Research Article Open Access
Autopsy Rates in the Department of Veterans Affairs Comparisons by Treating Specialty and Venue
Gary Hsin*, Periyakoil VJ and James HallenbeckDepartment of Medicine, Stanford University School of Medicine, USA
- *Corresponding Author:
- Dr. Gary Hsin
VA Palo Alto Health Care System
3801 Miranda Ave, Palo Alto, CA 94304, USA
Tel: 650-849-0550
Fax: 650-849-0260
E-mail: gary.hsin@va.gov
Received date: November 10, 2012; Accepted date: March 14, 2012; Published date: March 16, 2012
Citation: Hsin G, Periyakoil VJ, Hallenbeck J (2012) Autopsy Rates in the Department of Veterans Affairs Comparisons by Treating Specialty and Venue. J Palliative Care Med 2:109. doi:10.4172/2165-7386.1000109
Copyright: © 2012 Hsin G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Background: Institutional autopsy rates have fallen in recent years. Significant variability in autopsy rates by venue of care has been described.
Objectives: To compare institutional autopsy rates by treatment specialty and venue in the Department of Veterans Affairs and to the community. To explore the role of palliative care in autopsy inquiries.
Research Design: Compare national autopsy rates by acute care and nursing home treating specialties for two fiscal years.
Subjects: Decedents as recorded anonymously in a national VA database, classified by terminal venue of care, treating specialty, and autopsy status.
Measures: Chi-squared, Odds ratios for data using nominal scales, linear regression for interval scale data.
Results: 40,481 deaths in fiscal years 2006-2007 were examined. As compared to those dying in general medicine (autopsy rate [A.R]: 7.6%), decedents elsewhere were significantly more likely to undergo autopsies on surgical intensive care (A.R: 14.7%), surgical ward (A.R: 15.7%), or medical intensive care (A.R: 10.6%) treating specialties (Odds ratio [O.R]: 2.10, 2.27, 1.45, respectively, p.0.000) and less likely to undergo autopsy in nursing home (A.R: 5.7%) or inpatient hospice (A.R: 3.7%) treating specialties (O.R: 0.74, 0.47 respectively). VA acute hospital autopsy rates have declined 29% over the past 10 years.
Conclusions: VA autopsy rates show significant variation across venues and specialties, but are still generally higher than in the private sector, although still low against historic norms. Significant changes in education and processes regarding autopsy inquiry must take place.
Introduction
In recent decades autopsy rates have declined dramatically and numerous writers have lamented the “death” of the autopsy [1-6]. In this paper we compare autopsy rates for veterans dying in Veterans Affairs (VA) facilities by treating specialty and venue. Our primary purposes in doing so are:
1. To compare institutional autopsy rates across venues and treating specialties in terms of the probability of receiving an autopsy including hospice.
2. To compare these rates to published rates in the private sector.
3. To determine if autopsy rates have stabilized or are continuing to decline in recent years.
A major argument for the declining autopsy rate in the literature has been that the costs of autopsies to families and hospitals are generally uncompensated [4,7,8]. In the VA, where costs are borne by the Department of Veterans Affairs, this is not an issue for patients and families. Barriers such as cost or coordination with community pathologists that might exist in the private sector to obtaining autopsies in nursing homes are also minimized in the VA, which functions as an integrated healthcare system. The VA provides a unique opportunity to make such comparisons. As a healthcare system the VA is strongly supportive of autopsies. VA policy formally requires that “permission to perform an autopsy must be requested in every instance when a patient dies while an inpatient at a VHA facility.” [9]. Thus, we might expect higher autopsy rates in the VA with less variance in rates among institutional venues as compared to the private sector.
Hospice and palliative care physicians working inside and outside the VA are frequently called upon to care for those at the end-oflife. The request for and consent of autopsies is certainly a part of the practice for many palliative care professionals. The findings open an opportunity for further discussion about autopsies and end-of-life care, and what role should palliative care clinicians have in terms of communication with patients and families regarding autopsies.
