Associations between Healthcare Trust, Health Information Trust, and Barriers to Colorectal and Cervical Cancer Screening
Received: 03-Jan-2022 / Manuscript No. jcmhe-21-50022 / Editor assigned: 05-Jan-2022 / PreQC No. jcmhe-21-50022 (PQ) / Reviewed: 19-Jan-2022 / QC No. jcmhe-21-50022 / Revised: 24-Jan-2022 / Manuscript No. jcmhe-21-50022 (R) / Published Date: 31-Jan-2022 DOI: 10.4172/2168-9717.1000734
Abstract
Objective: Trust in the healthcare system and health information is an important determining factor for patient healthcare utilization. This study examines the relationships among healthcare trust, health information trust, and barriers to screening, and their association with receipt of cervical and colorectal cancer screening.
Methods: Women aged 45 years-65 years in central Pennsylvania completed a survey about cancer screening (n=474). We used chi square tests, bivariate and multivariable logistic regression, and moderation analysis to examine associations among healthcare trust, health information trust, barriers to screening, and being up to date with cervical cancer screening and with colorectal cancer screening.
Results: On average, participants were 55.1 years old. Being up to date with cervical and colorectal cancer screening was more common in participants with private insurance and those who had a check-up within the last year (all p<0.05). Cervical cancer screening was higher for participants with greater health information trust and fewer barriers (both p<0.05). Colorectal cancer screening was higher for participants with fewer barriers to screening (multivariable odds ratio [OR]=0.54, 95% confidence interval [CI]=0.35-0.82). There was no evidence of an interaction between barriers to screening and healthcare trust or health information trust with cervical cancer screening (p=0.70 and p=0.07, respectively) or colorectal cancer screening (p=0.59 andp=0.93, respectively).
Conclusion: Measures of trust did not moderate the relationship between barriers to screening and screening uptake, suggesting that interventions may directly impact screening behaviors by targeting either trust or barriers. The findings of this study can guide future interventions to promote cervical and colorectal cancer screening uptake.
Keywords
Cancer screening; Healthcare trust; Health information trust; Cervical cancer; Colorectal cancer; Barriers to screening
Introduction
Cancer is the second leading cause of death in the United States [1]. Cancer screening can reduce mortality from certain cancers, but uptake is suboptimal. The American Cancer Society (ACS) recommends that adults aged 45 to 75 undergo regular screening with a high sensitivity stool based test or a visualization exam for colorectal cancer [2]. The uptake of colorectal cancer screening is 65.2%, which is below the Healthy People 2030 goal of 74.4% [3]. Similarly, ACS recommends that women aged 25 to 65 get screened for cervical cancer every 5 years with primary Human Papillomavirus (HPV) testing; if primary HPV testing is unavailable, a co-test (HPV test with a Pap test) every 5 years or a Pap test every 3 years is recommended [2]. The uptake of cervical cancer screening in women aged 21-65 is 80.5%, which is below the Healthy People 2030 goal of 84.3% [4]. The reasons for suboptimal cancer screening are multiple and complex, including patients’ trust and other barriers to care.
Trust in the healthcare system plays a defining role in healthcare use [5]. Lack of trust in the healthcare system is associated with lower participation in health promoting behaviors, including cancer screening [6-8]. Healthcare trust is multifaceted. It can be evaluated at the micro level (i.e., between a patient and individual healthcare providers, health insurers, and pharmacists) and at the macro level (i.e., between the public and overall healthcare system) [9]. Trust in the U.S. healthcare system varies in different patient populations, with higher trust observed among higher versus low income adults, older versus younger adults, and men versus women [10]. An emerging, but separate, dimension of trust is trust in sources of health information. Trust in health information sources also varies among different patient populations, with increased trust of more diverse sources (i.e. radio, magazine, charitable organizations, and religious organizations) seen in Black and Latino individuals compared to White [11], as well as age differences specifically in trust in health information from the Internet [12]. Differing levels of trust in health information sources may influence health information seeking behaviors, and in turn impact cancer screening.
