higher | 90 | 25.7 | |
| Total | 350 | 100 | |
| Father educational level | Unable to read and write | 46 | 13.1 |
| Able to read and write only | 30 | 8.6 | |
| Primary school | 64 | 18.3 | |
| Secondary school | 91 | 26 | |
| College and higher | 119 | 34 | |
| Total | 350 | 100 | |
| Mother’s Occupation | Housewife | 211 | 60.3 |
| Civil servant | 71 | 20.3 | |
| Merchant | 41 | 11.7 | |
| Owns private organization | 20 | 5.7 | |
| Daily laborer | 6 | 1.7 | |
| Others | 1 | 0.3 | |
| Total | 350 | 100 | |
| Monthly income | ≤500 | 67 | 19.1 |
| 501-1000 | 55 | 15.7 | |
| >1000 | 110 | 31.4 | |
| Do not know | 118 | 33.7 | |
| Total | 350 | 100 |
Table 1: Socio-demographic characteristics of respondents attending public health institutions of Mekelle City, North Ethiopia, 2015 (n=350).
Maternal health related factors
Study subjects were asked about their history of ANC visits during pregnancy of the current neonate, 339 (96.9%) and 246 (70.3%) of them were received ANC service at least once and more than four times during the pregnancy respectively. Two hundred ninety nine (85.4%) of the mothers were made birth preparedness by either by saving money, arranging transport, identifying skilled birth attendant or buying materials. Most 345 (98.6%) of mothers gave birth to their current child in health institutions where 296 (84.6%) of them were giving birth in hospitals. And more than two third, 215 (61.4%) of those mothers were received advice on neonatal danger signs during the postnatal follow up (Table 2).
| Variables | Number | Percent |
|---|---|---|
| Parity | ||
| 1 | 162 | 46.3 |
| 4-Feb | 159 | 45.4 |
| 5 and above | 29 | 8.3 |
| Total | 350 | 100 |
| History of ANC | ||
| Yes | 339 | 96.9 |
| No | 11 | 3.1 |
| Total | 350 | 100 |
| Number of ANC visit | ||
| 3-Jan | 51 | 15 |
| 8-Apr | 213 | 62.8 |
| >8 | 33 | 9.7 |
| Do not remember | 42 | 12.4 |
| Total | 339 | 100 |
| Birth preparedness | ||
| Yes | 299 | 85.4 |
| No | 51 | 14.6 |
| Total | 350 | 100 |
| Place of delivery | ||
| Home | 3 | 0.9 |
| Hospital | 296 | 84.6 |
| Health center | 49 | 14 |
| Others | 2 | 0.6 |
| Total | 350 | 100 |
| Birth attendant | ||
| TBA | 2 | 0.6 |
| Health professional | 346 | 98.9 |
| Relatives | 1 | 0.3 |
| Others | 1 | 0.3 |
| Total | 350 | 100 |
| postnatal advice on neonatal danger signs | ||
| Yes | 215 | 61.4 |
| Yes | 215 | 61.4 |
| No | 135 | 38.6 |
| Total | 350 | 100 |
Table 2: Distribution of pregnancy and obstetrics related variables of respondents attending public health institutions of Mekelle City, North Ethiopia, 2015. (n=350).
Awareness of mothers towards neonatal danger signs
This study revealed that from a total of 350 respondents, 90% (n=315) of mothers were aware of at least one of the eleven listed key neonatal danger signs. However, only 50.6% (n=177) of all mothers had high awareness which we're aware of at least three of the eleven defined neonatal danger signs. Fever was more commonly known danger sign by almost 81.4% (n=285) of the mothers. The response “persistent vomiting” and “poor feeding” was given by 57.1% (n=200) and 42% (n=147) of the respondents respectively. The awareness of mothers of the remained neonatal danger signs, however, is very low which ranges from only 10.6% to 1.4% of mothers were aware of either of the remained eight neonatal danger signs. The least known danger signs were yellow palms/soles/eyes, pus or redness around the umbilicus and eye discharge or redness, stated by less than 5% of the respondents (Figure 2).