Methods
A retrospective analysis was conducted of institutional deaths in the VA during fiscal years 2006 and 2007 (Oct 1, 2005-September 30, 2007), as classified by venue (acute care or nursing home) and treating specialty, using data available through the VHA Support Services Center (VSSC), a VA intranet database of patient workload. The acute care treating specialties analyzed included general medicine, general surgery, medical, and surgical critical care, as most acute care deaths occurred in these specialties and their respective venues of care, inpatient medical wards and ICU’s. Other treating specialties and venues (such as rehabilitative medicine and spinal cord injury units) which are also included in the same VA acute hospital database were excluded from our analysis because few deaths occurred in them and because they would not generally be considered acute hospital care workload in the private sector. In the VA’s Community Living Center (CLC) venue, which is analogous to community nursing homes, nursing home treating specialties included the general classification of nursing home patients and a treating specialty identifying patients as meeting hospice criteria. General medicine was treated as the reference group, as the greatest percentage of institutional deaths (28%) was in this group. Study population accounted for 92.4% of all deaths during the study period.
All deaths were classified as being with or without autopsy. A chisquared analysis was used to compare autopsy rates among treating specialties and odds ratios were calculated, comparing treating specialties to autopsy rates on the general medicine treating specialty. (Primer of Biostatistics 5.0 software) National VA institutional autopsy rates from 1998-2007 were also determined using this database, subsequently trended, and tested for significance using linear regression. (SPSS 15.0 software) Two different softwares were used for data analysis since the chi-squared analysis was easily accomplished with a basic biostatistics program, while the regression analysis required the use of more powerful statics software. As this study analyzed decedent data, commonly available to VA practitioners, which includes no personal identifying information, our Institutional Review Board (IRB) determined that IRB approval was not required. Approval was obtained from our VA Research and Development Committee.
Results
In fiscal years 2006-2007, 43,827 institutional deaths were recorded nationally in the VA. Deaths in the six treating specialties studied accounted for 40,481 (92.4%) of these deaths. 55.7% of all institutional deaths were in the acute care treating specialties studied and 36.7% of deaths were in VA nursing homes. Deaths in intensive care accounted for 26.6% of all institutional deaths and 47.7% of acute care treating specialties studied. General Medicine (non-ICU) deaths accounted for the greatest percentage of deaths among treating specialties studied (28.0%, followed by hospice treating specialty deaths (26.7%) and medical intensive care deaths (22.4%). Table 1 summarizes these results.
2007 |
Autopsy | No Autopsy |
Total Deaths |
% Deaths with Autopsy |
% All Deaths |
Odds Ratio |
95% Confidence Interval |
P Value |
|---|---|---|---|---|---|---|---|---|
| Medicine | 930 | 11360 | 12290 | 7.57% | 28.04% | REF 1.00 | ||
| MICU | 1039 | 8765 | 9804 | 10.60% | 22.37% | 1.45 | 1.32-1.59 | 0.000 |
| Surgery | 72 | 388 | 460 | 15.65% | 1.05% | 2.27 | 1.75-2.94 | 0.000 |
| SICU | 269 | 1567 | 1836 | 14.65% | 4.19% | 2.10 | 1.81-2.43 | 0.000 |
| Nursing Home | 250 | 4121 | 4371 | 5.72% | 9.97% | 0.74 | 0.64-0.86 | 0.000 |
| Hospice | 434 | 11286 | 11720 | 3.70% | 26.74% | 0.47 | 0.42-0.53 | 0.000 |
| Total | 2994 | 37487 | 40481 | 7.40% | 92.37% | |||
| Nat'l Total | 3345 | 40482 | 43827 | 7.63% |
Table 1:
Autopsies were recorded for 7.4% of all deaths studied. Autopsy rates by treating specialty ranged from a high of 15.7% for the surgery ward to a low of 3.7% for nursing home patients classified by the hospice treating specialty.
Analysis demonstrated statistically significant (p =0.000) differences in autopsy rates in comparing all treating specialties to the general medicine reference group. Patients dying in other acute care treating specialties had a significantly greater chance of having an autopsy performed than those dying on general medicine (surgical ICU O.R 2.10, surgery ward O.R 2.27, medical ICU O.R. 1.45). In contrast nursing home patients were significantly less likely to have an autopsy performed (nursing home O.R 0.74, hospice 0.47).
Table 2 groups treating specialties for comparison with published autopsy rates by venue. The acute care group (autopsy rate 9.5%) includes both ICU and non-ICU acute care. The ICU group includes medical and surgical ICUs (autopsy rate 11.2%) and the nursing home group (autopsy rate 4.3%) includes the nursing home and hospice treating specialties.
| VA Autopsy Rate 2006-2007 | Published Rates |
|---|---|
| Acute Care (inc.ICU) 9.47% | 4.9% 10 21 |
| Intensive Care 11.24% | 33%30, 22.7% 3153% 3245% 16 |
| Nursing Home 4.25% | 0.8%8, 0.6-8% 10 |
Table 2: Autopsy Rates Comparison to Published Rates.
