Atrial Fibrillation in Intermediate CHA2DS2-Vasc Risk Group as a Cause of Thromboembolic Complications: Case Report
Received: 22-Oct-2021 / Accepted Date: 04-Nov-2021 / Published Date: 12-Nov-2021
Abstract
Atrial Fibrillation (AF) is a common arrhythmia, especially for elderly people and it can lead to thromboembolic complications. A 42-year-old man was presented with the strong abdominal pain, radiating to the back and a fever. He had elevated troponin, NT-pro-BNP, D-dimer. Electrocardiography (ECG) showed Atrial Fibrillation (AF), and an echocardiography revealed a slight enlargement of both atria. A coronary angiography did not show significant lesions, requiring an invasive intervention. Trans-Esophageal Echocardiography (TEE) confirmed thrombus in the left auricle. An embolic material in the superior mesenteric artery and infarction of right kidney were found in Computed Tomography Angiography (CTA). Beside standard treatment of ischemic heart disease, the patient received a therapeutic dose of Low Molecular Weight Heparin (LMWH) in the acute period of disease and then the heparin was changed to Novel Oral AntiCoagulants (NOAC). Despite of a therapy two weeks later he developed the embolism of the lower limb and the infarction of the left kidney. Then the TEE did not confirm the thrombus, so electric cardioversion was performed.
According to CHA2DS2-VASc scale, the patient received 1 point, so the anticoagulation should be considered (but it was not obligatory), weighing the individual bleeding risk against the risk of stroke. It is valid to treat each patient individually and take into account thromboembolic diseases, not only in high-risk group.
Keywords: CHA2DS2-VASc scale; Computed Tomography Angiography (CTA); Atrial fibrillation; Novel Oral Anti-Coagulants (NOAC), Peripheral vascular disease.
Case Report
A 42-year-old man was presented to the Emergency Department with the strong abdominal pain, severe on the right side, radiating to the back and a fever. The physical examination revealed a painful, tense stomach, nausea. On arrival, blood pressure was 148/92 mmHg and heart rate was 140 beats/min. So far, he has only been treated for hypertension. Abnormal laboratory results included elevated white blood cells, including elevated neutrocytes, elevated liver enzymes, NT-pro-BNP, D-dimer and troponin, moreover a slight prolong in prothrombin time. Electrocardiography (ECG) showed Atrial Fibrillation (AF). In echocardiography confirmed a normal systolic left ventricle function and a slight enlargement of both atria [Ejection Fraction (EF) about 60%, Left Atrial Dimension (LAD) about 4,1 cm, Left Atrial Area (LAAr) about 26 cm2, and right atrial area about 25 cm2].
Due to the elevated troponin level, it was decided to direct the patient to the Cardiology Department and perform a coronary angiography, to exclude or confirm Acute Coronary Syndrome (ACS). The invasive examination showed one-vessel disease-Left Anterior Descending artery (LAD) borderline stenosis. Because of hemodynamic stability of the patient and no significant stenosis of LAD, the patient was qualified for an ischemia assessment in stress ECHO. The patient was prescribed Angiotensin-Converting-Enzyme Inhibitor (ACEI), beta blocker, statin, and Dual Antiplatelet Therapy (DAPT) with a proton-pump inhibitor. Due to atrial fibrillation of unknown duration, Trans-Esophageal Echocardiography (TEE) was performed. It showed hyperechoic mass in the auricle of left atrium, corresponding to a thrombus, so the electric cardioversion was delayed (Figure 1).
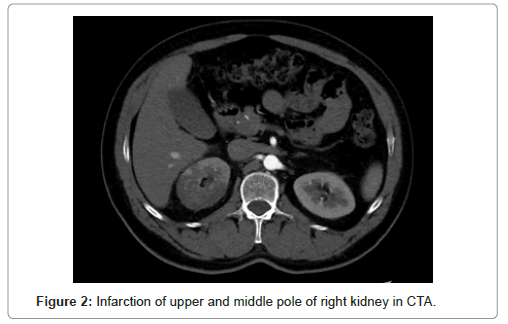
Clinical presentations of possible thromboembolic complications suggested Computed Tomography Angiography (CTA) performance. CTA revealed a small amount of embolic material in the superior mesenteric artery and no contrast in the upper pole of the right and middle part of the kidney diagnosed with a right kidney infarction. The patient was treated with therapeutic dose of Low Molecular Weight Heparin (LMWH) in the acute period of disease. In the last day of hospitalization, heparin was changed to dabigatran (150 mg twice daily).
Two weeks later the patient was directed to the Vascular Surgery Department, because of acute ischemia of left lower limb. Doctors performed embolectomy of left femoral artery. CTA confirmed infarction of the right kidney and additionally infarction of the upper pole of left kidney. There were no signs of mesenteric artery embolism and mesenteric vein thrombosis. TEE was repeated-without thrombus in the auricle of left atrium and chambers of the heart. The patient underwent a successful an electric cardioversion. Dabigatran treatment was still continued (Figure 2).
Later the patient was controlled twice in the Cardiology Clinic and AF was not diagnosed. The previous treatment was maintained i.e., Novel Oral Anti-Coagulants (NOAC), ACEI, beta blocker, statin and one antiplatelet drug with proton-pump inhibitor. The patient is still under the care of the Cardiology Department.
