Case Report Open Access
Asymptomatic Colonic Tuberculosis in an Immunocompetent Patient
Nimah N. Jamaluddin1*, Guy A. Weiss2 and Wendy Ho2
1Department of Internal Medicine, UCLA Medical Center, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
2Division of Digestive Diseases, UCLA Medical Center, David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
- Corresponding Author:
- Nimah N. Jamaluddin
Department of Internal Medicine, UCLA Medical Center
David Geffen School of Medicine at UCLA, Los Angeles, CA
University of Los Angeles California 757 Westwood Plaza, Los Angeles CA, 90095, USA
Tel: 314-570-6412
E-mail: njamaluddin@mednet.ucla.edu
Received Date: October 10, 2015 Accepted Date: October 20, 2015 Published Date: October 28, 2015
Citation: Jamaluddin NN, Weiss GA, Ho W (2015) Asymptomatic Colonic Tuberculosis in an Immunocompetent Patient. J Gastrointest Dig Syst S13:010. doi:10.4172/2161-069X.1000S13-010
Copyright: © 2015 Jamaluddin, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
We present a case of a woman found to have features concerning for tuberculosis on a screening colonoscopy. Colonic tuberculosis presents with diverse clinical manifestations and resembles other clinical disorders, making its diagnosis challenging. It is imperative to know the classic risk factors and features that define this disease, as empiric treatment is often needed.
Keywords
Tuberculosis; Colonic tuberculosis
Introduction
Although tuberculosis (TB) is still rare in the United States, given recent globalization with increased cross-continental transition of people, gastrointestinal tuberculosis (TB) is an important disease for healthcare providers to be aware of [1]. Colonic TB presents with diverse clinical manifestations and mimics other clinical disorders, particularly Crohn’s colitis and malignancy, making its diagnosis challenging. Our current laboratory studies and imaging techniques have limited accuracy. Therefore, investigation of risk factors for TB, as well as for endoscopic and histological features, is essential. Misdiagnosis of this disease could have unfortunate consequences, given that Crohn’s disease, for instance, is often managed with immunosuppressive therapy. We present a unique case of an immunocompetent patient that required the collaborative work of gastroenterology, infectious disease, and pathology experts to successfully diagnose and treat our patient.
Case Report
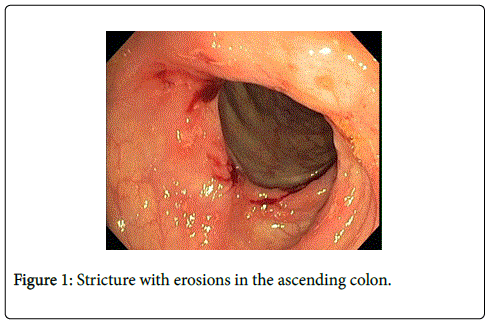
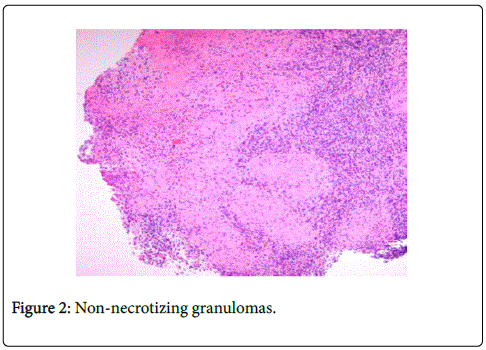
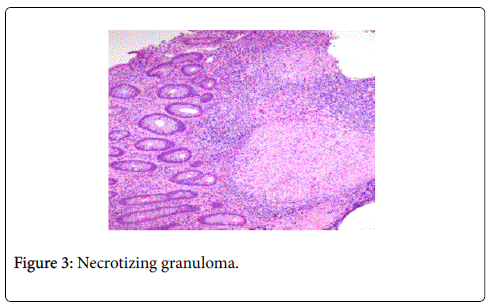
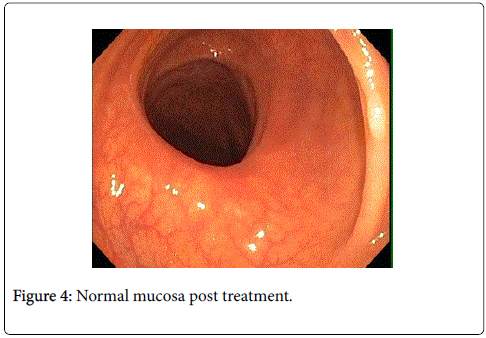
We present a female nurse with history of hypothyroidism who underwent her first average risk screening colonoscopy at the age of fifty-one. She was born in the Philippines and moved to the USA at age thirty-one. She denied nausea, abdominal pain, diarrhea, constipation, rectal bleeding, fever, chills, and weight loss. During colonoscopy, a colonic circumferential stricture with erosions was noted in the ascending colon (Figure 1). Multiple biopsies were obtained and pathology showed moderate to severe active colitis with multiple confluent necrotizing and non-necrotizing granulomas without features of chronic mucosal injury (Figures 2 and 3). Samples were negative for Mycobacterium tuberculosis complex polymerase chain reaction (MTB-PCR) and the smear was negative for acid-fast bacilli (AFB). The patient did, however test positive for MTB-Quantiferon-Gold. Chest x-ray showed no abnormalities. In light of her professional background as a nurse and her emigration from the Philippines, the suspicion of colonic tuberculosis was high and consequently, she was started on standard four drug therapy with isoniazid, rifampin, ethambutol, and pyrazinamide. After one month, this was simplified to isoniazid and rifampin, which she took for three months only, due to peripheral neuropathy despite daily pyridoxine 100mg daily. Repeat colonoscopy one month later revealed complete resolution of the colonic stricture with biopsies showing no residual granulomas (Figure 4).