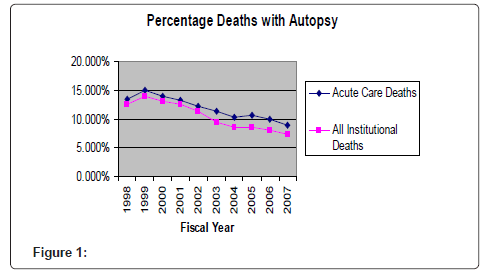
The autopsy rate in the VA shows a consistent downward trend in recent years. The national autopsy rate in acute care decreased from 13.4% in fiscal year 1998 to 9.0% in fiscal year 2007, a decline of 33% (p= 0.000 R2 0.88). The overall institutional autopsy rate (acute care plus nursing home & hospice) decreased from 12.5% in 1998 to 7.3% in 2007, a decline of 42% (p=0.000, R2 0.90).
Discussion
The results demonstrate significant variation in autopsy rates by treating specialty and institutional venue with dramatically lower autopsy rates in nursing homes. In the literature the highest autopsy rates have been reported in ICU and acute care settings with very low autopsy rates reported in nursing homes [8,10]. Overall, these VA rates are higher than commonly published values in the private sector for both acute care and nursing homes [10]. The ICU autopsy rate is lower than rates in cited publications. However, autopsy rates for ICUs cited in Table 2 represent individual facility rates in academic medical centers and are likely biased toward higher rates than in the community, reflecting what appear to be strong facility-specific mandates to inquire about and obtain autopsies. The VA nursing home autopsy rate, while low, is more than 7 times higher than the CDC published autopsy rate of 0.8% (2003), likely as a result of better access to and support of autopsy services in VA nursing homes [10]. As in the private sector, autopsy rates have declined significantly as compared to historical norms and this decline appears to be continuing in recent years.
These results are not surprising. Higher autopsy rates have been correlated with unexpected death and younger age [10,11] and thus one would expect to find higher rates in acute care as compared to the nursing home. In a system like the VA which encourages/requires autopsy requests and in which autopsies are performed at no cost to families, one would expect to find higher autopsy rates than in the private sector. The hospital autopsy rate is still remarkably low relative to historic norms. In 1964 the national hospital autopsy rate was 41%, falling to 15% in 1983 [12]. By 1994 a survey of national hospitals revealed that 50% had autopsy rates at or below 8.5% [13].
These results suggest that having an autopsy performed appears to be highly dependent upon where a person dies, despite the facts that in the VA system access to autopsy services is readily available to all patients dying as inpatients. While not surprising, this is disturbing. We do not presume to know what proper autopsy rates might be. The literature reviewed, while largely calling for more autopsies, is remarkably lacking in providing any standards by which autopsy rates might be evaluated in terms of appropriateness. From a palliative care perspective, we would hope that rates obtained by facilities would reflect first and foremost patient and family preferences for autopsies and secondarily the potential value of autopsies to contribute to medical knowledge. Both of these factors would seem only weakly correlated with where a person dies.
While much attention has focused on why individuals might decline autopsies, inadequate attention has been paid to reasons why patients and families might desire an autopsy. Three major reasons patients and families might desire autopsies stand out: 1) to resolve any diagnostic uncertainty and to confirm the appropriateness of actions taken [14], 2) to evaluate for occult disease, such as heart disease, dementia, and cancer, that might suggest a genetic risk to descendents [14,15], and 3) as an altruistic contribution to medical science [9]. From this perspective inquiry about autopsy is less a matter of consent for something the physician desires and more a matter of eliciting personal and family care preferences, a tenant to which palliative care strongly subscribes.
This study is limited in that we did not attempt to control for other variables that might influence the probability of having an autopsy performed - disease process, circumstances of death, decedent demographics, academic status of medical centers, and patient and family preferences regarding autopsy [10,11]. More importantly, we have no idea how many patients or families were actually counseled regarding autopsy as an option. Most relevant literature cites only autopsy rates, not the percentage of patients or families who were approached and counseled, even though permission for an autopsy must be granted, except where required by a medical examiner [10]. While some studies cite reasons families might decline an autopsy, arguably the more important statistic is how often they were actually asked and accepted and perhaps even how they were asked [14,16]. A recent study by Combes and colleagues suggests that, when asked, a high percentage of families actually agree to autopsies [17].