Beyond the association with healthcare trust, the suboptimal prevalence of cervical and colorectal cancer screening is associated with other barriers to screening. Underserved patients face barriers to cancer screening such as cost, fear of finding cancer, fear of the procedure itself, and logistical challenges [13,14]. The roles of healthcare and health information trust, other barriers to screening, and their interrelated associations with cancer screening are yet to be fully understood. Trust and barriers to screening may operate as independent or interacting correlates of cancer screening, and understanding the nature of these relationships can inform future interventions to promote cancer screening.
Materials and Methods
Data source
English speaking women aged 45 years-65 years (inclusive) from 28 counties in central Pennsylvania were recruited to participate in a survey on cancer screening. Participants were primarily recruited through paid social media advertisements, targeted by zip code. Surveys were administered by a study team member over the phone or self-administered online. Participants provided verbal or implied consent before completing the survey.
Out of 994 people who responded to the study invitation, 773 (77.8%) were eligible for participation; age was the most common reason for ineligibility (n=184). A total of 474 women enrolled and finished the survey. (The remaining respondents were not able to complete the survey due to meeting recruitment goals.) Full details regarding the study population, recruitment methods, survey details, and additional participant information can be found elsewhere [15].
Measures
Self-reported demographic and medical information was collected from all participants, including education, insurance status, check-up in the last year, personal and family history of cancer, and if they had had a hysterectomy (Table 1).
Table 1: Descriptive statistics for survey participants
| n | % | |
|---|---|---|
| Total sample | 474 | -- |
| Educational attainment | ||
| High school degree or less | 63 | 13.8 |
| More than high school degree | 393 | 86.2 |
| Insurance status | ||
| Non-private | 130 | 27.4 |
| Private | 344 | 72.6 |
| Check-up in last year | ||
| No | 116 | 24.6 |
| Yes | 356 | 75.4 |
| Personal cancer history | ||
| No | 389 | 82.2 |
| Yes | 84 | 17.8 |
| Family cancer history | ||
| No | 148 | 31.5 |
| Yes | 322 | 68.5 |
| Had a hysterectomy | ||
| No | 345 | 72.8 |
| Yes | 129 | 27.2 |
Independent variables: Healthcare trust was assessed using three items [16]. Participant responses to the three items were scored and averaged such that higher scores indicated greater healthcare trust. The average scores (potential range: 1-4) were then classified as “high trust” if the average was ≥ 3 or “low trust” if the average was <3.
Health information trust was assessed using two items drawn from the National Cancer Institute Health Information National Trends Survey [17]. Participant responses to the two items were scored and averaged such that higher scores indicated greater health information trust. The average scores (potential range: 1-4) were then classified as “high trust” if the average was ≥ 3 or “low trust” if the average was <3.
Barriers to cancer screening were assessed separately for cervical cancer and for colorectal cancer. Participants reported how much they agreed or disagreed with the following potential barriers to each cancer screening: they
(1) Don’t know how to
(2) Don’t need to
(3) Think it is embarrassing to
(4) Are afraid to
(5) Think it is too great a cost to
(6) Think the doctor is too far away to get screened (Table 2).
Table 2: Health-related barriers to cervical and colorectal cancer screening.
