Case Report Open Access
At-Risk EMS Employees: A Model of Assessment and Intervention
Peter Taillac, Ron Hammond*, Kate Miller
Department of Behavioral Science, University of Utah and Utah Valley University, USA
Emergency Medicine, University of Utah and Utah Valley University, USA
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
This paper includes data results from a survey of Utah (U.S.) EMS (Emergency Medical Services) personnel. Those who reported having already reach a point of wanting to quit the field and having reached a point of wanting to resign their current position were classified as being ?At Risk? (N = 142) and were compared to those who had not (N = 395). T-Test and ratio analysis indicated that that ?At Risk? were found to have significantly higher incidences of difficult past calls, PTSD-like symptoms, and a variety of personal hardships. Both groups had relatively high indicators of negative impact of working in the EMS field on their relationships, life satisfaction, and positive job outlook. Arguments are made for implementing a posttraumatic growth model that builds on the Critical Incident Stress Management (CISM) debriefing model and that provides preventative rather than reparative intervention efforts to EMS personnel.
Keywords
EMS, PTSD, posttraumatic growth, CISM
The day-to-day pressures born by Emergency Services Personnel are managed or mismanaged by dispatchers, emergency room professionals, EMT/paramedics, and firefighters alike. These pressures and their accompanying stressors can shorten careers, disrupt personal lives, and contribute to self-destructive conditions if not dealt with appropriately. The traditional notion of stress among emergency professionals had been for years the pathology model of traumatic calls. Stressor pile-up has dominated the literature on the EMS (Emergency Medical Services) professions. A more recent model has emerged since the 1980s called the post-traumatic growth model which is described by Paton (2006):
Since the 1980s, research conducted on the consequences of exposure to traumatic events has witnessed a gradual shift from a focus on their pathogenic nature to a perspective that recognizes the prominent role of positive outcomes in people’s experiences with adversity.
To assume that exposure to adverse events encountered in the course of performing their professional role produces only deficit or pathological outcomes ignores an important reality. Post-traumatic growth describes the outcome explained by Tedeschi (2004) as significant beneficial changes in cognitive and emotional life beyond levels of adaptation, psychological functioning, or life awareness that occur in the aftermath of psychological traumas. (p. 225)
It is safe to assume that most EMS professionals do not fully understand the Post-traumatic Growth model and are also likely entrenched in the pathology model-based way of thinking. This is evidenced by the statement of one former Utah firefighter: “I feel the incident of 9-11 had a larger impact on me than any call I have been on and I think it is a big factor in the emotions of most EMS workers.” Such statements reflect the pathological model and the yet-to-beresolved nature of difficult past calls among those who approach them using the pathological perspective.
Paton (2006) also explained that various studies have shown that “most” eventually benefit from traumatic experience and that there is a “need to identify the resources and processes people bring to bear on their experiences to facilitate growth outcomes” (p. 227). The purpose of this article is to report the findings of a recent Utah EMS survey which was administered statewide in the spring of 2010. In one month 668 respondents provided detailed feedback on the stress, well-being, and overall nature of their careers, including efforts they had made to ameliorate their stressors formally and informally.1 Efforts were made to solicit every county and city EMS system director for their employees’ participation.
From a supervisory perspective the response to two questions was very much a relevant concern. When asked, “Have you ever reached a point of wanting to quit your current EMS role,” 38 percent indicated that they had reached that point. The second question echoes the first, “I sometimes want to resign from EMS altogether” and was agreed to by 26 percent of respondents. This level of departure-desiring behavior could prove to be very taxing on any EMS system with training, talent-loss, and turnover creating undue burdens. A recent national study of EMTs estimated an 11 percent quit rate; about 23 percent of the EMS systems with an attrition problem had no plan in place to deal with it (Williams, 2008.)
Method
This study was approved by two IRB (Institutional Review Board) review boards from Utah Valley University and the Utah State Department of Health. The sampling intention was to solicit responses from every EMS individual working in the state of Utah at the time of the survey. The online survey link was emailed via a snowball sampling technique which included the use of an existing network of Utah CISM volunteers, a newsletter, and through the support of local commanders and chiefs throughout the state. It is estimated that there were approximately 7,000 EMS persons at the time (many were dual licensed as firefighters, EMTs, and other). There were a total of 668 respondents who completed the survey.