Associated factors of neonatal danger sign awareness among mothers
The awareness level of mothers regarding neonatal danger signs was assessed for its association with socio-demographic, pregnancy and obstetric related variables. The binary logistic regression model showed that the residence of mothers was significantly associated with awareness level of mothers on neonatal danger signs (p=0.000) in which urban residents were 4.1 times more likely to be aware of neonatal danger signs as compared to their counterpart [COR=4.14; 95% CI (2.09, 8.2)]. Maternal education was statistically associated with awareness of neonatal danger signs (P=0.003). Mothers who had college and higher educational level were 3.3 times more likely to know the defined neonatal danger signs than those who had no formal education [COR=3.3; 95% CI (1.71, 6.41)]. Likewise, those mothers whose husband had an educational level of college and higher were 3.9 times more likely to be aware of the neonatal danger signs than those whose their husbands' educational level were no formal education [COR=3.93; 95% CI (2.12, 7.26)].
Maternal occupation was also statistically significant with awareness of neonatal danger signs (p=0.016). Those mothers who were civil servants were two fold times more likely to be aware of the defined neonatal danger signs as compared to those housewives [COR=2.12; 95% CI (1.22, 3.66)]. Monthly income was also statistically significant (P=0.000). Those mothers who had a household income of 501 to 1000 Ethiopian Birr was 2.2 times more likely to be aware of neonatal danger signs [COR=2.22; 95% CI (1.07, 4.60)] and those who had more than 1000 Ethiopian Birr monthly incomes were also 2.9 times more likely to be aware of the defined neonatal danger signs as compared to those who had Ç 500 Ethiopian Birr household monthly income [COR=2.92; 95% CI (1.56, 5.48)].
Number of ANC visits (p=0.011), birth preparedness by at least two ways (p=0.000), postnatal care advice on neonatal danger signs (p=0.000), travel time to nearby health facility (p=0.003) and parity (p=0.009) were also statistically significant to awareness of the defined neonatal danger signs. Mothers who had ANC follow up four times and above were 2.6 times more likely to be aware of neonatal danger signs as compared to those mothers who had 1 to 3 ANC follow up [COR=2.66; 95% CI (1.4, 5.06)]. Mothers, those who were prepared for birth by at least two ways (saving money, identifying transport, identifying skilled birth attendant or buying materials) were three times more likely to be aware of neonatal danger signs as compared to their counterpart [COR=3.14; 95% CI (1.98, 4.98)]. Similarly, those mothers who had postnatal follow up and who received advice regarding neonatal danger signs were 4 times more likely to know the defined neonatal danger signs as compared to their counterpart [COR=4.17; 95% CI (2.63, 6.62)].
Mothers who had travel time less than 1 hour were 2.2 times more likely to be aware of neonatal danger signs than those who had travel time C1 hour to the nearby health facility [COR=2.23; 95% CI (1.31, 3.8)]. In addition, having TV, radio or reading magazine was also statistically significant with awareness of neonatal danger signs (p=0.000). Those mothers who had either of TV, radio or read magazines were 3.9 times more likely to be aware of neonatal danger signs as compared to their counterpart [COR=3.93; 95% CI (2.30, 6.72)]. On the other hand, maternal age, marital status, neonate’s age, birth attendant and place of delivery were not statistically significant.
In the multivariate analysis, adjusting possible confounding variables, birth preparation by at least in two ways [AOR=2.5; 95% CI (1.35, 4.66)] and post-natal care advice on neonatal danger signs [AOR=3.4; 95% CI (2.01, 5.77)] were statistically associated with awareness of neonatal danger signs. Likewise residence, number of ANC visits, parity, monthly household income, maternal education, maternal occupation, paternal education, having information source, and travel time to the nearby health facility were not retained as a significant factor in the multivariate analysis (Table 3).