| Disagree (1, 2) | Agree (3, 4) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Cervical cancer | ||||
| I don't know how to get checked for cervical cancer. | 426 | 95.7 | 19 | 4.3 |
| I don't need to get checked for cervical cancer. | 374 | 85.8 | 62 | 14.2 |
| It is embarrassing to get checked for cervical cancer. | 315 | 69.5 | 138 | 30.5 |
| I'm afraid of the results I would receive from a cervical cancer checkup. | 345 | 77.7 | 99 | 22.3 |
| The cost of getting checked for cervical cancer is too high. | 363 | 82.5 | 77 | 17.5 |
| The doctor is too far away for me to easily go get a cervical cancer checkup. | 434 | 96.9 | 14 | 3.1 |
| Colorectal cancer | ||||
| I don't know how to get checked for colorectal cancer. | 442 | 96.7 | 15 | 3.3 |
| I don't need to get checked for colorectal cancer. | 425 | 92.8 | 33 | 7.2 |
| It is embarrassing to get checked for colorectal cancer. | 267 | 58.6 | 189 | 41.5 |
| I'm afraid of the results I would receive from a colorectal cancer checkup. | 327 | 72.0 | 127 | 28.0 |
| The cost of getting checked for colorectal cancer is too high. | 331 | 72.8 | 124 | 27.3 |
| The doctor is too far away for me to easily go get a colorectal cancer checkup. | 433 | 95.6 | 20 | 4.4 |
| Few barriers (0-1 endorsed) | Many barriers (2+endorsed) | |||
| n | % | n | % | |
| Cervical cancer screening barrier score | 302 | 74.4 | 104 | 25.6 |
| Colorectal cancer screening barrier score | 285 | 65.1 | 153 | 34.9 |
Participant responses of agree or strongly agree were coded as “endorsed,” and responses of disagree or strongly disagree were coded as “not endorsed.” Total number of barriers for screening for each cancer was summed and coded as “few barriers” (0-1 barriers endorsed) or “many barriers” (2+barriers endorsed).
Dependent variables: Participants were classified as up to date on screening for cervical and colorectal cancer following the American Cancer Society recommendations [2]. Women were considered up to date for colorectal cancer screening if they reported having a visualization test (e.g., colonoscopy, sigmoidoscopy) within the past five years and/or a stool based test within the past year. Women were considered up to date with cervical cancer screening if they had a Pap test within the past three years and/or had a HPV test within the past five years.
Statistical analysis
We generated descriptive statistics for the sample, calculating means and frequencies of demographic and medical variables, scores on cancer screening barriers and trust variables, and prevalence of being up to date with screening.
To evaluate which participants were more or less likely to have high levels of trust, we assessed the bivariate relationships between (a) demographic and medical variables and (b) high versus low trust (separately for healthcare trust and health information trust) using chi square tests. We also used a chi square test to assess the concordance between healthcare trust and health information trust.
Next, we conducted bivariate logistic regression models to assess the associations between each independent variable (healthcare trust, health information trust, barriers to screening, and the demographic and medical variables) and being up to date with cervical cancer screening or with colorectal cancer screening (separately). (Models evaluating associations with cervical cancer screening used the barriers to cervical cancer screening score only, and models evaluating associations with colorectal cancer screening used the barriers to colorectal cancer screening score only.) Then, we conducted multivariable logistic regression to assess the associations between all of the independent variables and being up to date with screening. Finally, to assess potential moderated effects, we added to each multivariable logistic regression model two multiplicative interaction terms for (1) scores on healthcare trust and barriers to screening, and (2) scores on health information trust and barriers to screening. We used a Wald chi square test to evaluate the joint contribution of each interaction term to the model. We probed these interactions by evaluating the relationship between barriers to screening and being up to date, stratified across levels of trust.
Analyses were conducted using SAS version 9.4 (Cary, NC). The statistical tests used a two sided p<.05, except for the interaction analyses, which used a two sided p<.10. The Penn State College of Medicine Institutional Review Board/Human Subjects Protection Office approved all components of this study, including data collection and analysis.
Results
On average, participants were 55.1 years old (standard error [SE]=0.3) (Table 1). Most participants had more than a high school degree (86.2%), private insurance (72.6%), a check-up within the last year (75.4%), and no personal history of cancer (82.2%). A large percentage of participants had a family history of cancer (68.5%). Most participants reported few barriers (0-1 barriers endorsed) to cervical cancer screening (74.4%) and colorectal cancer screening (65.1%) (Table 2).
Measures of trust
index (Table 3). Participants with high trust in the health care system were more likely to have a personal (p<.01) or family (p<.01) history of cancer.