The survey was launched online using Qualtrics software and data were collected May-June, 2010. The survey was comprised of 61 questions including: 11 demographic; 2 evaluation of CISM debriefing experiences; 46 asked about their current and past stressors, relationships, well-being, and work experiences; and finally, 2 were open-ended. The results presented in Tables 1 and 2 indicate agreement on one of three types of response scales. Those questions which presented a statement which the respondent would either agree or disagree with used a 5 point Likert-type scale (1 = Strongly Disagree, 2 = Disagree, 3 = Neither Agree nor Disagree, 4 = Agree, 5 = Strongly Agree, and 0 = Does not apply to me). The second type of question presented here was “yes” and “No” (1-Yes and 0 = No).
| Role | # of Times Selected | % of Respondents |
|---|---|---|
| EMS | 510 | 76.3 |
| Firefighter | 443 | 66.3 |
| Other | 53 | 7.9 |
| Public Safety/Law | 40 | 6.0 |
| Hospital ER | 35 | 5.2 |
| Dispatch | 17 | 2.5 |
| Security Officer | 15 | 2.2 |
Table 1: Number of Respondents Identifying Professional Roles (N = 668)
| Measures | Not at Risk % | At Risk% | Ratio |
|---|---|---|---|
| I still suffer physical symptoms that came from exposure to a dangerous call | 1.8 | 12.7*** | 1:7.1 |
| At times I have made self-destructive mistakes in my personal life because of EMS burnout | 6.9 | 31.7*** | 1:4.6 |
| In the last 12 months, I have had thoughts of ending my life | 4.6 | 19.7*** | 1:4.3 |
| I tend to be sick more than most people I know | 3.6 | 14.8*** | 1:4.1 |
| I still blame myself for the negative outcome of a call | 7.6 | 22.5*** | 1:3.0 |
| My EMS stressors have harmed my relationships | 14.5 | 42.3*** | 1:2.9 |
| I suffer from depression | 10.2 | 29.6*** | 1:2.9 |
| My life has an unreasonable level of stress in it | 8.3 | 19.7 | 1:2.4 |
| I have felt call-related PTSD symptoms | 17.2 | 38.7*** | 1:2.3 |
| My work stressors follow me home | 22.3 | 45.1*** | 1:2.0 |
| I’ve increased my alcohol consumption in the last 6 months | 5.6 | 12.3** | 1:2.0 |
| I often worry about being made physically ill because of exposure to diseases at work | 17.9 | 32.4*** | 1:1.8 |
| I feel overburdened by debt | 3.6 | 51.4*** | 1:1.6 |
| I have experienced overwhelming stress on at least one incident in my career | 68.6 | 81.0 | 1:1.2 |
aT-Tests comparisons of means yielded significant differences as indicated by *= 0.05; **= 0.01; and ***= 0.001 levels.
Table 2: Percent Agreement among At Risk and Not At Risk Respondents on Measures of Stressors with Ratio of Not at Risk to At Risk Responses (Not at Risk N = 395, At Risk N = 142) with t-Tests Comparisons of Mean Scoresa
The third type of question was unique to their evaluation of their level of income. “Based on my current needs, my income is… (1 = Inadequate, 2 = Adequate, and 3 = More than Adequate). The percentage in each column of Tables 1 and 2 indicate percent agreement by having selected “Agree or Strongly Agree” and/or having selected “Yes” in response to the respective question. In Table 2 the percentages represent only those who chose “Adequate” to the question on income. The results of these questions and their related importance will be discussed below. Comparisons of means t-Test analysis was used to obtain the results in Tables 1, and 2 while multiple logistic regression was used to obtain the results in Table 3.
