Augmentation of Conventional Medicine for Post-concussion Syndrome with Cognitive Behavioral Therapy Accelerates Symptomatic Relief in Affected Individuals
Received: 01-Jan-2022 / Manuscript No. nctj-22-51516 / Editor assigned: 03-Jan-2022 / PreQC No. nctj-22-51516 (PQ), / Reviewed: 17-Jan-2022 / QC No. nctj-22- 51516 / Revised: 22-Jan-2022 / Manuscript No. nctj-22-51516 (R) / Accepted Date: 18-Jan-2022 / Published Date: 31-Jan-2022 DOI: 10.4172/nctj.1000111
Abstract
Post-concussion syndrome (PCS) is a clinical term used to point out the complicated combination of physical, emotional, cognitive and behavioral signs and symptoms associated with Mild Traumatic Brain Injury (mTBI). This study was conducted to assess the improvement or debilitating effect of behavioral therapy in addition to the conventional treatment and to document these results for increasing the efficiency of treatment provided to such patients. This study was primarily an interventional prospective cohort which was conducted in the department of neurosurgery,Allama Iqbal Medical College. Sample size was set at 200 patients which were randomly distributed into 2 groups. Interventional group with Cognitive behavioral therapy added in addition to conventional treatment regimen and the Control group receiving only conventional treatment. Results were noted initially as well as after two weeks of follow up period. Data was analyzed using Statistical Package for Social Sciences (SPSS) Among the patients that were given therapy sessions along with conventional medicine, there was significant improvement in the symptoms and their
overall quality of life. It is also important to notice that the time period taken for these effects to wane was cut down by psychiatric solutions too. So, we can conclude that CBT sessions not only speed up recovery in patients of postconcussion syndrome, they also aid in efficient improvement in functional capability and quality of life.
Keywords: Post-concussion syndrome; Cognitive Behavioral therapy; Psychiatric therapy
Keywords
Post-concussion syndrome; Cognitive Behavioral therapy; Psychiatric therapy
Introduction
Post-concussion syndrome is a neurocognitive disorder that is expressed as a combination of cognitive and behavioral as well as physical symptoms that arise after trauma to the head and brain [1]. Head ache, dizziness and cognitive disorders are more common. While PCS often undergoes resolution within initial weeks of injury for a significant number of people, some patients have extended and even negative recovery course which has been recorded in many instances [2]. Each year, around 60-70 million people worldwide are assessed to suffer from a Traumatic Brain Injury (TBI) with roughly 80% of these cases analyzed as a mild TBI (mTBI), interpreted as scoring 13–15 on Glasgow Coma Scale (GCS). The real prevalence is hard to determine as many individuals with mTBI or concussion, do not pursue medical attention. About 10-16% of patients undergo persistent symptoms 3-months post-concussion, cited to as Post-Concussion Syndrome (PCS). There are no rigid biomarkers for detecting this condition, but progressive neuroimaging tools such as Diffusion Tensor or Weighted Imaging (DTI/DWI) or functional MRI (fMRI) can observe subtle changes in the anatomy of white matter tracts or brain activity, respectively. The majority of patients document acute headache that modifies with time, there may be cases in which persistent PCS would indicate significant disability, especially if patients also have medication overuse headache (MOH). Furthermore, it also requires a substantial direct and indirect financial cost as a result of adverse impact of PTH on patients’ work life and daily life actions. Current acute pharmacological treatments for PTH include nonsteroidal anti-inflammatory drugs, triptans, and antiemetics (i.e., metoclopramide, prochlorperazine, and ondansetron) and peripheral nerve block, whereas tricyclic antidepressants and anticonvulsants have been known to prevent PCS. Available data on pharmacological approaches are based on low-quality studies that show modest response, poor adherence, and compliance due to side effects, and a significant risk of developing MOH in patients with daily symptoms attributed to TBI or whiplash. A very recent systematic review on pharmacological treatment of mTBI burden found a limited number of high-quality, clinically meaningful studies, particularly among children and individuals in the acute stage of injury, hampering an evidence-based analysis that would inform clinical decision-making. Cognitive-behavioral therapy (CBT) and repetitive transcranial magnetic stimulation (rTMS) appear to be the most promising approaches for PCS. A review on behavioral treatments for PTH reported promising data on multimodal interventions including CBT, biofeedback, progressive muscle relaxation, acupuncture, and physical therapy, but underscored the limited evidence on individual non-pharmacologic interventions, and the paucity of randomized clinical trials. A more recent systematic review on behavioral therapies and mind–body interventions for PTH and PCS yielded few good quality studies and high heterogeneity in study populations (i.e., general population, military and veteran staff), methodology, and findings, impeding a conclusion on the real clinical relevance of non-pharmacological interventions. This research article meant to formulate and integrate clinical findings in mild Traumatic Brain Injury (mTBI) around three focal areas of significance relevant to psychological and medicinal therapies for post-concussion symptoms (PCS). These are the relative paucity of symptom specificity, the apparent extent to which subjective cognitive difficulties predominate around the globe, and the role of psychological (especially cognitivebehavioral) processes in the development and stabilizing as well as resolution of presenting symptoms [3,4]. Former researches guiding cognitive behavioral therapy (CBT) for near or absolute similar symptoms in other clinical groups were considered in connection to PCS, as well as some of the practical considerations and approval in application and analysis of CBT with this study group. Existing and unique research issues were identified and studied, including the opportunities, Risks and efficacy of conjoining CBT and cognitive rehabilitation processes precisely [5].