| Variables | Category | Awareness of mothers on neonatal danger signs | |||
|---|---|---|---|---|---|
| High | Low | COR (95%CI) | AOR (95%CI) | ||
| Residence | Urban Rural 15-19 | 165 (55.4%) | 133 (44.6%) | 4.135 (2.09, 8.19)* | 2.13 (0.83, 5.50) |
| 20-24 | 12 (23.1%) | 40 (76.9%) | 1 | ||
| Maternal age | 25-29 | 11 (44.0%) | 14 (56.0%) | 0.84 (0.29, 2.42) | |
| 30-34 | 51 (47.7%) | 56 (52.3%) | 0.97 (0.44, 2.16) | ||
| 35+ | 66 (52.0%) | 61 (48.0%) | 1.15 (0.53, 2.53) | ||
| Illiterate Primary school | 34 (56.7%) | 26 (43.3%) | 1.40 (0.58, 3.33) | ||
| Maternal education level | Secondary school College and higher House wife | 15 (48.4%) | 16 (51.6%) | 1 | |
| Civil servant Business woman Others | 23 (34.3%) | 44 (65.7%) | 1 | 1 | |
| Maternal occupation | Illiterate primary school | 40 (45.5%) | 48 (54.5%) | 1.59 (0.83,3.07) | - |
| Secondary school College and higher | 57 (54.3%) | 48 (45.7%) | 2.27 (1.21, 4.28)* | ||
| <500 | 57 (63.3%) | 33 (36.7%) | 3.30 (1.71, 6.41)* | ||
| Father's educational level | 501-1000 | 92 (43.6%) | 119 (56.4%) | 1 | 1 |
| 1001 and above Do not know Yes | 44 (62.0%) | 27 (38.0%) | 2.11 (1.22, 3.66)* | 0.46 (0.16,1.29) | |
| Monthly income | No | 24 (58.5%) | 17 (41.5%) | 1.83 (0.93, 3.60) | 0.54 (0.19, 1.59) |
| 17 (63.0%) | 10 (37.0%) | 2.20 (0.96, 5.03) | 0.61 (0.17, 2.18) | ||
| 3-Jan | 23 (30.3%) | 53 (69.7%) | 1 | 1 | |
| History of ANC | 4 and above | 31 (48.4%) | 33 (51.6%) | 2.17 (1.08, 4.33)* | 0.97 (0.44, 2.13) |
| Do not remember Yes | 48 (52.7%) | 43 (47.3%) | 2.57 (1.36, 4.88)* | 1.01 (0.47, 2.18) | |
| Number of ANC visit | No Yes No | 75 (63.0%) | 44 (37.0%) | 3.93 (2.12, 7.26)* | 1.48 (0.52, 4.24) |
| 1 | 27 (40.3%) | 40 (59.7%) | 1 | 1 | |
| Birth preparedness by at least 2 ways | 4-Feb | 33 (60.0%) | 22 (40.0%) | 2.22 (1.07, 4.60)* | 1.86 (0.71, 4.88) |
| Postnatal care advice Parity | 5 and above Yes | 73 (66.4%) | 37 (33.6%) | 2.92 (1.56, 5.48)* | 1.81 (0.67, 4.85) |
| No | 44 (37.3%) | 74 (62.7%) | 0.88 (0.48, 1.63) | 2.30 (0.80, 6.66) | |
| 174 (51.3%) | 165 (48.7%) | 2.81 (0.73, 10.78) | 1 | ||
| Haves TV/radio or reads magazine | 3 (27.3%) | 8 (72.7%) | 1 | 1.38 (0.56, 3.37) | |
| 2.11 (0.90, 4.93) | |||||
| 16 (31.4%) | 35 (86.6%) | 1 | 1.43 (0.62, 3.30) | ||
| 135 (54.9%) | 111 (45.1%) | 2.66 (1.40, 5.06)* | - | ||
| 23 (54.8%) | 19 (45.2%) | 2.65 (1.13, 6.18) | |||
| 86 (68.3%) | 40 (37.1) | 3.14 (1.98, 4.98)* | 1 | ||
| 91 (40.6%) | 133 (59.4%) | 1 | 1.40 (0.65, 3.01) | ||
| 137 (63.7%) | 78 (36.3%) | 4.17 (2.63,6.62)* | 1.28 (0.48, 3.43) | ||
| 40 (29.6%) | 95 (70.4%) | 1 | 2.50 (1.35, 4.66)** | ||
| 73 (45.1%) | 89 (54.9%) | 1.56 (0.68, 3.56) | 1 | ||
| 94 (59.1%) | 65 (40.9%) | 2.75 (1.20, 6.29)* | 3.40 (2.00,5.77)** | ||
| 10 (34.5%) | 19 (65.5%) | 1 | 1 | ||
| 154 (58.6%) | 109 (41.4%) | 3.93 (2.30, 6.72)* | 0.57 (0.19, 1.71) | ||
| 23 (26.4%) | 64 (73.6%) | 1 | 1.16 (0.40, 3.40) | ||
| 1 | |||||
| 1.21 (0.59, 2.49) | |||||
| 1 | |||||
| Travel nearby facility | Time to health | <1 h | 151 (54.7%) | 125 (45.3%) | 1.15 (0.54, 2.43) |
| Ç 1 h | 26 (35.1%) | 48 (64.9%) | 1 | ||
*p-value<0.05 in bivariate, **p value<0.05 in multivariable analysis
Table 3: Binary logistic regression analysis result of related variables to awareness level respondents to ward neonatal danger signs in Mekelle City, North Ethiopia 2015.
