Autoinoculation Versus Intralesional Injection of Bleomycin in the Treatment of Multiple Recalcitrant Warts
Received: 04-Aug-2018 / Accepted Date: 27-Aug-2018 / Published Date: 05-Sep-2018 DOI: 10.4172/2332-0877.1000376
Keywords: Autoinoculation therapy; Bleomycin; Multiple recalcitrant warts
Introduction
Warts are polymorphic lesions that affect different areas of the skin and mucous membranes. They are caused by the human papilloma virus (HPV). There are different types of warts including common warts, filiform, digitiform, plane, plantar and genital warts. There are few population-based studies on the prevalence of non-genital warts. Two large population-based studies found prevalences rates of 0.84% in USA and 12.9% in Russia [1].
In Egypt there is a cross sectional study that assessed the prevalence of common warts of hands in rural primary school for children in Dakahlia governorate. The prevalence was 2.3% [2]. Regarding genital wart, a multicenter observational study was done in Egypt. The conclusion of this study was that the prevalence of genital wart in Egypt was 10.4% and that of genital warts in women aged 45-54 years was 9.2% [3].
warts include functional impairment, cosmetic reasons, and sometimes the risk of malignancy in certain type of warts. Management is difficult, primarily due to recalcitrance to traditional therapy, high recurrence rates, the potential for contagious spread to other sites or to contacts, disfigurement and psychosocial effects. The traditional treatment options include cryosurgery, laser, electrosurgery, podophylline, curettage, and topical keratolytics [5].
These therapeutic modalities destruct the wart without the generation of a specific immunity against HPV. This often leads to recurrence, irritation, pain, scars, and prolonged morbidity (especially in palmoplantar warts). The stimulation of the immune system by exposing the virus to immune mediators forms an ideal modality of treatment due to spontaneous regression of the wart with long-lasting immunity. This is called immunotherapy [6].
Diphencyclopropenone (DCP), squaric acid dibuty ester (SADBE), candida antigen, imiquimod, tuberculin jelly and different viral vaccines were used, and none has been consistently standard [5].
Autoinoculation is a novel, inexpensive and effective procedure which treats the warts by stimulating an immune response against HPV. As it is an autograft technique, it is more likely that immunity against the same genotype is elicited (in contrast to the HPV vaccine where immunity is developed only against HPV 6, 11, 16 and 18). This is done by excision of the full thickness warty tissue and implanting it in a dermal pocket made in uninvolved skin [7].
Bleomycin is an anticancer drug that is derived from Streptococcus verticillus. It inhibits cell cycle at G2 phase and causes destruction of the tumor cells by DNA fragmentation, RNA degradation, and simultaneous free radicals’ production. Systemic use of this medication with a dose higher than300mg / day shows more toxic effects on lung and skin and so is not considered as the first choice in the treatment of warts [8].
Intralesional bleomycin injection was reported to be effective in treatment of warts either by injection into the lesion by syringe or using dermojet or prick method [9]. The effect of bleomycin injection in resistant warts has been evaluated in several studies. In some studies, this treatment has been rejected [10], others show that the healing rate was14% to 99% [11].
Materials and Methods
This intervention study (pre - post intervention) involved 50 patients with multiple recalcitrant warts. Patients were randomized selected from the outpatient clinic of dermatology, venereology and andrology department. They were divided into two groups. Group A (25 patients) received treatment with the autoinoculation procedure, and group B (25 patients) treated with intralesional bleomycin injection. The institutional review board (IRB) approval of this study had been assigned number 3412 on 14/2/2017.
Inclusion criteria included patients with multiple recalcitrant warts at different sites, with ages ranged from 18 – 45 years and both sexes.
Exclusion criteria included patients having other dermatological diseases, with mucosal warts, immunosuppressed ones, patients with koebner phenomenon, HCV or HIV infections. Those on aspirin or anticoagulant therapy and with bleeding tendency. Patients with lung diseases (in bleomycin treated group). Pregnant and lactating females and children were also excluded.
Written informed consents were obtained from the patients participating in this study after informing them about the steps of study and the complications.
All patients were subjected to detailed history taking including personal history, family history of similar conditions, past history of previous medication, and medical history regarding any dermatological, lung, blood diseases. General and dermatological examinations were also done for all patients.
Group A patients who treated with autoinoculation procedure were subjected to the followings:
1) A digital photograph was taken for the multiple warty lesions before treatment.
2) The procedure was done under strict aseptic conditions.
3) A wart with a considerable volume was chosen as the donor and was anesthetized by lignocaine infiltration. It was shaved with a 15- scalpel blade. Haemostasis was done using a high frequator electrocauterization.