Cognitive behavioral therapy
It’s usually short-term purpose-oriented psychotherapy treatment that takes a practical and consistently modifiable direct approach to mental health issues. Its goal is to change or influence the way of thinking or behavior that are nearly always, causative to people’s difficulties and so change the way they feel about any particular thing or in general. It focuses on the thoughts, images and attitudes that are held by people over an extended period of time. For all the process, sessions were arranged and delivered by the specialist and included psych education regarding TBI; strategies to improve sleep, fatigue, headaches, and tension; and Resolution based cognitive strategies in the areas of prospective memory, attention percentage, learning and memory, and executive higher mental functioning [6]. We also identified and analyzed the potential confounders that seemed to interfere with diagnosis and prognosis of post-concussion syndrome following traumatic brain injury. These were listed as narcotics in the emergency department, psychotropic medication, psychiatric diagnosis, alcohol consumption near time of admission, and preadmission narcotic prescription [7].
Objective
Assess the overall tolerability, viability and efficiency while calculating the treatment effect of Cognitive Behavioral therapy (CBT) delivered after traumatic brain injury to patients for symptomatic relief of chronic Post-Concussion Syndrome (PCS) along with medicinal solutions [8].
Method
It was a six months cross-sectional study conducted at DEPARTMENT OF NEUROSURGERY, Allama Iqbal Medical College and Lahore. Keeping the population estimate of 500 patients presenting into the department during the 6-month period, confidence level of 95% and margin of error at 5%, as a sample,200 patients were included in this research [9,10]. The technique used for enrollment was simple random sampling with each considered patient having equal chance of being included.
The patients were included into the study on the following criteria
• Patients between the ages of 16-60 years
• Either gender
• Clinically diagnosed case of post-concussion syndrome by a consultant neurosurgeon/neurologist
In the same way, decision to exclude patients from study was made on the basis of
• Patients that were not willing to partake in study
• Children under the age of 16 years were excluded from the study
• Patients manifesting serious life-threatening illness were not considered
In this study that lasted six months, various patients with diagnosed post-concussion syndrome were included. The conventional medicine was administered as per routine that included selective serotonin re uptake inhibitors (SSRI’S), Dopamine agonists, Analgesics, anticonvulsant and steroids for symptomatic treatment was added to the treatment of these patients which initially amounted to sessions conducted by therapists. It included strategies to improve sleep, fatigue, headaches, and anxiety; and compensatory cognitive strategies in the areas of prospective memory, attention percentage, learning and memory, and executive higher mental functioning. Comparative Psychotherapy Process Scale (CPPS) was used in study to analyze the effectiveness of CBT and the results were distributed in mild, significant and very significant domains primarily based on improvement of symptoms and the severity that was documented on basis of DSM-5 [11,12].