| Measures | Not at Risk % | At Risk % | Ratio |
|---|---|---|---|
| Family relationships | |||
| My immediate family is a positive source of support for me in handling my EMS stressors | 76.2 | 73.2 | 1:0.96 |
| I have been overly angry with my family at times because of stressors from my EMS activities | 24.8 | 50.7*** | 1:2.0 |
| Most days of the week my family does NOT sit down for dinner together | 26.1 | 43.0** | 1:1.6 |
| I would consider myself to be a good parent | 72.7 | 76.7 | 1:1.1 |
| Talking to family members about a difficult call makes me feel better | 62.3 | 54.9** | 1:0.88 |
| My spouse and I tend to be very critical of one another | 15.7 | 25.3** | 1:1.6 |
| My spouse and I see way too much defect in one another | 10.3 | 19.0* | 1:1.8 |
| My spouse and I are overly defensive in our relationship together | 14.1 | 21.1* | 1:1.5 |
| My spouse and I withdraw from each other at times | 25.1 | 43.7*** | 1:1.7 |
| Coworker Relationships | |||
| My coworkers are like family to me | 73.9 | 59.1*** | 1:0.80 |
| Talking to other EMS persons about a difficult call makes me feel better | 73.9 | 64.1*** | 1:0.87 |
| I’ve attended a CISM debriefing in the past | 53.7 | 62.7 | 1:1.2 |
| The CISM team is crucial to my success in the system | 29.9 | 24.7 | 1:0.83 |
| If attended CISM debriefing evaluated “Didn’t help much” | 11.0 | 18.0 | 1:1.6 |
| If attended CISM debriefing evaluated “Helped somewhat” | 26.6 | 28.2 | 1:1.1 |
| If attended CISM debriefing evaluated “Helped a great deal” | 16.5 | 16.9 | 1:1 |
| Spiritual and Religious Support | |||
| My personal spiritual practices are a source of strength in my life | 59.7 | 61.3 | 1:1 |
| I consider myself to be very active in my religion | 43.3 | 45.0 | 1:1 |
| My personal spiritual beliefs are a source of strength to me | 59.5 | 64.8 | 1:1.1 |
aT-Tests comparisons of means yielded significant differences as indicated by *= 0.05; **= 0.01; and *** =0.001 levels
Table 3: Percent Agreement Among Not at Risk and At Risk Respondents on Measures of Support (Not at Risk N = 395, At Risk N = 142) with t-Tests Comparisons of Mean Scoresa
The survey was specifically designed to assess the stress experienced by Utah EMS workers and the impact it had on their personal and professional lives. Specifically this study sought to assess the comparative difference between those who had already reached a point of wanting to both quit and resign the profession and those who had not; to predict the chances they had of reaching a point of wanting to quit using multiple logistic regression; and finally to synthesize the findings from this study toward effective and new stress-mediating efforts in the field.
There were two groups of respondents who were identified in this study. First, those who had reach a point of both wanting to quit and a point of wanting to resign from the EMS field. This group was formed by combining those who agreed to both wanting to quit and to resign, yielding 142 Utah EMS workers were identified as being “At Risk” (21% of the total sample). The second category included 395 Utah EMS workers who indicated that they did not want to neither quit nor resign. These were called the “Not at Risk” group (57% of the total sample). Those not fitting these two categories were excluded from this analysis.
The concepts used for this analysis include measures already present in the literature and some that were unique to this survey. Physical health issues were identified as a measure of well-being and as an indicator of potential duress (Blau & Chapman, 2011; Cieslak et al., 2014; Halpern et al., 2008; Haslam & Mallon, 2003; Setti & Piergiorgio 2014).
Results
In this study, quitting and resigning were highly correlated together. By combining those who agreed to both the quitting and resigning questions, “At Risk” personnel were identified (N = 142, 21% of the total sample). Another category of “Not at Risk” respondents were also identified based on those who had disagreed with both the quitting and resigning questions (N = 395, 57% of the total sample). The responses from the At Risk group were statistically compared to those from the Not at Risk group and the results were very insightful. Compared to the Not at Risk category, the At Risk category was slightly older (median age of 43.38 compared to 40.49); had been in their EMS role longer (13.5 compared to 11.76 years); higher percentage of females (29.6% compared to 19.7%); had fewer full-time (57.7% compared to 67.8%); had higher levels of divorce after becoming certified in their current role (21.8% compared to 12.9%, 0.05 significance); and were less likely to report their income as being adequate (47.2% compared to 58.0%, 0.05 significance). Education level, percent married, and number of children were very close between the two groups.