Three major reasons have been suggested for declining rates of inquiry regarding autopsy - a change in accreditation requirements for autopsies, associated cost burdens, and the changing role of pathologists [4,7,8,10,18]. While acknowledging the probable importance of these factors, we believe greater attention to education and system issues regarding autopsy inquiries could make a significant difference in ensuring that preferences are respected and autopsies remain a vital component of medical care. Palliative care clinicians can and should play an important role in this.
Studies of medical students and residents have generally found that trainees acknowledge the value of autopsies, but also are reluctant to make inquiries. Attitude surveys have found that trainees find the task unpleasant, are concerned with upsetting families, and believe they have been inadequately prepared to conduct inquiries and answer family questions [19,20]. Sherwood and colleagues in a survey of practicing physicians found that few had any formal instruction in how to inquire about an autopsy [21].
Significant efforts have been made in the hospice and palliative care literature regarding how best to communicate bad news and deal with other difficult encounters with patients and families at the end-of-life. However, the topic of communication skills regarding inquires about autopsies has been almost completely neglected [22]. Further curriculum development in this area is clearly needed and further research is needed on the impact of training on autopsies both quantitatively and qualitatively.
If inquiry about autopsy as a patient and family option should be the standard of care (as compared to pushing for or obtaining some percentage of autopsies as previously required by the JCAH), then, as McPhee noted in an article over a decade ago, this will only happen if major changes occur in processes surrounding inquiries, autopsy procedures, and family follow-up [23]. While a detailed discussion of such changes is beyond the scope of this report, we highlight below some specific issues that would need to be addressed:
• When should an inquiry be made? Must inquiries be postmortem? Given that most modern deaths can be anticipated, should inquiries be made to the extent possible prior to death?
• Who should be asked? Should competent, terminally ill patients be asked about autopsy as an option or should permission remain the responsibility of next-of-kin?
• Who should be responsible for making inquiries and who should be responsible for ensuring reasonable rates of inquiry? Must this be done by solely by physicians? Veterans Affairs facilities have administrative personnel responsible for managing decedent affairs. Greater involvement by trained administrative staff in inquiries regarding autopsies might be an effective way to improve compliance with regulations and reduce variance among venues.
• Establish standards by venue for autopsy inquiries and track the percentage of deaths in which an inquiry was possible and made through quality assurance activity.
• Development of educational materials, which would summarize potential benefits (and possible burdens) of autopsies both to the family and the healthcare system in a balanced manner.
• Establish a mechanism for communicating and interpreting autopsy results to family members and answering their questions.
• Ensure that both inquirers regarding autopsy and clinicians (pathologists and others) who will communicate results to family members are competent in their communication skills.
Summary
In comparison to the private sector autopsy rates in the VA are higher, but still low relative to historical norms. Significant variance exists in autopsy rates by treating specialty and venue of death. If patient and family preferences regarding autopsy are to be honored and if we as a society are to fully benefit from autopsies, significant changes in education and processes regarding autopsy inquiry must take place. While this study focused on autopsy rates, we suggest that future work in palliative care address how best to honor patient and family preferences regarding autopsies.
Acknowledgements
The authors’ work is supported by the VA Palo Alto Health Care System.
References
- McPhee SJ, Bottles K (1985) Autopsy: moribund art or vital science? Am J Med 78: 107-113.
- Brooks JP, Dempsey J (1991) How can hospital autopsy rates be increased? Arch Pathol Lab Med 115: 1107-1111.
- Start RD, McCulloch TA, Benbow EW, Lauder I, Underwood JC (1993) Clinical necropsy rates during the 1980s: the continued decline. J Pathol 171: 63-66.
- Hasson J, Schneiderman H (1995) Autopsy training programs. To right a wrong. Arch Pathol Lab Med 119: 289-291.
- Esteban A, Fernandez-Segoviano P (2003) Is autopsy dead in the ICU? Intensive Care Med 29: 522-525.
- Jeganathan VS, Walker SR, Lawrence C (2006) Resuscitating the autopsy in Australian hospitals. ANZ J Surg 76: 205-207.
- Nemetz PN, Ludwig J, Kurland LT (1987) Assessing the autopsy. Am J Pathol 128: 362-379.
- Katz PR, Seidel G (1990) Nursing home autopsies. Survey of physician attitudes and practice patterns. Arch Pathol Lab Med 114: 145-147.
- VHA Directive 2011-019 (2011) The autopsy as a critical component of quality management.