Discussion
Colonic TB is emerging in the United States due to increasing Western immigration [1]. Patients can present with nonspecific symptoms such as fevers, weight loss, anorexia, and abdominal pain or, as in our case, patients may remain asymptomatic [2]. Regardless of the presenting symptoms, it is imperative that providers are able to recognize the pertinent endoscopic features as well as important risk factors to make the correct diagnosis. Intestinal TB can easily be misdiagnosed as inflammatory bowel disease, ischemic colitis, infectious colitis or colon cancer [3].
Evidence supporting intestinal TB in our patient included clinical aspects of her case, including her immigration status. Although there has been a decrease in the total number of reported cases of tuberculosis in United States, cases of TB in foreign-born individuals continues to rise [4]. A pertinent laboratory value in our patient’s case was having a positive Quantiferon Gold (QFT-G). The sensitivity of QFT-G for detecting MTB infections is approximately 80% in published studies, although the specific use of this test in intestinal tuberculosis has not been well studied [5,6]. Our patient also had an occupational risk factor working as a health care provider, making her at an increased risk of becoming infected with TB.
Most clinicians feel that colonoscopy with biopsies is the most important element of the evaluation [7]. The majority of studies have shown that the presence of granulomas, especially necrotizing granulomas as seen in our patient, is commonly seen in tuberculosis. Granulomas, also occur in Crohn’s disease, but are usually infrequent, non-necrotizing, and small [8]. Although our patient’s biopsies were negative for acid-fast bacilli staining and MTB complex PCR, they are important components of the evaluation. Acid fast bacilli staining of biopsy specimens has been shown to be positive in 30-60% of intestinal TB cases [9]. Given the length of time needed for culture, polymerase chain reaction (PCR) has become the more common diagnostic test with sensitivity and specificity reported around 75% and 85-95% respectively [3,10].
In conclusion, a high degree of suspicion is required for a timely diagnosis of intestinal TB. Studies show these patients have a high variability of symptoms, making evaluation of endoscopic features and risk factors important components of the investigation. Intestinal tuberculosis should be considered in the differential diagnosis, especially when physicians are considering giving immunosuppressant medications. We present this case to show that if the suspicion for intestinal TB is high enough, a therapeutic trial with antitubercular drugs should be considered.
References
- (2013) CDC, Reported Tuberculosis in the United States. Atlanta, GA: U.S. Department of Health and Human Services.
- Sato S, Yao K, Yao T, Schlemper RJ, Matsui T, et al. (2004) Colonoscopy in the diagnosis of intestinal tuberculosis in asymptomatic patients. below GastrointestEndosc 59: 362-368.
- Almadi MA, Ghosh S, Aljebreen AM (2009) Differentiating intestinal tuberculosis from Crohn's disease: a diagnostic challenge. below Am J Gastroenterol 104: 1003-1012.
- Jehangir W, Khan R, Gil C, Baruiz-Creel M, Bandel G, et al. (2015) Abdominal Tuberculosis: An Immigrant's Disease in the United States. below N Am J Med Sci 7: 247-252.
- Pulimood AB, Amarapurkar DN, Ghoshal U, Phillip M, Pai CG, et al. (2011) Differentiation of Crohn's disease from intestinal tuberculosis in India in 2010. below World J Gastroenterol 17: 433-443.
- Li X, Liu X, Zou Y, Ouyang C, Wu X, et al. (2011) Predictors of clinical and endoscopic findings in differentiating Crohn's disease from intestinal tuberculosis. below Dig Dis Sci 56: 188-196.
- Khan R, Abid S, Jafri W, Abbas Z, Hameed K, et al. (2006) Diagnostic dilemma of abdominal tuberculosis in non-HIV patients: an ongoing challenge for physicians. below World J Gastroenterol 12: 6371-6375.
- Pulimood AB, Ramakrishna BS, Kurian G, Peter S, Patra S, et al. (1999) Endoscopic mucosal biopsies are useful in distinguishing granulomatous colitis due to Crohn's disease from tuberculosis. below Gut 45: 537-541.
- Horvath KD, Whelan RL (1998) Intestinal tuberculosis: return of an old disease. below Am J Gastroenterol 93: 692-696.
- Gan HT (2002) Differentiation between intestinal tuberculosis and Crohn's disease in endoscopic biopsy specimens by polymerase chain reaction. Am J Gastroenterol 97: 1446-1451.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13635
- [From(publication date):
specialissue-2015 - Dec 27, 2024] - Breakdown by view type
- HTML page views : 9210
- PDF downloads : 4425