We can compare the stressors and well-being of those At Risk and those Not at Risk by considering key stressor indicator variables asked in this survey. Table 2 shows the details of these 17 measures of stressors between the Not at Risk and At Risk categories with ratios depicting the comparison in relation to one another. In all 17 of the stress measures, the At Risk group scored significantly worse, except in the question “My life has an unreasonable level of stress in it” and “I have experienced overwhelming stress on at least one incident in my career.” For these two questions, the At Risk group scored worse but not significantly worse as measured by t-test comparisons of means. A ratio was developed to contrast the percentages agreeing between the Not at Risk and the At Risk categories.
The Not at Risk-to-At Risk ratios were strikingly diverse on some measures: “Suffering physical symptoms from a dangerous call” was 1:7.1. “Being burdened by unresolved anxieties from a past call” was 1:6.4 while “my levels of stress often exceeding my abilities to handle them” 1:6.0. For those “still suffering psychological symptoms that came from a difficult call,” the ratio was 1:5.7. In each of these categories, the measures are of past and current call stressors that still linger for the respondent.
Of special concern is the self-destructive nature of these stressors in the respondents’ lives. “Making self-destructive mistakes” was 1:4.6; “Thoughts of suicide” had a ratio of 1:4.3 while “being sick more than others” was 1:4.1. Collectively, these represent a dismal outlook for the At Risk category of respondents. The lowest ratio was for “having experienced overwhelming stress on at least one incident in my career” at 1:1.2. This was so close because the majority of all respondents indicated they had experienced overwhelming stress in their careers. The At Risk group had more physical, psychological, and anxiety related measures as well as more stress-related mistakes in their lives with the most unresolved issues than the Not at Risk group. Clearly identifying At Risk employees and making efforts to intervene with them is a good starting place.
With these measurable levels of stress so high for At Risk personnel, how does it impact their families and what, if anything helps to manage or reduce their stressors? Stress is often relieved through relationships and networks of support that buffer the harmful influences of the stress. Table 3 shows the comparison of the levels of support between the Not at Risk and At Risk respondents. In terms of their family relationships, the At Risk group scored better on only one measure, “I would consider myself to be a good parent” but the result was not significantly different. In other family measures, the At Risk group reported less support from family. They also reported significantly more stress in family context as well as being less likely to sit down to dinner together on a regular basis. The four questions about the relationship with the spouse are taken from Dr. John Gottman’s model The Four Horsemen of Divorce (1999). The At Risk group scored significantly higher on all four measures. The higher the scores on these four questions, the more likely divorce will occur.
In terms of coworker relationships, the At Risk group reported a significantly lower family life relationship with coworkers and significantly lower levels of feeling better by talking to coworkers about a difficult call. The At Risk had attended CISM debriefings slightly more, yet evaluated it slightly lower in terms of its being crucial to their success in the system. Among the At Risk who attended a CISM debriefing, 18 percent evaluated it as “didn’t help much” (compared to 11% of Not at Risk). Both groups reported similar levels of “it helped somewhat” and “it helped a great deal.” Under the three questions that addressed support from spiritual and religious sources, the At Risk group scored slightly higher than the Not at Risk group.
Well-being and positive job issues were also addressed in this study. An often studied measure of well-being is life satisfaction (Haslam & Mallon, 2003; Lourel et al., 2008; Mitchell, 1983; Setti & Argentero, 2014; Taylor, Wood, & Lichtman, 1983) and this study included seven measures of satisfaction. These include satisfaction with: life, family finances, spouse/partner, sleep, health, enjoying time off, and feeling that they would not change anything in their lives were they to live it over. Table 4 shows some of the consequences or outcomes of those Not at Risk compared to At Risk in satisfaction and positive job issues. The findings proved to be mixed when comparing the At Risk to Not at Risk groups. At Risk respondents had significantly lower measures of satisfaction with: life, finances, sleep. Both groups were very similar in satisfaction with spouse. The At Risk group also had significantly lower responses to “If I could live my life over I would change almost nothing.” The At Risk respondents did score significantly higher in enjoying time off from being on call as well as satisfaction with health.