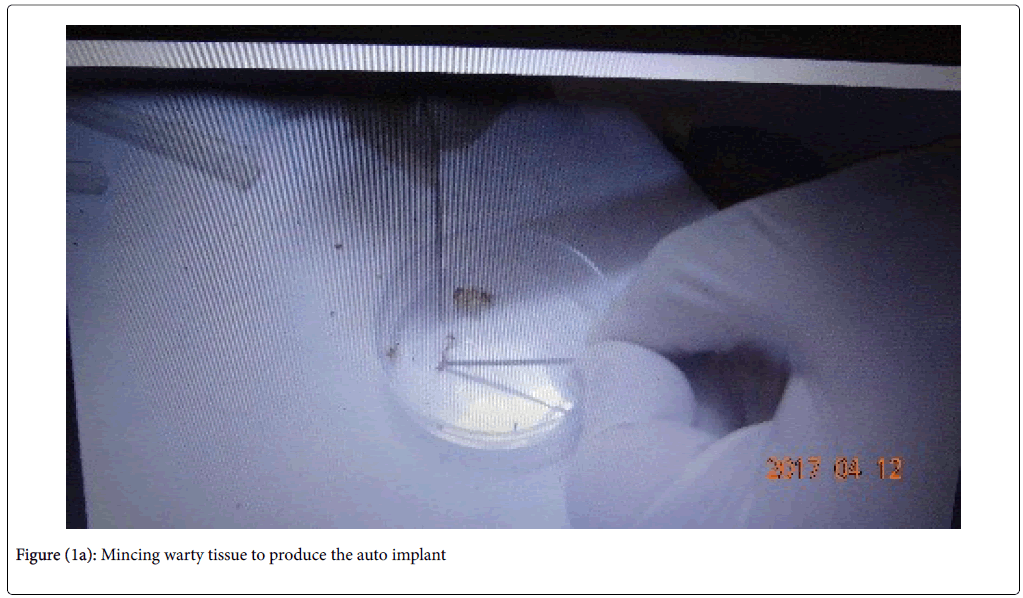
4) The tissue from the donor wart was put in a petri dish and minced in to tiny bits (fig 1a and 1b).
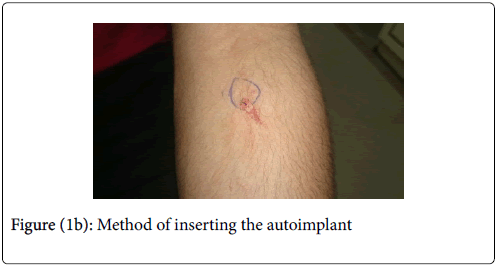
5) Using a 20gauge needle, a dermal pocket extending to the subcutis was formed over the volar aspect of the left forearm of the same patient with prior anaesthesia infiltration.
6) The minced bits of the donor wart were introduced in to the dermal pocket in the left forearm with the tip of the 20-gauge needle that used before (figure 1b).
7) Both donor and recipient site were dressed in gauze and adhesive plaster and patients were asked not to remove the plaster except after 5 days of this procedure. systemic antibiotics were given to patients (cefradine 500mg three times daily and metronidazole 500mg twice daily for one week after the procedure) to guard against secondary bacterial infection.
8) The follow up visits were scheduled every 4 weeks for 3 months. At each follow up visits the procedure was repeated using a different donor wart.
9) A digital photograph of the warts was taken every 4 weeks.
Group B patients who treated with intralesional injection of bleomycin were subjected to the followings:
1) A digital photograph was taken for the wart treated before starting this therapeutic option.
2) Each bleomycin vial contains 15 mg in dry form, each milligram contains 1.5 to 2 units of active bleomycin. Each vial was dissolved with 5 ml distilled water, thus each ml contained 3mg of the drug. Then we mixed 1 ml of the solution with 2 ml lidocaine 1% so that each ml contained 1 mg of the drug.
3) Injection was done by insulin syringe directly in to wart, until the color of the lesion turned in to white. In small wart, injection was with a dose of 0.1 ml of the final solution as one injection point. In large warts, injection was with a dose not exceed 0.2 to 0.3 ml of the final solution in multiple injection points. The maximum total dose for each patient per session was less than 2 mg.
4) The session was repeated every 4 weeks for 3 months.
5) Digital photographs of warts were taken every 4 weeks.
Results
The demographic data of the two groups showed that there were no statistically significant differences between the two studied groups in age or sex distribution. There were no statistically significant differences between the two studied groups in duration or previous therapy of warts. Regarding the type and site of warts treated in this study, there was a statistically significant increase in frequency of common warts (as a type) and two hands warts (as a site) among autoinoculation group compared to bleomycin group.
