Avascular Necrosis of the Talus in Juveniles
Received: 22-Aug-2017 / Accepted Date: 30-Aug-2017 / Published Date: 07-Sep-2017 DOI: 10.4172/2329-910X.1000246
Abstract
Avascular necrosis of the talus after severe ankle injury is well known. Avascular necrosis of talus is extremely rare in juveniles. However, it has been controversial whether the incidence of AVN after fracture of talus is higher in adult than in juveniles. It is possible that the immature talus can be more susceptible to circulatory. As treatment of avascular necrosis of the talus, non-operative treatment could be considered in juveniles. Prolonged non weight bearing might not be necessary for avascular necrosis of the talus.
Keywords: Avascular necrosis; Talus; Corticosteroids; Ankle injury
13803Short Communication
The causes of avascular necrosis of the talus are a traumatic and post-traumatic. Concerning about pathogenesis of a traumatic osteonecrosis, it has been reported in association with many condition as use of corticosteroids, alcoholism, occlusive vascular disease and systematic lupus erythematosus [1-3]. Concerning about pathogenesis of post-traumatic osteonecrosis, avascular necrosis of the talus after severe ankle injury is well known [4].
Hawkins showed a classification useful in the initial treatment of a patient with a vertical fracture of the neck of the talus, and reported that subchondral atrophy excludes the diagnosis of avascular necrosis. After avascular necrosis, reestablishment of blood supply through the medial surface of the talus play a major role in the replacement process, especially in fractures of the talar neck [5]. Mulfinger reported that the blood supply to the talus is quite diffuse and arises from the three major arteries of the lower leg. The incidence of necrosis rises sharply with dislocation and fracture-dislocation of the body [6]. Avascular necrosis of talus is extremely rare in children. The reason is that fractures of the talus are extremely rare in children. Schmit reported that the incidence varies between 0.01 and 0.08% [7-9]. According to Rammelt, long-term or multicenter clinical studies only report between one and two dozen cases. In the fracture of talus, the incidence of AVN is higher in displaced fractures than in nondisplaced fracture [10]. Mulfinger reported most fractures of neck of talus do not cause avascular necrosis of the body. Avascular necrosis of the body of the talus after simple fracture of the neck must imply unrecognized soft-tissue damage around the talus with arterial occlusion from soft tissue swelling or arterial rupture from dislocation [6]. On the other hand, the point that the incidence of AVN after fracture of talus is higher in adult than in child has been controversal. Pereles reported that AVN after fracture of talus is higher in adult than in child [11]. Mazel reported that the immature talus seems to be more susceptible to circulatory [12].
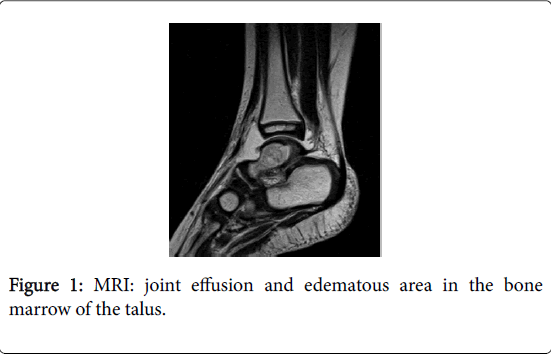
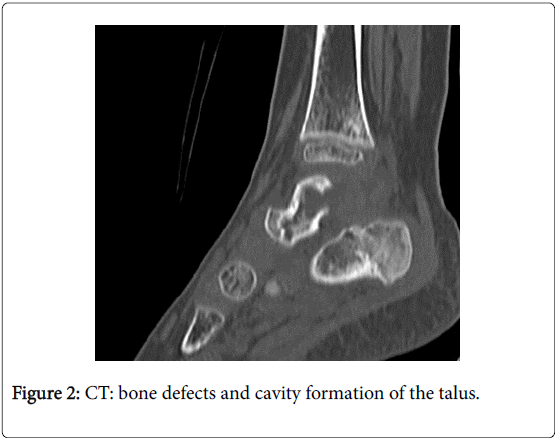
We encountered a 2-year-old child case of avascular necrosis of the talus without fracture. He did not have obvious past history of fracture and dislocation of the talus. According to histological findings, we considered the diagnosis to be posttraumatic avascular necrosis of the talus. It was considered that hyperflexion of the ankle joint in grass sleigh had caused soft tissue damage around the talus, although he did not have the fracture of talus. Collapse did not occur, cortical defect in the posterolateral corner occurred (Figures 1 and 2).
As treatment of avascular necrosis of the talus, non-operative treatment, core decompression, or arthrodesis could be considered. Non-operative treatment is use of anti-inflammatory analgesic, physiotherapy, partial weight-bearing and an ankle-foot orthosis. Use of anti-inflammatory analgesic is effective for pain, but not for avascular necrosis. Physiotherapy is important to decrease pain and swelling around the ankle joint. However, we consider that revascularization of the necrotic talus could not be prompted directly with physiotherapy. The period for partial weight-bearing and use of ankle-foot orthosis is controversial. There is no controlled study comparing early functional treatment with gradual weightbearing and prolonged non-weight-bearing. Rammelt reported there is no clear advantage for prolonged non-weightbearing. Non-weightbearing only for as long as the symptoms of pain and swelling exist is recommended [10]. In our case, non-weight-bearing with cast was for 2 months. Collapse did not occur. We considered that prolonged non-weightbearing might not be necessary for avascular necrosis of the talus.
References
- Adleberg JS, Smith GH (1991) Corticosteroid induced avascular necrosis of the talus. J Foot Surg30:66-69.
- Cruess RI(1981) Steroid induced osteonecrosis:a review. Canadian J Surg24:567-571.
- Harris RD, Silver RA (1973) Atraumatic aseptic necrosis of the talus. Radiology106:81-83.
- Lancaster S, Horowitz M, Alonso J (1985)Subtalar dislocations: A prognosticating classification. Orthopedics 8:1234-1240.
- Hawkins LG (1970) Fractures of the neck of the talus. J Bone and Joint Surg52: 991-1002.
- Mulfinger GL, Trueta J (1970) The blood supply of the talus. J BoneJoint Surg 52:160-167.
- Schmidt M, Havemann D, Behrens P (1990)Talusfrakturenbeikindermund jugendlichen. Vertetzungen der unterenextremitatenbeikindemund jugendlichen. Springer Verlag, Berlin,pp. 337-339.
- Draijer F, Havemann D, Beilstein D (1995)VerietzungsanalysekindlicherTalusfrakturen. Unfallchirug 98:130-132.
- Jensen I, Wester JU, Rassmussen F, Lindequist S,Schantz K (1994) Prognosis of fracture of the talus in children: 21-year follow-up of 14 cases. ActaOrthopScand65:398-400.
- Rammelt s, Zwipp H, Gavlik JM (2000) Avascular necrosis after minimally displaced talus fracture in a child. Foot Ankle Int 21:1030-1036.
- Pereles TR, Koval KJ, Feldman DS (1996) Fracture dislocation of the neck of the talus in a ten year old: A case report and review of the literature. BullHospJoint Dis55:88-92.
- Mazel C, Rigault P, Padovani JP, Finidori G, Touzet P (1986) Les fracture de l’astragale de I’enfant: A propos de 23 case. Rev ChirOrthop 72:183-195.
Citation: Mine T (2017) Avascular Necrosis of the Talus in Juveniles. Clin Res Foot Ankle 5: 246. DOI: 10.4172/2329-910X.1000246
Copyright: © 2017 Mine T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5129
- [From(publication date): 0-2017 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 4311
- PDF downloads: 818