| Measures | Not at Risk% | At Risk % | Ratio |
|---|---|---|---|
| Life satisfaction | |||
| Overall, I am satisfied with my life | 86.8 | 82.4 | 1:0.94 |
| Overall, I am satisfied with my family’s financial situation | 42.6 | 33.1*** | 1:0.80 |
| I enjoy my time off from being on call | 78.7 | 90.2* | 1:1.1 |
| Overall, I’m satisfied with my spouse/partner | 70.9 | 70.5 | 1:1 |
| Overall, I’m satisfied with the quality of my sleep | 32.4 | 24.6*** | 1:0.80 |
| Overall, I’m satisfied with my health | 38.1 | 49.3*** | 1:1.3 |
| If I could live my life over I would change almost nothing | 53.9 | 38.1*** | 1:0.71 |
| Positive job issues | |||
| I find my Emergency Service job to very rewarding to me | 84.3 | 74.6*** | 1:0.88 |
| My coworkers are like family to me | 73.9 | 59.1*** | 1:0.80 |
| I enjoy training experiences for my job | 83.1 | 69.1*** | 1:0.83 |
| I know that the victims I help are better off because of my efforts | 80.7 | 84.5 | 1:1 |
| The public views the work I do as valuable community service | 73.0 | 61.9*** | 1:0.85 |
| Working in EMS has given purpose to my life | 65.6 | 54.9** | 1:0.84 |
aT-Tests comparisons of means yielded significant differences as indicated by *= 0.05; **= 0.01; and ***= 0.001 levels.
Table 4: Percent Agreement among At Risk and Not At Risk Respondents on Measures of Consequences Measured by Life Satisfaction and Positive Job Issues for Not At Risk to At Risk Responses (Not At Risk N = 395, At Risk N = 142) with T-Tests Comparisons of Mean Scoresa
The positive job issues were also very revealing, assuming that higher levels of stress and unresolved past-call related issues impact the quality of work. The At Risk group scored significantly worse in all but one of the measures of their connectedness to their jobs. They were less likely to find the job rewarding; feel like coworkers are like family; enjoy training; feel that the public values their work; and that EMS has given purpose to their lives. They were slightly higher in feeling that the victims were better off because of their efforts.
These Utah EMS professionals have predictable levels of stress as measured by an Ongoing Stressors scale. “Ongoing Stressors” were comprised of 8 variables: “In the last 12 months, I have had thoughts of ending my life;” “My levels of stress often exceed my ability to handle them;” “I’ve increased my alcohol consumption in the last 6 months;” “I feel overburdened by debt;” “I often worry about being made physically ill because of exposure to diseases at work;” “My EMS stressors have harmed my relationships;” “I tend to be sick more than most people I know;” and “I suffer from depression.” Predicting their stressors was facilitated by using a Multiple Regression Path Analysis model. Multiple Regression is a strong analytical model when predicting behavioral outcomes as it indicates the simultaneous influence of each independent variable on the dependent variable using multi-variate coefficients. It also allows for the identification of paths of influence between the independent variables and the dependent variable. The model required the statistical development of five scales that were derived from factor analysis results; these scales and their development are recorded below.
“Life Satisfaction” was comprised of 6 well-used life satisfaction variables: “Overall, I am satisfied with my life;” “Overall, I am satisfied with my family’s financial situation;” “Overall, I’m satisfied with my spouse;” “Overall, I’m satisfied with the quality of my sleep;” “Overall, I’m satisfied with my health;” and “If I could live my life over I would change almost nothing.” “Support” was comprised of 5 variables: “My immediate family is a positive source of support for me in handling my EMS stressors;” “My personal spiritual beliefs are a source of strength to me;” “The CISM team is crucial to my success in the system;” “My personal spiritual practices are a source of strength in my life;” and “I consider myself to be very active in my religion.”