Table 3: Healthcare and health information trust
| Low trust (1, 2) | High trust (3, 4) | |||
|---|---|---|---|---|
| Healthcare Trust | n | % | n | % |
| Healthcare organizations are more concerned about making money than taking care of people. [reverse-coded] | 183 | 39.2 | 284 | 60.8 |
| Patients should always follow the advice given to them at healthcare organizations. | 97 | 20.8 | 370 | 79.2 |
| If I had a medical problem, I would see a doctor. | 30 | 6.5 | 435 | 93.6 |
| Low trust (1, 2) | High trust (3, 4) | |||
| Health Information Trust | n | % | n | % |
| In general, how much would you trust information about cancer from a doctor or other healthcare professional? | 9 | 1.9 | 457 | 98.1 |
| In general, how much would you trust information about cancer on the internet? | 249 | 53.6 | 216 | 46.5 |
| Low (mean: 1 to <3) | High (mean: 3 to 4) | |||
| n | % | n | % | |
| Healthcare trust index score | 117 | 25.0 | 352 | 75.1 |
| Health information trust index score | 107 | 22.9 | 360 | 77.1 |
Overall, 77.1% of participants had high scores on the health information trust index (Table 3). Participants with high trust in health information were more likely to have an education beyond high school (p=.03) and were more likely to have received a check-up within the last year (p<.01).
Overall, 58.5% of participants had high trust in both health information and the health care system, and 6.2% of participants had low trust in both health information and the health care system. Trust in the health care system was not associated with trust in health information (p=.54), indicating that the two trust variables were independent from each other.
Cervical cancer screening
Most participants were up to date for cervical cancer screening (284/343 women without a hysterectomy, or 82.8%). In bivariate analysis, cervical cancer screening was more common among participants with high health information trust, few barriers to screening, private insurance, and a check-up within the last year (all p<.05); (Table 4).
Table 4: Bivariate and multivariable analyses of being up-to-date for cervical cancer screening, excluding hysterectomy
| Bivariate | Multivariable | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Healthcare trust index score | ||||
| Low | (ref) | (ref) | ||
| High | 1.69 | (0.93-3.10) | 1.21 | (0.56-2.64) |
| Health information trust index score | ||||
| Low | (ref) | (ref) | ||
| High | 2.14 | (1.17-3.93) | 1.55 | (0.72-3.31) |
| Barriers to screening | ||||
| Few barriers (0-1 endorsed) | (ref) | (ref) | ||
| Many barriers (2+ endorsed) | 0.45 | (0.24-0.83) | 0.82 | (0.38-1.77) |
| Educational attainment | ||||
| High school degree or less | (ref) | (ref) | ||
| More than high school degree | 1.41 | (0.66-3.04) | 1.01 | (0.41-2.52) |
| Insurance status | ||||
| Non-private | (ref) | (ref) | ||
| Private | 4.45 | (2.48-7.99) | 3.11 | (1.50-6.43) |
| Check-up in last year | ||||
| No | (ref) | (ref) | ||
| Yes | 6.36 | (3.49-11.57) | 6.20 | (3.09-12.43) |
| Personal cancer history | ||||
| No | (ref) | (ref) | ||
| Yes | 2.21 | (0.84-5.80) | 1.26 | (0.40-3.97) |
| Family cancer history | ||||
| No | (ref) | (ref) | ||
| Yes | 1.25 | (0.69-2.25) | 0.92 | (0.43-1.97) |
In multivariable analysis, none of the three independent variables (healthcare trust, health information trust, and barriers to screening) were associated with being up to date with cervical cancer screening (Table 4). Being up to date with cervical cancer screening was more common among participants with private insurance (odds ratio [OR]=3.11, 95% confidence interval [CI]=1.50-6.43) and those who had a check-up in the last year (OR=6.20, 95% CI=3.09-12.43).