Discussion
The purpose of this study was to assess awareness towards neonatal danger signs and associated factors among mothers attending in Mekelle City public health institutions. In this study it was found that almost half (50.6%) of mothers were aware of at least three of eleven listed neonatal danger signs. This result is more or less similar to the study in north India [9] which was 50%. But it is lower than being aware of mothers at least three danger signs in rural Wardha, India [13] which was 67.4%. And the findings of this study are higher than the awareness of mothers in Ghana 2013 [14] which was 28.3% and the awareness in 4 regions (Tigray, Oromia, Amhara and SNNP) of Ethiopia [15] which was 29.3%. These variations and encouraging result might be explained in terms of the high proportion of respondents from urban in which the habit of attending information is higher than in rural areas.
This study showed that “fever” is the commonest known neonatal danger sign which is reported by 81.4% of the mothers. This finding is consistent with the findings in peri urban Wardha, India (2008) [16] which was reported by 76.4%, Luck know City India (2006) [17] which was reported by 76.9%, Ghana (2013) [18], and in the previous study in 4 regions of Ethiopia (2012) [15] which was reported by 83.6% of the mothers. “Poor sucking” is also found to be among the three most commonly reported neonatal danger signs in this study, which is reported by 42.0% of mothers which is in agreement with findings in the study conducted in Lucknow city, India (2006) [17] which was reported by 68.9%, rural Waldha, India (2007) [19] which was responded with 61.6%, Bangladesh (2007) [20] which was responded with 56%, and Ghana (2013) [21] and Ethiopia (2012) [22] which was responded by 39.5%. This study also found that “umbilical redness”, “eye redness or discharge” and “yellow palms/sole, eye” are the least known neonatal danger signs which was responded by Ç 5% of mothers. Surprisingly, this result is in line with the findings in Ghana (2013) [23] which was umbilical redness by 4.9%, yellow palms by 6.4% and in the previous study in the 4 regions in Ethiopia (2013) [24-27] which was umbilical redness by 1.7%, yellow palm by 0.4% of the mothers. In the binary logistic regression analysis of this study showed that birth preparedness by at least two ways has appeared to be unaffected by any confounders [AOR=2.5; 95% CI (1.35, 4.66)]. This result is consistent with the study conducted in Uganda (2011) [28] where mothers who prepared for birth were more likely to be aware of neonatal danger signs [AOR=1.7; 95% CI (1.2, 2.2)].
Conclusion and Recommendations
Conclusion
This study revealed that the awareness of neonatal danger signs among mothers was better as compared to the previous study conducted in Ethiopia. But nearly half of mothers had low awareness of the neonatal danger signs and majority of them did not aware either of umbilical redness/discharge, eye redness/discharge or yellow palm/ sole/eyes as neonatal danger signs. In the bivariate logistic regression analysis; residence, maternal education, maternal occupation, paternal education, monthly household income, parity, number of ANC, birth preparedness by at least two ways, postnatal care and advice, having information source, travel time to the nearby health facility were significantly associated with awareness of neonatal danger signs. Of these variables, birth preparedness by at least two ways and postnatal care and advice were the independent determinant factors for awareness of mothers regarding neonatal danger signs.
Recommendations
Based on the study findings the following recommendations are forwarded:
• It is better if the health care providers work on educational programs at health facilities aimed to increase the mothers' awareness level of the different neonatal danger signs.
• It is also recommended if the HEWs provides health education regarding neonatal danger signs at community level to increase awareness level among mothers.
• It is well again if the stakeholders (RHB and NGOs) strengthen and sustain the existing newborn care strategies, and approaches for further improvement of awareness of the mother towards neonatal danger signs.
• Further studies that mainly address all areas of associated factors that may significantly affect the awareness level of mothers towards neonatal danger signs are needed.
References
- Unicef (2014) Committing to child survival: A Promise Renewed. Progress Report 2014.
- Herbert HK, Lee ACC, Chandran A, Rudan I, Baqui AH (2012) Care Seeking for Neonatal Illness in Low- and Middle-Income Countries: A Systematic Review. PLoS Med 9: e1001183.