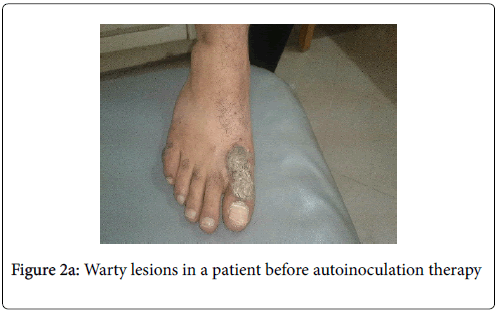
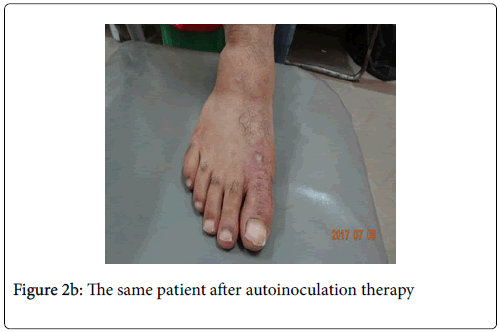
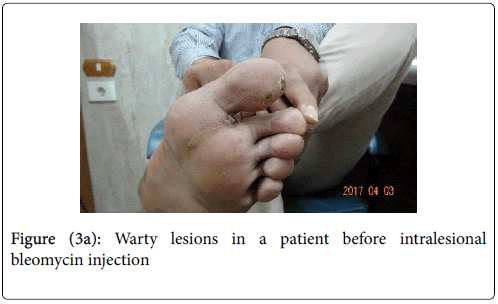
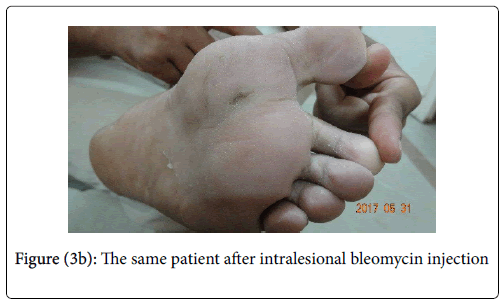
Regarding the number of warts at baseline session and the follow up sessions in both groups, there were no statistically significant differences between the two studied groups in number of warts at baseline or after 1st, 2nd or 3rd sessions. But there was highly statistically significant decrease in number of warts in each group when comparing baseline with 3rd session. The clinical complete response of the manipulated warts after the 3 sessions was 44% and 40% in bleomycin group and autoinoculation group respectively (fig 2a,2b, 3a, 3b).
A remote clearance of non-manipulated warts was achieved in 28% in bleomycin group and in 40% in autoinoculation group with no statistically significant differences between the two studied groups. It was found a statistically significant increase in frequency of nonresponders in autoinoculation group compared to bleomycin group. Itching was a predominant sign in patients treated with autoinoculation procedure with 100% of the autoinoculation group complained of itching at the recipient (injection ) site and 40% complained of generalized itching. There was statistically significant increase in frequency of itching in site of injection and in remote sites in autoinoculation group compared to bleomycin group. It was noticed that 60% of patients treated with intralesional bleomycin injection had experience pain at injection site that subsided 24 hours after injection. There was a statistically significant increase in frequency of generalized itching in completely responded cases. On the other hand, all the cases with remote response had generalized itching.
In the group A, there were no statistically significant differences between responded and non-responded cases in age or disease duration but there was statistically significant decrease in number of warts and increase in percentage of reduction among responded compared to non-responded cases. Eight patients out of the 10 completely responded patients were presented with number of less than 12 warts at the baseline session.
In group B, there were no statistically significant differences between partial and complete responded and non-responded cases in age or disease duration but there was statistically significant decrease in number of warts and increase in percentage of reduction among partial and complete responded compared to non-responded cases. Nine patients out of the 11 completely responded patients were presented with number of less than 12 warts at the baseline session
Discussion
Multiple recalcitrant warts (more than five warts and resistant to many therapeutic modalities) [12] have a significant morbidity by inducing discomfort both physically and psychologically [13]. Multiple recalcitrant warts treatment may fail to clear the warts even after repeated sessions of various physical therapeutic remedies as electrocautery, cryotherapy, laser or radiofrequency [12]. The present study showed 44% clinical complete response of the manipulated warts after the 3 sessions in bleomycin group. A previous study showed 94.9% complete clearance rate in 39 wart patients treated with bleomycin [14]. This difference may be attributed to the higher concentration of bleomycin used in their study and the larger sample size.