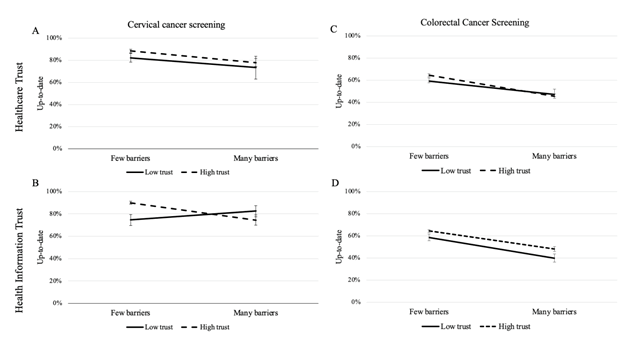
Interactions between barriers with healthcare trust or health information trust in their relationship with cervical cancer screening. In moderation analysis, there was no evidence of an interaction between barriers to screening and healthcare trust in their relationship with cervical cancer screening (interaction p=.70) (Figure 1A). However, barriers to screening and health information trust interacted in their relationship with cervical cancer screening (interaction p=.07) (Figure 1B). Specifically, among participants with low health information trust, endorsing many barriers to screening was non significantly associated with higher odds of screening (OR=2.71, 95% CI=0.57-12.76; p=.21), but among participants with high health information trust, endorsing more barriers to screening was non-significantly associated with lower odds of screening (OR=0.59, 95% CI=0.23-1.50; p=.27). Participants with few barriers and high health information trust were most likely to be up to date on cervical cancer screening (88.7%, SE=0.6%).
Colorectal cancer screening
About half of participants were up to date for colorectal cancer screening (262/473, or 55.4%). In bivariate analysis, colorectal cancer screening was more common among participants with few barriers to screening, private insurance, a check-up in the last year, and a family history of cancer (Table 5).
Table 5: Bivariate and multivariable analyses of being up-to-date for colorectal cancer screening.
| Bivariate | Multivariable | |||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Healthcare trust index score | ||||
| Low | (ref) | (ref) | ||
| High | 1.09 | (0.72-1.70) | 0.97 | (0.60-1.54) |
| Health information trust index score | ||||
| Low | (ref) | (ref) | ||
| High | 1.42 | (0.92-2.19) | 1.21 | (0.75-1.96) |
| Barriers to screening | ||||
| Few barriers (0-1 endorsed) | (ref) | (ref) | ||
| Many barriers (2+ endorsed) | 0.51 | (0.34-0.76) | 0.54 | (0.35-0.82) |
| Educational attainment | ||||
| High school degree or less | (ref) | (ref) | ||
| More than high school degree | 0.80 | (0.46-1.39) | 0.67 | (0.37-1.22) |
| Insurance status | ||||
| Non-private | (ref) | (ref) | ||
| Private | 1.67 | (1.11-2.51) | 1.63 | (1.04-2.57) |
| Check-up in last year | ||||
| No | (ref) | (ref) | ||
| Yes | 2.26 | (1.47-3.46) | 2.09 | (1.31-3.31) |
| Personal cancer history | ||||
| No | (ref) | (ref) | ||
| Yes | 1.23 | (0.76-1.99) | 1.16 | (0.67-2.00) |
| Family cancer history | ||||
| No | (ref) | (ref) | ||
| Yes | 1.75 | (1.18-2.59) | 1.78 | (1.16-2.75) |
In multivariable analysis, participants with more barriers were less likely to be up to date with colorectal cancer screening (OR=0.54, 95% CI=0.35-0.82), but healthcare trust and health information trust were not associated with screening (Table 5). Being up to date was more common among participants with private insurance (OR=1.63, 95% CI=1.04-2.57), those who had a check-up in the last year (OR=2.09, 95% CI=1.31-3.31), and those with a family history of cancer (OR=1.78, 95% CI=1.16-2.75).
Interactions between barriers with healthcare trust or health information trust in their relationship with colorectal cancer screening. There was no evidence that barriers to screening interacted with healthcare trust (p=0.59) or health information trust (p=0.93) in their relationship with colorectal cancer screening (Figures 1C and 1D).
Discussion
Overall, the findings from this study indicate that healthcare trust, health information trust, and barriers to screening are distinct concepts with generally independent associations with cancer screening behaviors. Most participants had high healthcare trust, high health information trust, and few barriers to screening. Importantly, the measures of trust were distinct and had dissimilar covariates: High levels of healthcare trust were associated with personal and family history of cancer, while high levels of health information trust were associated with post high school education and recent check-ups.