“Past Call Stress” was comprised of 5 variables: “I still suffer physical symptoms that came from exposure to a dangerous call;” “I still suffer psychological symptoms that came from a difficult call;” “At this time, I am burdened by unresolved anxieties about a past difficult call;” “I have felt call-related PTSD symptoms;” and “I still blame myself for the negative outcome of a call.” “Negative Marriage” was comprised of the 4 marriage assessment variables developed by Dr. John Gottman in his Four Horsemen of Divorce (1999): “My spouse and I tend to be very critical of one another;” “My spouse and I see way too much defect in one another;” “My spouse and I are overly defensive in our relationship together;” and “My spouse and I withdraw from each other at times.” Finally, Income Inadequacy was taken from the single question “Based on my current needs my income is: inadequate, adequate, or more than adequate”.
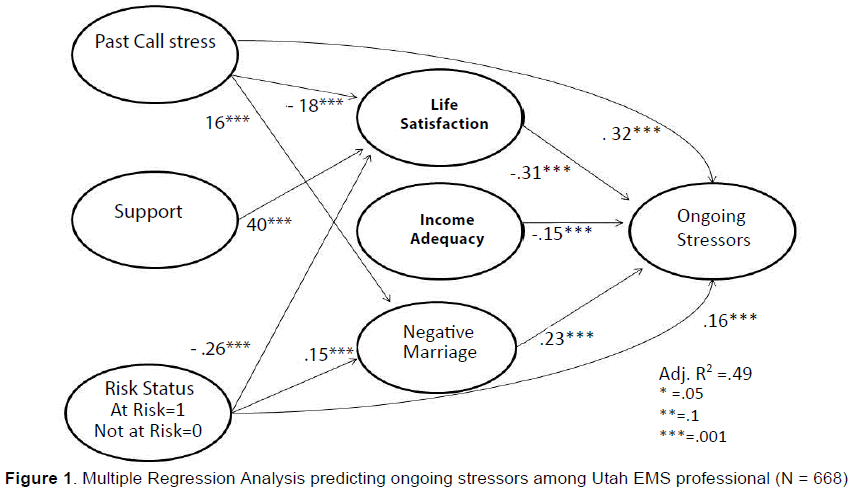
Risk status was coded At Risk = 1 and Not At Risk = 0. Figure 1 shows the results of the regression model. This model had an adjusted R squared of 0.49, meaning that it successfully predicted nearly half of the variance found in the Ongoing Stressor variable. The single strongest predictor of Ongoing Stressors was the Past Call Stress scale (0.32***). The higher their Past Call Stress score the significantly higher their Ongoing Stressors. Life Satisfaction was found to be inversely related to Ongoing Stressors, meaning the higher their life satisfaction, the lower their Ongoing Stressors (-0.31***). Higher income adequacy led to a lower Ongoing Stressor Score (-0.15***). The higher the negative Marriage score the significantly higher the Ongoing Stressors score (0.23***). Risk Status was coded as a 1 or 0. When higher it was found to predict significantly higher Ongoing Stressors (0.16***). Support was not found to be a significant direct predictor of Ongoing Stressors.
There were also indirect predictive paths found in the variables on the far left of the model. For example, Past Call Stress lead to lower Life Satisfaction (-0.18***) and Higher Negative Marriage (0.16***). The higher their Support the significantly higher their Life Satisfaction score (0.40***). Finally, the higher their At Risk status the significantly higher their negative Marriage score (0.15***).
Discussion
The At Risk respondents had more experience in their role while also feeling more discontent with their incomes and having a higher percentage of divorces. The At Risk respondents also scored worse on all 17 measures of stress. The ratios presented showed disproportionate levels of disparity between At Risk and Not at Risk groups in many of the measures. These findings present a troublesome set of data, especially for the At Risk category of respondents. First, be aware that highly stressed EMS employees are truly at risk. Burnout (Lourel, Abdellaoui, Chevaleyre et al., 2008); PTSD (Chopko & Schwartz, 2009); loss of social support as a result of mismanaged stresses (Haslam & Mallon, 2003); personal, social, and familial imbalances that impact work (Harris, Baloglu, & Stacks, 2003); the stress-related development of maladaptive coping styles (Bamber & McMahon, 2008); and the development of vulnerabilities that make subsequent traumas more harmful than past ones (Bryant & Guthrie, 2007). These issues are not in any way comprehensive nor exhausting in terms of consequences of stress and trauma in the lives of EMS professionals. From the traditional pathological point of view, this study’s results and other findings published in the field could render the discussion of post-trauma growth a lost cause.