Result
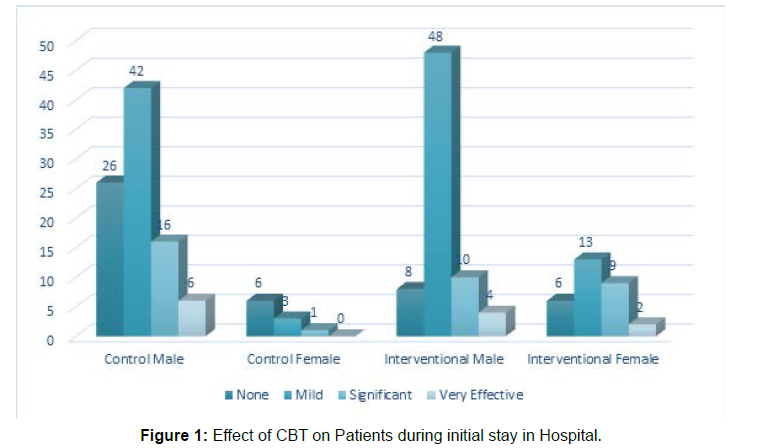
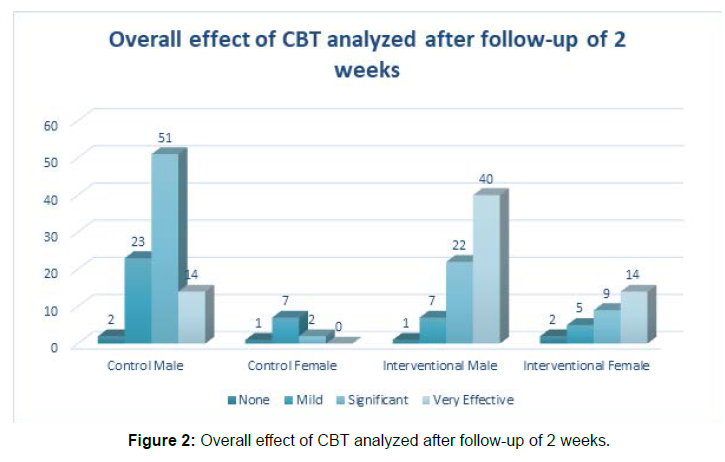
A total of 200 patients were included in the research. They were randomly distributed into 2 groups of 100 patients each. One of these groups (control) was given medicinal treatment while the other group (interventional) was exposed to CBT as well as conventional medicine. The calculated mean age was 38.4_+ 8.6 years. The intensity of mental symptoms and their severity was divided into mild, moderate, severe and very severe or profound according to the Diagnostic and Statistical Manual of Mental Disorders 5th Edition (DSM-5) published by American Psychiatric Association for categorizing disorders. The effect of CBT and overall results are presented in the tables (Tables 1-3) and (Figures 1 and 2).
| Loss of consciousness; n (%) | Cognitive disabilities; n (%) | Behavioral changes; n (%) | |
|---|---|---|---|
| Male | 42 (21) | 62 (31) | 56 (28) |
| Female | 8 (4) | 18 (9) | 14 (7) |
Table 1: PCS predominant symptoms in the sample patients.
| Effect | Control group n | Total N (%) |
Intervention group n | Total n (%) | ||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| None | 26 | 6 | 32% | 8 | 6 | 14% |
| Mild | 42 | 3 | 45% | 48 | 13 | 61% |
| Significant | 16 | 1 | 17% | 10 | 9 | 19% |
| Very effective | 6 | 0 | 6% | 4 | 2 | 6% |
Table 2: Effect of CBT on patients during initial stay in hospital.
| Effect | Control group n |
Total n (%) | Intervention group n |
Total n (%) | ||
|---|---|---|---|---|---|---|
| Male | Female | Male | Female | |||
| None | 2 | 1 | 3% | 1 | 2 | 3% |
| Mild | 23 | 7 | 30% | 7 | 5 | 12% |
| Significant | 51 | 2 | 53% | 22 | 9 | 31% |
| Very effective | 14 | 0 | 14% | 40 | 14 | 54% |
Table 3: Overall effect of CBT analyzed after follow up of 2 weeks.
Discussion
PCS can be a source of distress and disability following traumatic brain injury. These symptoms can be viewed as difficult to treat but vulnerable to psychological approaches. [13] Among the symptoms, cognitive defects were the most prominent with 40% of all patients exhibiting symptoms. This was followed closely by behavioral changes seen in 35% of patients. By executing a modifiable and tailored careful intervention technique, patients report feeling elated and in control and when asked, describe having higher sense of stability and mental efficiency. [14] CBT was first developed as an individual treatment for depression, and it has been shown to improve mood disorders, anxiety disorders, bulimia, and alcohol use disorders and in this case, it was applied to traumatic brain injury patients. [15] Improvements associated with CBT were detected on the mainstay outcome measures relating to quality of life spent by the patient. Improvements were more obvious and clinically detectable for those completing CBT sessions over a brief period of time than taking a longer course, but were not related in any sense to medico legal status, injury severity or length of time that had passed since injury. [16] All the patients in both groups were ensured to have received usual therapeutic and symptomatic medicines as routine with no breaks or planned or unplanned drops. During the initial stay in the hospital that amounted to hours and a few sessions, majority of the patients (61%) experienced mild improvement in the symptoms of PCS with some of them (25%) even progressing into the significant scale. After the completion of sessions that culminated in the assessment of effects at the end of follow-up of two weeks, significant improvement was noted as compared to the patients not given psychological solutions as well as the conventional medicine. A total of 85% of the patients in interventional group had significant reduction in the symptoms of PCS and substantial improvement in the quality of life. The results are supported by similar outcomes in the study that was conducted on military veterans who experienced distress and anxiety [17]. Early diagnosis and treatment of PCS and anxiety may significantly increase the levels of functioning of patients with TBI. Bornstein et al. Supported the positive relationship between neuropsychological distress and emotional disorders with CBT in patients with closed head injury. Further, Williams, Rapport reported that prognosis was positively related to social integration and negatively correlated with emotional disorders. Additional studies are required to elucidate and integrate these associations.