In the present study the clinical complete response of the manipulated warts after the 3 sessions was 40% in autoinoculation group. Other autoinoculation studies showed a higher complete clearance rate as that by 2016 who mentioned that 75% of all the study participants revealed complete clearance of their warts after autoinoculation procedure. This better response may be due to the larger sample size (40 patients) and the modified technique of autoinoculation as they pared only the superficial layers of the wart and reimplanted it subcutaneously rather than taking a fleshy part of the wart (full thickness wart tissue with mincing) as we performed. However, had used autoinoculation procedure with full thickness warty tissue (as we performed) and they showed 62.5% complete clearance rate. The remote response in our study was achieved in 40% in autoinoculation group. This can be explained by inducing a delayed hypersensitivity response to wart antigens of the individual human papilloma virus (HPV)genotype affected each patient individually. This response helping in clearance of both manipulated and nonmanipulated remote warts through T helper 1(Th1) cytokines. These cytokines include tumor necrosis factor alpha (TNFα) and interleukin-1(IL-1) which downregulate the transcription of HPV genes whereas interferon-gamma and interleukin-2(IL-2) direct cytotoxic T cells and natural killer cells to attack HPV infected cells [7].
While the remote response in our bleomycin treated group was reached in 28% of patients involved in this group. Although this finding is not statistically significant but should be considered. This can be explained by an immunologic effect of bleomycin. Bleomycin induces interferon-gamma and CD8+ T cytotoxic cells specific against HPV and also can counteract Foxp3+ regulatory T(Treg) cell proliferation [15].
The non-responders were higher in autoinoculation group (60%). This may be due to many possible causes. One of these causes is the genotype of HPV of the donor wart may differ from the genotype of the not responding warts as the immune response developed after autoinoculation is specific to the genotype of HPV in donor wart and each patient may have multiple different genotypes of HPV producing multiple warty lesions. The other possible cause is that autoinoculation procedure works through one method which is the induction of delayed hypersensitivity reaction, whereas intralesional bleomycin works by multiple arms including the immune responses as well as local antiproliferative effects and reactive oxygen species (ROS)- mediated reticulum stress and autophagy [15]
In this work, itching was noticed as a predominant sign in patients treated with autoinoculation procedure with 100% of the autoinoculation group complained of itching at the recipient (injection) site and 40% complained of generalized itching. There was statistically significant increase in frequency of itching in site of injection and in remote sites in autonoculation group compared to bleomycin group.
There was an increase in frequency of generalized itching in completely responded cases in group (A). We found also that all the cases had remote response had generalized itching.The generalized itching may be a sign of the will developed delayed hypersensitivity reaction. This means that generalized itching may be a predictive sign of the effectiveness of autoinoculation procedure in treatment of multiple recalcitrant warts. To our knowledge, this is the first study to correlate the clinical response of autoinoculation procedure with a sign of itching present in some patients treated with this procedure. In this study, 60% of group B patients complained of pain at injection site that subsided 24 hours after injection. This side effect that was rapidly subsided because of the mixture of local anesthesia with bleomycin. This goes with [16] but they mentioned other side effects as keloid, bullae, Raynaud's phenomenon that were not reported in our study.
The results of this work demonstrated that 9 patients out of the 11 complete responsed patients in bleomycin group were presented with number of less than 12 warts at the baseline session. Also 8 patients out of the 10 complete responded patients in autoinoculation group were presented with number of less than 12 warts at the baseline session. We can state that a more favorable outcome (of both procedures) is predicted when treating patients with multiple warts with their count less than 12. To our knowledge, this is the first study that determine a cutoff number of warts above which the response of the two therapeutic procedures are non-favorable in treating multiple recalcitrant warts. However, [7] noticed that number of warts at baseline didn't affect the degree of reduction in warts (p=0.144). We treated 3 patients with genital multiple recalcitrant warts in this study, two of them treated with intralesional bleomycin injection and one treated with autoinoculation procedure. Unfortunately, none of them showed any clinical improvement by the two procedures. Moreover, the two patients of genital warts treated with bleomycin showed more flare and appearance of new warty lesions without disappearance of the manipulated warts.Within group A, one patient developed an erythematous tender nodule at the recipient site in which the minced warty material was inoculated. This nodule subsided after 48 hours of the procedure following every session. This patient showed complete clinical response with complete clearance of the manipulated as well as the remote non-manipulated warts and this response was recorded from the 1st follow up visit and in the subsequent visits. This may be explained by the development of intense immediate inflammatory reaction in response to a foreign body in the dermis [17,12] mentioned also that only one patient in their study developed an erythematous nodule at implantation site but with purulent discharge and resolved by systemic and topical antibiotics.