However, from the posttraumatic growth paradigm, the issue must be dealt with and will best be deal with using scientificallybased wisdom and lessons learned in the arena of daily practice. The findings in this and other studies mandate some form of intervention strategy. The most commonly implemented of these is the Critical Incident Stress Debriefing and Management (CISD/CISM) efforts used by departments throughout the US and the world. At best, the original debriefing works by Jeffery Mitchell (1983; 1990; & 1997) has come under tremendous scrutiny among EMS professionals and within the scientific literature. Many publications of original and meta-analysis studies have shown either no benefit from CISDs or some harm (Bledsoe, 2003; Greenburg, 2001; Harris, 2003; Robinson, 2008). In this study, most respondents had attended a CISM debriefing, yet most did not find it crucial to their success in the EMS system. “Didn’t help much” was chosen by 11 percent of Not at Risk and 18 percent of At Risk respondents. Around 43-45 percent of respondents gave CISM any type of “helped” score.
Mitchell’s model was the answer when originally published because it was low cost, lay-people-sustained with only professional direction and support as needed, and mostly because it formally acknowledged the need to ameliorate the impact of traumas in the lives of EMS personnel. Throughout the world today, CISDs are being received in various settings for these very same reasons and applauded because something formal is being done to help people deal with work-related traumatic events (Regel, 2007). However, many in the field are ready to throw Mitchell and his CISM/CISD model out with proverbial dirty bathwater.
Regardless of the debriefing’s effectiveness—or lack thereof— it is unwise to undo stress management and debriefing efforts without having a sound strategy to replace it. Besides, “debriefed parties generally seem to appreciate the gesture…and report high levels of satisfaction” (Devilly, 2006, p. 332). This is especially true if the CISD was not mandated by supervisors or policies but was undertaken voluntarily. However, at its core, Mitchell’s CISDs are reparative in nature, contexted within a short session, and based to some degree on the pathological paradigm in their goal of repairing the damage from a significant trauma. The one-hit-wonder is perhaps necessary, but it is rarely sufficient alone.
Using the posttraumatic growth paradigm, the CISD would not simply be reparative. It would be prophylactic as part of a broader and more comprehensive growth-based model. Continuing to use Mitchell’s CISDs would allow EMS professionals to become more aware of the propensity for the types of stress that could overwhelm them by working in the field and not taking a proactive strategy to anticipate and manage traumatic events throughout their careers. The Correctional Service Canada has such a broad approach and defines their version of CISM in a Policy Bulletin from 2008 (Méthé):
Critical Incident Stress Management (CISM) is a program designed primarily for employees of the Service as they are likely to be involved in critical incidents because of the nature of their work. The first element is preventative, aimed at educating and preparing employees to deal with potential hazards of being exposed to very stressful events, and second, it focuses on providing support, assistance and follow-up services to individuals who have been involved in critical incidents. Some support, assistance and follow-up services may also be available for people who could be affected by the events, including employees, their families, visitors, etc., based on an evaluation of the situation, observed needs and/or requests brought forward.
The Canadian Correctional Services Policy is a comprehensive, system-wide intervention plan that includes these main comprehensive elements: ongoing preventative training; on-scene support; defusing session; individual interventions; demobilization sessions which would be a day long and away from the site— interventions intended for this major incidents that could span extended periods of time; Critical Incident Stress Debriefing (CISD); and thematic help sessions to provide ongoing information and education. Though no EMS system has perfected such a program, it may well be in the best interest of state and regional administrators to consider a comprehensive plan such as this in order to decrease the number of At Risk EMS personnel.