Before reaching the conclusion, we have to take into light, the limitations of this study to effectively assess the degree of impact it is going to have in the domains of mental health and treatment. Although there are documented disparities in provisioning access, continuation and quality of treatment as bias, it is somewhat off putting to infer solely from the presence of or absence of these disparities. To avoid overlooking the problem and any futile attempts at finding solutions, we must consider explanations along with bias in investigation. Socioeconomic status affects the amount of stress a patient has and his passage to healthcare facilities and effectiveness of the treatment being received. It appears that even after economic and financial barriers have been removed, there is still a considerable amount of limitation in the form of lack of adequate familiarity with mental illness concepts, likelihood for interpreting mental health problems in superstitious or other culturally defined terms, social stigma, and tolerant habits that emphasize self-reliance and family reliance instead of seeking professional psychiatric solutions.
Conclusion
The current study concludes that CBT can improve quality of life as overall for adults with persistent PCS and potentially accelerate symptomatic relief for affected individuals when added with conventional medicine resulting in desirable treatment objective.
Disclaimer: None to declare.
Conflict of Interest: None to declare.
Funding Disclosure: None to declare.
References
- Hauptmann LK & Ashkanian M(2017 Nov) Post-concussion syndrome is a neuro-cognitive condition Ugeskr Laeger 179
- Al Sayegh A, Sandford D & Carson AJ (2010) Psychological approaches to treatment of post concussion syndrome: a systematic review. J Neurol Neurosur Ps 81:1128-1134.
- Potter S, Brown RG (2012)Cognitive behavioral therapy and persistent post-concessional symptoms: integrating conceptual issues and practical aspects in treatment Neuropsychol Rehabil 22:1–25
- Twamley EW, Jak AJ, Delis DC, Bondi MW& Lohr JB (2014)Cognitive Symptom Management and Rehabilitation Therapy (CogSMART) for veterans with traumatic brain injury: pilot randomized controlled trial J Rehabil Res Dev 51:59–70
- Silverberg ND, Hallam BJ, Rose A, Underwood H, Whitfield K, et al.(2013) Cognitive-behavioral prevention of postconcussion syndrome in at-risk patients: a pilot randomized controlled trial. J Head Trauma Rehabil 28:313-322.
- Snowden LR (2003) Bias in mental health assessment and intervention: Theory and evidence. Am J Public Health 93:239-243.
- Potter SD, Brown RG & Fleminger S (2016) Randomised, and waiting list controlled trial of cognitive–behavioural therapy for persistent postconcussional symptoms after predominantly mild–moderate traumatic brain injury. J Neurol Neurosurg Psychiatry 87:1075-1083.
- Malone HE, Nicholl H & Coyne I (2016). Fundamentals of estimating sample size. Nurse Res 23:21-5.
- Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW et al(2010) Sample size calculations: basic principles and common pitfalls Nephrol Dial Transplant 25:1388-1393.
- Zimmerman M, Morgan TA & Stanton K (2018)The severity of psychiatric disorders World J. Psychiatry 17: 258-275.
- Lopez MA & Basco MA (2015) Effectiveness of cognitive behavioral therapy in public mental health: Comparison to treatment as usual for treatment-resistant depression Adm Policy Ment Health 42: 87-98.
- Hiltunen AJ, Kocys E &Perrin Wallqvist R.(2013)Effectiveness of cognitive behavioral therapy: An evaluation of therapies provided by trainees at a university psychotherapy training center Psych J, 2:101-112.
- Hsieh MY, Ponsford J, Wong D & McKay A (2012) Exploring variables associated with change in cognitive behaviour therapy (CBT) for anxiety following traumatic brain injury Disabil Rehabil 34:408-415.
- Brunger H, Ogden J, Malia K, Eldred C, Terblanche R et al(2014) Adjusting to persistent post-concussive symptoms following mild traumatic brain injury and subsequent psycho-educational intervention: a qualitative analysis in military personnel Brain Inj. 28:71-80.
- Bradbury CL, Christensen BK, Lau MA, Ruttan LA, Arundine AL et al(2008) The efficacy of cognitive behavior therapy in the treatment of emotional distress after acquired brain injury ARCH PHYS MED REHAB 89:S61-S68.
- Helmick K(2010) Cognitive rehabilitation for military personnel with mild traumatic brain injury and chronic post-concussional disorder: Results of April 2009 consensusconference NeuroRehabilitation, 26:239-255.
- Sheese ALN & Hammeke TA (2014) Rehabilitation from postconcussion syndrome: nonpharmacological treatment Prog Neurol Surg 28:149-160.
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2371
- [From(publication date): 0-2022 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 1849
- PDF downloads: 522