- Hoyert D, Kung H, Xu J (2007) Autopsy patterns in 2003. National Center for Health Statistics. Vital Health Stat 20.
- Nemetz PN, Leibson C, Naessens JM, Beard M, Tangalos E, et al. (1997) Determinants of the autopsy decision: a statistical analysis. Am J Clin Pathol 108: 175-183.
- (1987) Autopsy. A comprehensive review of current issues. Council on Scientific Affairs. JAMA 258: 364-369.
- Zarbo RJ, Baker PB, Howanitz PJ (1996) Quality assurance of autopsy permit form information, timeliness of performance, and issuance of preliminary report. A College of American Pathologists Q-Probes study of 5434 autopsies from 452 institutions. Arch Pathol Lab Med 120: 346-352.
- Oppewal F, Meyboom-de Jong B (2001) Family members' experiences of autopsy. Fam Pract 18: 304-308.
- Meert KL, Eggly S, Pollack M, Anand KJ, Zimmerman J, et al. (2007) Parents' perspectives regarding a physician-parent conference after their child's death in the pediatric intensive care unit. J Pediatr 151: 50-55.
- Rosenbaum GE, Burns J, Johnson J, Mitchell C, Robinson M, et al. (2000) Autopsy consent practice at US teaching hospitals: results of a national survey. Arch Intern Med 160: 374-380.
- Combes A, Mokhtari M, Couvelard A, Trouillet JL, Baudot J, et al. (2004) Clinical and autopsy diagnoses in the intensive care unit: a prospective study. Arch Intern Med 164: 389-392.
- Lemaire F (2003) Should the autopsy be resuscitated? Intensive Care Med 29: 518-521.
- Hull MJ, Nazarian RM, Wheeler AE, Black-Schaffer WS, Mark EJ (2007) Resident physician opinions on autopsy importance and procurement. Hum Pathol 38: 342-350.
- Girgis A, Sanson-Fisher RW, McCarthy WH (1997) Communicating with patients: surgeons' perceptions of their skills and need for training. Aust N Z J Surg 67: 775-780.
- Sherwood SJ, Start RD, Birdi KS, Cotton DW, Bunce D (1995) How do clinicians learn to request permission for autopsies? Med Educ 29: 231-234.
- Hallenbeck J (2005) Palliative care in the final days of life: "they were expecting it at any time". JAMA 293: 2265-2271.
- McPhee SJ (1996) Maximizing the benefits of autopsy for clinicians and families. What needs to be done. Arch Pathol Lab Med 120: 743-748.
- Dimopoulos G, Piagnerelli M, Berre J, Salmon I, Vincent JL (2004) Post mortem examination in the intensive care unit: still useful? Intensive Care Med 30: 2080-2085.
- Pastores SM, Dulu A, Voigt L, Raoof N, Alicea M, et al. (2007) Premortem clinical diagnoses and postmortem autopsy findings: discrepancies in critically ill cancer patients. Crit Care 11: R48.
- Ferguson RP, Burkhardt L, Hennawi G, Puthumana L (2004) Consecutive autopsies on an internal medicine service. South Med J 97: 335-337.
- Sanner M (1994) A comparison of public attitudes toward autopsy, organ donation, and anatomic dissection. A Swedish survey. JAMA 271: 284-288.
- Charlton R (1994) Autopsy and medical education: a review. J R Soc Med 87: 232-236.
- Welsh TS, Kaplan J (1998) The role of postmortem examination in medical education. Mayo Clin Proc 73: 802-805.
- Schneiderman H, Gruhn J (1985) How--and why--to request an autopsy. Postgrad Med 77: 153-156, 160-164.
- Sherwood SJ, Start RD (1995) Asking relatives for permission for a post mortem examination. Postgrad Med J 71: 269-272.
- Nadrous HF, Afessa B, Pfeifer EA, Peters SG (2003) The role of autopsy in the intensive care unit. Mayo Clin Proc 78: 947-950.
- Tai DY, El-Bilbeisi H, Tewari S, Mascha EJ, Wiedemann HP, et al. (2001) A study of consecutive autopsies in a medical ICU : a comparison of clinical cause of death and autopsy diagnosis. Chest 119: 530-536.
- Shojania KG, Burton EC, McDonald KM, Goldman L (2002) The autopsy as an outcome and performance measure. Evid Rep Technol Assess (Summ) 58: 1-5.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 10514
- [From(publication date):
May-2012 - Jul 01, 2025] - Breakdown by view type
- HTML page views : 5922
- PDF downloads : 4592