1See Harris (2003) for a 5-state study of EMS and CISM
References
- Bamber, M.A., & McMahon, R. (2008). Danger—early maladaptive schemas at work!: The role of early maladaptive schemas in career choice and the development of occupational stress in health workers. Clinical Psychology and Psychotherapy, 15(2), 96-112
- Bledsoe, B.E. (2003). Critical incident stress management (CISM): Benefit or risk for emergency services? Prehospital Emergency Care, 7(2), 272-279
- Bryant, R.A., & Guthrie, R.M. (2007). Maladaptive self-appraisals before trauma exposure predict posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 75(5), 812-815
- Chopko, B.A., & Schwartz, R.C. (2009). The relation between mindfulness and posttraumatic growth: A study of first responders to trauma-inducing incidents. Journal of Mental Health Counseling, 31(4), 363-376
- Devilly, G.J., Gist, R., & Cotton, P. (2006). Ready! Fire! Aim! The status of psychological debriefing and therapeutic interventions: In the work place and after disasters. Review of General Psychology, 10(4), 318-345.
- Gottman, J.S. (1999). The seven principles of making marriage work. New York, NY: Three Rivers Press
- Greenburg, N. (2001). A critical review of psychological debriefing: The management of psychological health after traumatic experiences. Journal of the Royal Naval Medical Service, 87(3), 158-161.
- Harris, M.A., Baloglu, M., & Stacks, J.R. (2002).Mental health of trauma-exposed firefighters and critical incident stress debriefing.Journal of Loss and Trauma, 7(3), 223-238
- Haslam, C., & Mallon, K. (2003).A preliminary investigation of post-traumatic stress symptoms among firefighters.Work & Stress, 17(3), 277-285
- Lourel, M., Abdellaoui, S., Chevaleyre, S., Paltrier, M., &Gana, K. (2008).Relationships between psychological job demands, job control and burnout among firefighters.North American Journal of Psychology, 10(3), 489-496
- Méthé, D. (2008, May 08). Commissioner’s directive: Critical incident stress management policy bulletin. Retrieved from http://www.csc-scc.gc.ca/text/plcy/cdshtm/253-2-gl-eng.shtml
- Mitchell, J.T. (1983). When disaster strikes…the critical incident stress debriefing process.Journal of Emergency Services, 8(1), 36-39.
- Mitchell, J.T., & Bray, G.P. (1990).Emergency service stress: Guidelines for preserving the health and careers of emergency services personnel. Englewood Cliffs, N.J.: Prentice-Hall.
- Mitchell, J.T., & Everly, G.S. (1997).The scientific evidence for critical incident stress management.Journal of Emergency Medical Services, 22(1), 86-93
- Paton, D. (2006). Posttraumatic growth in disaster and emergency work. In L.G. Calhoun & R.G. Tedeschi (Eds.), The handbook of posttraumatic growth: Research and practice (pp. 225-247). New York, NY: Psychology Press.
- Regel, S. (2007). Post-trauma support in the workplace: The current status and practice of critical incident stress management (CISM) and psychological debriefing (PD) within organization in the UK. Occupational Medicine, 57, 411-416
- Robinson, R. (2008). Reflections on the debriefing debate.Journal of Emergency Mental Health, 10(4), 253-259.
- Setti, I., &Argentero, P. (2014).The role of mindfulness in protecting firefighters from psychosomatic malaise.Traumatology: An International Journal, 20(2), 134-141
- Taylor, S.E., Wood, J.V., &Lichtman, R.R. (1983). It could be worse: Selective evaluation as a response to victimization. Journal of Social Issues, 39(2), 19-40.
- Tedeschi, R.G., & Calhoun, L.G. (2004). Routes to posttraumatic growth through cognitive processing. In D. Paton, J.M. Violanti, & L.M. Smith (Eds.), Promoting capabilities to manage posttraumatic stress: Perspectives on resilience. Springfield, IL: Charles C. Thomas.
- Williams, D. (2008). JEMS salary & workplace survey.Journal of Emergency Medical Services, 33(10), 21-29.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13995
- [From(publication date):
June-2015 - Apr 24, 2025] - Breakdown by view type
- HTML page views : 9312
- PDF downloads : 4683