- Urban Health Resource Centre (2008) Newborn Care Scenario in the slums of Meerut, Uttar Pradesh: Implications for Program & Policy Urban Health Resource Centre, New Delhi.
- Md. Mahbubul H (2011) Newborn Care Practices by the Mother/Care Givers’ and Their Knowledge about Signs of Sickness of Neonates. Bangladesh J Child Health 35: 90-96.
- Aga Khan Foundation (2011) Endline Study for Community Led Initiatives for Child Survival (CLICS): Final Report. ORG Centre for Social Research, Neilesen.
- Black RE, Morris SS, Bryce J (2003) Where and why are 10 million children dying every year? Lancet 361: 2226-2234.
- Khan MH, Kahlique N, Sddiqui AR, Amir A (2013) Newborn Care Practices among Slum Dwellers in Aligarh City, Uttar Pradesh. Indian J Community Health 25: 28-33.
- Shally A (2006) Danger signs of neonatal illnesses: perceptions of caregivers and health workers in northern India. Bull World Health Org 84: 819-826.
- Kyomuhendo GB (2003) Low use of Rural Maternity Services in Uganda: Impact of Women’s Status, Traditional Beliefs and limited Resources. Reproductive Health Matters, 11: 16-26.
- Mahbubul H, Mohammed FHK, Jotsnaara B, Mak AC, Lars AP (2011) Newborn care practices by the mother/care givers’ and their knowledge about signs of sickness of neonates. Bangladesh J Child Health 35: 90-96.
- Liu L, Johnson HL, Cousens S, Perin J, Scott S, et al. (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379: 2151-2161.
- Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S (2010) 3.6 million neonatal deaths–what is progressing and what is not? Semin Perinatol 34: 371-386.
- Bhargava SK (2004) The Challenges of Neonatal Mortality in India. Indian Pediatr 41: 657-662.
- Dongre AR, Garg BS (2006) Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha, India. Indian J Pediatr 75: 325- 329.
- Padiyath MA, Bhat VB, Ekambaram M (2010) Knowledge attitiude and practice of neonatal care among postnatal mothers. Curr Pediatr Res 14: 147-157.
- Young Infants Clinical Signs Study Group (2008) Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet 371: 135-142.
- Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA (2005) Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics 2: 519-617.
- Dongre AR, Deshmukh PR, Garg BS (2009) A Community Based Approach to Improve Health Care Seeking for Newborn Danger Signs in Rural Wardha, India. Indian J Pediatr 76: 45-50.
- Rama R, Gopalakrishnan S, Udayshankar PM (2014) Assessment of knowledge regarding new-born care among mothers in Kancheepuram district, Tamil Nadu. Int J Community Med Public Health 1: 58-63.
- Oommen A (2012) Mothers Awareness Regarding Danger Signs of Neonatal Illnesses at a Selected Hospital in Trivandrum. Int J Nurs Care 1: 2-6.
- Gupta P, Srivastava VK, Kumar V, Jain S, Masood J (2012) Care seeking behaviour of mothers during illness of newborn in urban slums of Lucknow City. Indian J Community Health 24: 179-183.
- Kuganab-Lem R, Yidana A (2014) Exploring Women Knowledge of Newborn Danger Signs: A Case of Mothers with under Five Children. Public Health Res 4: 195- 202.
- Sandberg J, Odberg Pettersson K, Asp G, Kabakyenga J, Agardh A (2014) Inadequate Knowledge of Neonatal Danger Signs among Recently Delivered Women in Southwestern Rural Uganda: A Community Survey. PLoS ONE 9: e97253.
- Callaghan-Koru A, Abiy Seifu A, Tholandi M, Daniel E, Rawlins B, et al. (2013) Newborn care practices at home and in health facilities in 4 regions of Ethiopia. BMC Pediatr 13: 198.
- Tumla S (2013) Knowledge and Practice of Postnatal Mother in Newborn Care. J Nepal Med Assoc 52: 372-377.
Citation: Adem N, Berhe KK, Tesfay Y (2017) Awareness and Associated Factors towards Neonatal Danger Signs among Mothers Attending Public Health Institutions of Mekelle City, Tigray, Ethiopia, 2015. J Child Adolesc Behav 5: 365. DOI: 10.4172/2375-4494.1000365
Copyright: © 2017 Adem N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 7144
- [From(publication date): 0-2017 - Dec 21, 2024]
- Breakdown by view type
- HTML page views: 6141
- PDF downloads: 1003