We hypothesized that patients with high levels of trust would access screening regardless of other barriers, but patients with low levels of trust would demonstrate a negative association between barriers and screening. However, we found limited support for this hypothesis. For cervical cancer, we found that, among participants with high trust in health information, screening was negatively associated with other barriers to screening, but among participants with low trust, screening was positively associated with other barriers (although both relationships were not statistically significant). For colorectal cancer, there was no evidence of an interaction between barriers and either measure of trust. Thus, psychosocial interventions aiming to increase cancer screening may be able to target any of these three constructs independently, or focus on other, more salient predictors of screening uptake.
The findings from the current study extend prior knowledge of factors associated with cervical cancer screening. The bivariate analysis demonstrated that being up to date with cervical cancer screening was more common for women with higher health information trust and fewer barriers to screening, as shown in previous literature [13]; however, these relationships no longer held true after adjusting for demographic variables. In fact, the final models demonstrated that, controlling for all other variables, being up to date with cervical cancer screening was more common for participants with private insurance and a recent check-up. Therefore, our results suggest a potential mediation effect such that the relationship between our primary predictor variables and screening was explained by having private insurance and a recent check-up; these latter variables were more strongly and proximally associated with being up to date with cervical cancer screening. (However, the cross-sectional design of our study precludes inferences about temporality and causality). Insurance coverage has been previously linked to cervical cancer screening disparities among women, as it mitigates cost [18]. In addition, primary care providers can provide cervical cancer screening at yearly check-ups, as well as educate and refer patients for screening. These opportunities for interactions between patients and representatives of the healthcare system may also support the development of healthcare/health information trust. We also found a relationship between barriers to screening, health information trust, and being up to date with cervical cancer screening (Figure 1B). Cervical cancer screening was highest among participants with few barriers and high health information trust. It is possible that this group of patients have opportunities (e.g., via annual check-ups) to interact with clinicians, who may provide both cancer screening and education about health information sources, thereby increasing a patient’s level of health information trust.
For colorectal cancer, bivariate analysis demonstrated that barriers to screening, private insurance, a check-up within the last year, and a family history were associated with being up to date on screening. The multivariable analysis suggested that there was no relationship between healthcare trust, healthcare information trust, and being up to date with colorectal screening; however, private insurance, a recent check-up, and family history maintained their relationships to screening. Similar to cervical cancer screening, prior research has demonstrated an association between colorectal cancer screening and insurance status [19], likely as a reflection of cost, and having a recent check-up, as it gives the opportunity for the provider to discuss screening options and benefits. Results were also consistent with a previous study that reported the importance of social influences (e.g., having multiple affected family members, receiving family encouragement, and being close to an affected family member) for colorectal cancer screening [20]. In the current study, family history of cancer was associated with higher healthcare trust, and individuals with a family history of cancer were more likely to get screened (Table 5). This suggests that interventions should therefore consider the significant influence of family history, and providers may counsel patients differently for individuals with or without this history. While moderation analysis indicated no interaction between barriers to cancer screening and trust in the healthcare system or health information (Figure 1D), individuals reporting more barriers to screening were significantly less likely to be up to date with colorectal cancer screening, suggesting that the impact of barriers on cancer screening is similar regardless of trust. As a result, it may be more efficient for colorectal cancer screening promotion programs to target barriers to screening rather than trust.
Cancer screening promotion programs should focus on reducing barriers at the structural, provider, and individual levels. These include structural level barriers of high cost, inability to take time off work, or lack of insurance, individual level barriers of embarrassment or fear of the results, and provider level barriers such as lack of trust or lack of recommendation [21,22]. While the use of at home self-sampling tests, including fecal occult blood tests and fecal immunochemical tests, may overcome some of these obstacles, barriers such as lack of motivation and forgetfulness to send back the testing kits still impede optimal screening uptake [23].