Discussion
Atrial Fibrillation (AF) is a common arrhythmia. Currently, there are about 335 million people in the world with AF [1]. The incidences of AF increase with age: 0,1% of cases in people under 55 years old, more than 5% in people over 65, and more than 9% in people over 80 [2]. The case of our patient is not very common, due to relatively young age of atrial fibrillation revealing.
The risk of ischemic stroke of brain in patients with AF is 4 times higher than in patients with sinus rhythm [3]. CHA2DS2-VASc score predicts thromboembolic events in patients with AF and helps to decide about anticoagulation therapy with Vitamin K Antagonist (VKA) or NOAC. The score includes the parameters such as heart failure, age, hypertension, diabetes, stroke, peripheral vascular disease and gender [4]. According to the CHA2DS2-VASc score, in the absence of risk factors (CHA2DS2-VASc score of 0 in males or 1 in females), anticoagulation therapy should not be started. With a score of 1 in males or 2 in females, anticoagulation should be considered, weighing the individual bleeding risk against the risk of stroke. In males with a CHA2DS2-VASc score of 2 or females with a score of 3, should be applied [5]. Patients with AF and intermediate risk (1 point form men or 2 for woman) are current problem, because it is still not clear, whether anticoagulants should be used [6].
Based on the CHA2DS2-VASc score, our patient received 1 point (for hypertension), so anticoagulation therapy should have been considered, but it was not obligatory. After the acute period of the disease, our patient was cured with high dose of dabigatran (150 mg twice a day) as a prevention of ischemic stroke. In the case of this patient, the decision about anticoagulation therapy was accurate, because a tendency to form thrombus and embolism was really high.
The one of the observational study, between 2013 and 2018, out of 1163 enrolled AF patients treated with NOAC, the Left Atrial Appendage Thrombus (LAAT) had been detected in 50 individuals (4,3%). Among these patients, 9 people (18,0%) were classified as an intermediate-risk of thromboembolic complications (the same as our patient) according to CHA2DS2-VASc scale [7]. LAAT was detected in all analyzed groups (except females without additional risk factors) of AF patients treated with NOAC independently of risk categories calculated by the CHA2DS2-VASc scale. It indicates that there are also other factors (not included in CHA2DS2-VASc scale), which determine thromboembolic diseases, so it should be remembered, especially in intermediate-risk group (Table 1).
| Parameter [unit] | Value | Normal range |
|---|---|---|
| WBC [/µL] | 20100 | 4000-10000 |
| ALT [U/L] | 79,6 | 0-41 |
| ASPT [U/L] | 84,3 | 0-40 |
| NT PRO-BNP [pg/ml] | 3155 | 0-115 |
| D-DIMER [ngFEU/ml] | 1258 | 0-500 |
| TROPONIN [pg/ml] | 39,3 | 0-14 |
| PT [s] | 13,2 | 9,4-12,5 |
Table 1: Patient’s incorrect parameters at the time of admission.
Conclusion
In pursuance of CHA2DS2-VASc scale, our patient was qualified as intermediate risk of thromboembolic complications. Despite this, the patient had a thrombus in the auricle of left atrium and systemic embolism. In conclusion, it is really important to treat each patient individually and take into account thromboembolic diseases, not only in high-risk group. It should be considered to extending the guidelines for NOAC therapy in patients with intermediate risk of thromboembolic complications.
References
- Wu J, Zhang Y, Liao X, Lei Y (2020) Anticoagulation therapy for non-valvular atrial fibrillation: A mini-review. Front Med (Lausanne) 7: 350.
- Alan Go S, Hylek EM, Phillips KA, Chang YC, Henault LE, et al. (2001) Prevalence of diagnosed atrial fibrillation in adults national implications for rhythm management and stroke prevention: The AnTicoagulation and risk factors in Atrial Fibrillation (ATRIA) study. Clin Cardiol 285(18): 2370-2375.
- Kim W, Kim E (2018) Heart failure as a risk factor for stroke. J Stroke 20(1): 33-45.
- Oksul M, Sener Y, Coteli C (2019) CHADS-VASc Score in STEMI patients: Should we use it really.? Acta Cardiologica Sinica 35(1): 89.
- Huisman M (2015) Patients with atrial fibrillation and a CHA2DS2-VASc score of 1: Are they at low or high stroke risk.? J Am Coll Cardiol 65(14): 1395-1397.
- Michalska A, Gorczyca I, Chrapek M, Kap?o?-Cie?licka A, Uzi?b?o-?yczkowska B, et al. (2020) Does the CHA2DS2-VASc scale sufficiently predict the risk of left atrial appendage thrombus in patients with diagnosed atrial fibrillation treated with non-vitamin K oral anticoagulants.? Medicine (Baltimore) 99(25):e20570.
Citation: Sobieszek G, Wójtowicz-Ściślak A (2021) Atrial Fibrillation in Intermediate CHA2DS2-Vasc Risk Group as a Cause of Thromboembolic Complications: Case Report. Atheroscler Open Access. 6:163.
Copyright: © 2021 Sobieszek G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 1496
- [From(publication date): 0-2021 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 964
- PDF downloads: 532