Conclusion
Autoinoculation is a novel inexpensive therapeutic modality that is effective in treatment of multiple recalcitrant warts. This effectiveness is achieved better when the number multiple recalcitrant warts is less than 12 warts. Generalized itching following autoinoculation procedure may be a predictive sign of efficacy of this technique.
References
- LOO SK, Tang W. YM (2010) Clinical evidence hand book: Warts (Non-genital). Am Fam- Physician 81: 1008-1009.
- Kasim Kh, Amer S, Mosaad M, Wahed AA, Allam H, et al. (2013) Some epidemiological aspects of common warts in rural school children. ISRN Epidemiology 5: 1-6.
- Shatout MF, Sallam HN, DeAntoin, AbouSeeda M, Moiety F, et al. (2014) Prevalence and type distribution of human papilloma virus among woman older than 18 years in Egypt : a multicenter observational study. Int j infect dis 29: 226-231.
- Sterling J (2004) Virus Infection. In: Burns T, Breathnach S, Cox N, Griffiths CAR editors. Rooks Textbook of Dermatology. Oxford Blackwell 37-60.
- Signore RJ (2002) Candida albicans intralesional injection immunotherapy of warts. Cutis 70: 185-92.
- Venugopal SS, Murrell DF (2010) Recalcitrant cutaneous warts treated with recombinant quadrivalent human papilloma virus vaccine (types 6, 11, 16, and 18) in a developmentally delayed, 31-year-old white man. Arch Dermatol 146: 475-7.
- Lal NR, Sil A, Gayen T, Bandyopadhyay D, Das NK (2014) Safety and effectiveness of autoinoculation therapy in cutaneous warts:A double-blind ,randomized placebo-controlled study. Indian J Dermatol Venereol Leprol 80: 515-520.
- Lewis TG, Nydorf ED (2006) Intralesional bleomycin for warts: a review. J Drugs Dermatol 5: 499-504.
- Agius E, Mooney JM, Bezzina AC, Yu RC (2006) Dermojet delivery of bleomycin for the treatment of recalcitrant plantar warts. J Dermatolog Treat 17: 112–116.
- Pollock B, Sheehan-Dare R (2002) Pulsed dye laser and intralesional bleomycin for treatment of resistant viol hand warts. Lasers Surg Med 30: 135-40.
- Salk R, Douglas TS (2006) Intralesional bleomycin sulfate injection for the treatment of verruca plantaris. J Am Podiatr Med Assoc 96: 220-225.
- Swaroop MR, Sathyanarayana BD, Vasudevan P, Aneesa, Kumari P, et al. (2016) Evaluation of efficacy and safety of modified technique of auto wart implantation in the treatment of multiple,recurrent and recalcitrant warts. Indian J Clinic Exp Dermatol 2: 27-31.
- Ciconte A, Campbell J, Tabrizi S, Garland S, Marks R, et al. (2003) Warts are not merely blemishes on the skin: A study on the morbidity associated with having viral cutaneous warts. Australas J Dermatol 44: 169-73.
- Dhar SB, Rashid MM, Islam AZMM, Bhuiyan M (2009) Intralesional bleomycin in the treatment of cutaneous warts:A randomized clinical trial comparing it with cryotherapy. Indian J Dermatol Venereol Leprol 75: 262-267.
- Bugaut H, Bruchard M, Berger H, Derangère V, Odoul L, et al. (2013) Bleomycin experts ambivalent antitumor immune effect by triggering both immunogenic cell death and proliferation of regulatory T cells. PLoS One 8: e65181.
- Laura K, Saggar V, Akhavan A, Patel P1, Umanoff N, et al. (2015) Intralesional bleomycin for warts: Patient satisfaction and treatment outcome. J Cutan Med Surg 19: 470-476.
- Nischal KC, Sowmya CS, Swaroop MR, Agrawal DP, Basavaraj HB, et al. (2012) A novel modification of the autoimplantation therapy for the treatment of multiple,recurrent and palmoplantar warts. J Cutan Aesthet Surg 5: 26-29.
Citation: El-Ghareeb MI, Khater M, Adel A (2018) Autoinoculation versus Intralesional Injection of Bleomycin in the Treatment of Multiple Recalcitrant Warts. J Infect Dis Ther 6:376. DOI: 10.4172/2332-0877.1000376
Copyright: © 2018 El-Gharee MI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4400
- [From(publication date): 0-2018 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 3588
- PDF downloads: 812