In terms of study strengths, we expanded upon previous literature on cancer screening through the simultaneous analysis of two forms of health related trust (healthcare and health information), and multiple screening barriers. In terms of study limitations, we assessed selfreported cancer screening behaviors, which are subject to recall bias [24]. Furthermore, the data may lack generalizability due to the demographics of participants, e.g., 97% of participants were non-Hispanic White, a group that is generally less at risk for cervical and/or colorectal cancer than Latina or Black women [25-27]. Our study used direct marketing to recruit participants, which is likely less effective at recruiting participants from underrepresented racial and ethnic groups than referrals from other participants [28].
Conclusion
This study provides insight into the relationship between healthcare and health information trust, barriers to cervical and colorectal cancer screening, and uptake of cancer screenings. While our moderation hypothesis was not supported by the data, we were able to identify personal characteristics that correlated with uptake of cervical and colorectal cancer screenings. Our findings suggest that future interventions aimed at increasing colorectal cancer screening should focus on reducing barriers instead of focusing on trust. Studies addressing cervical cancer screenings should aim to better understand how trust and barriers relate to screening uptake, as this relationship is more nuanced. Additional research is needed to better understand the role of healthcare and health information trust and barriers as they generally relate to cancer screening uptake.
Conflicts of Interest
The authors have no real or potential conflicts of interest to report.
Funding
This study was supported by an Institutional Research Grant, IRG-17- 175-04, from the American Cancer Society.
Data Availability
Data are available upon reasonable request to the senior author (JLM).
References
- Siegel RL, Miller KD, Jemal A (2020) Cancer statistics. CA Cancer J Clin 70: 7-30.
[Cross Ref] [Google Scholar] [PubMed]
- Cancer statistics.
- White A, Thompson TD, White MC, Sabatino SA, Janet DM, et al. (2017) Cancer Screening test use: United States, 2015. MMWR Morb Mortal Wkly Rep 66(8): 201-206.
[Cross Ref] [Google Scholar] [PubMed]
- State Cancer Profiles. (2020) Dynamic views of cancer statistics for prioritizing cancer control efforts across the nation, National Cancer Institute.
- Whetten K, Leserman J, Whetten R, Ostermann J, Thielman N, et al. (2006) Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health 96(4): 716-721.
[Cross Ref] [Google Scholar] [PubMed]
- Katapodi MC, Pierce PF, Facione NC (2010) Distrust, predisposition to use health services and breast cancer screening: Results from a multicultural community-based survey. Int J Nurs Stud 47(8): 975-983.
[Cross Ref] [Google Scholar] [PubMed]
- Tse-Chuan Y, Stephen AM, Hillemeier MM (2011) Effects of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am J Public Health, 101(7): 1297–1305.
[Cross Ref] [Google Scholar] [PubMed]
- Gupta S, Brenner AT, Ratanawongsa N, Inadomi JM (2014) Patient trust in physician influences colorectal cancer screening in low-income patients. Am J Prev Med 47(4): 417-423.
[Cross Ref] [Google Scholar] [PubMed]
- Rasiah S, Jaafar S, Yusof S, Ponnudurai F, Pooi K, et al. (2020) A study of the nature and level of trust between patients and healthcare providers, its dimensions, and determinants: a scoping review protocol. BMJ Open 10(1): 1-5.
- Blendon RJ, Benson JM, Hero JO (2014) Public trust in physicians: US medicine in international perspective. N Engl J Med, 371(17): 1570-1572.
[Cross Ref] [Google Scholar] [PubMed]
- Fareed N, Swoboda C, Jonnalagadda P, Walker D, Huerta T (2021) Differences between races in health information seeking and trust over time: Evidence from a cross-sectional, pooled analyses of hints data. Am J Health Promot 35(1): 84-92.
[Cross Ref] [Google Scholar] [PubMed]
- Miller L, Bell R (2012) Online health information seeking: The influence of age, information trustworthiness, and search challenges. J Aging Health 24(3): 525-541.
[Cross Ref] [Google Scholar] [PubMed]
- Akinlotan M, Bolin JN, Helduser J, Ojinnaka C, Lichorad A, et al. (2017) Cervical cancer screening barriers and risk factor knowledge among uninsured women. J Community Health 42(4): 770–778.
[Cross Ref] [Google Scholar] [PubMed]
- Muthukrishnan M, Arnold D, James AS (2019) Patients' self-reported barriers to colon cancer screening in federally qualified health center settings. Prev Med Rep 15:100896.
[Cross Ref] [Google Scholar] [PubMed]
- Popalis. Geographic disparities in cancer screening barriers and behaviors: The role of county-level metropolitan status and racial residential segregation.
- Turgeon M, Havard M, Pallera H, Diller P, Gefter L (2021) Levels of trust in the healthcare system among low-income youth: An evaluation of an assessment tool for a school-based health promotion program.
[Cross Ref] [Google Scholar] [PubMed]
- National Cancer Institute. Health Information National Trends Survey.
- Cowburn S, Carlson MJ, Lapidus JA, DeVoe JE (2013) The association between insurance status and cervical cancer screening in community health centers: Exploring the potential of electronic health records for population-level surveillance, 2008-2010. Prev Chronic Dis 10: E173.
[Cross Ref] [Google Scholar] [PubMed]
- De Moor JS, Cohen RA, Shapiro JA, Nadel MR, Sabatino SA, et al. (2018) Colorectal cancer screening in the United States: Trends from 2008 to 2015 and variation by health insurance coverage. Prev Med 112: 199-206.
[Cross Ref] [Google Scholar] [PubMed]
- Lowery JT, Ahnen DJ, Schroy PC, Hampel H, Baxter N, et al. (2016) Understanding the contribution of family history to colorectal cancer risk and its clinical implications: A state-of-the-science review. Cancer 122(17): 2633-2645.
[Cross Ref] [Google Scholar] [PubMed]
- Nagelhout E, Comarell K, Samadder N, Wu Y (2017) Barriers to colorectal cancer screening in a racially diverse population served by a safety-net clinic. J Community Health 42: 791-796.
[Cross Ref] [Google Scholar] [PubMed]
- Wang H, Roy S, Kim J, Farazi PA, Siahpush M, et al. (2019) Barriers of colorectal cancer screening in rural USA: A systematic review. Rural Remote Health 19: 5181.
[Cross Ref] [Google Scholar] [PubMed]
- Ylitalo K, Camp B, Umstattd MMR, Barron LA, Benavidez G, et al. (2019) Barriers and facilitators of colorectal cancer screening in a Federally Qualified Health Center (FQHC). J Am Board Fam Med 32(2): 180-190.
[Cross Ref] [Google Scholar] [PubMed]
- Rauscher GH, Johnson TP, Cho YI, Walk JA (2008) Accuracy of self-reported cancer-screening histories: A meta-analysis. Cancer Epidemiol Biomarkers Prev 17(4): 748-757.
[Cross Ref] [Google Scholar] [PubMed]
- MacLaughlin KL, Jacobson RM, Radecki CR, Wilson PM, Jacobson DJ, et al. (2019) Trends over time in pap and pap-hpv cotesting for cervical cancer screening. J Womens Health 28(2): 244-249.
[Cross Ref] [Google Scholar] [PubMed]
- Miller KD, Sauer AG, Ortiz AP, Fedewa, SA, Pinheiro PS, et al. (2018) Cancer statistics for Hispanics/Latinos, 2018. CA Cancer J Clin 68(6): 425-445.
[Cross Ref] [Google Scholar] [PubMed]
- Ward EM, Sherman RL, Henley SJ, Jemal A, Siegel DA, et al. (2019) Annual report to the nation on the status of cancer, 1999-2015, Featuring Cancer in Men and Women ages 20-49. J Natl Cancer Inst 111(12): 1279-1297.
[Cross Ref] [Google Scholar] [PubMed]
- Sankare IC, Bross R, Brown AF, Del PHE, Jones LF, et al. (2015) Strategies to build trust and recruit African American and Latino community residents for health research: A cohort study. Clin Transl Sci 8(5): 412-420.
[Cross Ref] [Google Scholar] [PubMed]
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3524
- [From(publication date): 0-2022 - Nov 26, 2025]
- Breakdown by view type
- HTML page views: 2954
- PDF downloads: 570