Association between environmental levels of PM 2.5 and mortality from SARS-CoV-2 in inhabitants of Mexico City
Received: 05-Jan-2023 / Manuscript No. JIDT-23-85631 / Editor assigned: 09-Jan-2023 / PreQC No. JIDT-23-85631 (PQ) / Reviewed: 23-Jan-2023 / QC No. JIDT-23-85631 / Revised: 30-Jan-2023 / Manuscript No. JIDT-23-85631 (R) / Published Date: 06-Feb-2023 DOI: 10.4172/2332-0877.1000529
Abstract
Objective: To evaluate the association between exposure to environmental levels of PM2.5 and mortality from SARS-CoV-2 in inhabitants of Mexico City.
Material and Methods: A secondary analysis with the total number of deaths from COVID-19 in residents of Mexico City as well as 25 municipalities in the interior of the Republic was carried out. Environmental levels of PM2.5 were between 2018 and 2021. Bivariate analysis and multivariate logistic regression were performed.
Results: A total of 1,083,175 cases of COVID-19 were included, with 57,384 deaths (5.3%), of which 30,561 were in residents with exposure to more than 20 μg/m3 of PM2.5 (OR 1.27, CI 95%: 1.25 to 1.29). When performing the multivariate analysis, an OR of 1.39 (CI 95%:1.36 to 1.43) was observed.
Keywords: COVID-19; Environmental pollution; PM2.5; Death
Introduction
In December 2019, the Chinese province of Wuhan became the epicenter of an unknown etiology pneumonia, that as the days passed, started to increase the global attention and concern. On January the 7th of 2020, Chinese health authorities identified the causative agent as an RNA virus that would be known as SARS-CoV-2, which caused the COVID-19 disease. At the time of writing of this manuscript, the disease has caused more than 490,000,000 cases of contagion and more than 6,100,000 deaths worldwide [1]. In addition, more than 5,700,000 cases and 320,000 deaths have been reported in Mexico [2,3].
One of the epidemiological aspects that has drawn attention to the infections and deaths caused by the COVID-19 is its variable behavior between different regions, which could be explained in part by socioeconomic, demographic, geographical, and climatic conditions. Pansini and Fornacca published one out of the first studies documenting the proportional relationship between average annual levels of particulates less than 2.5 and 10 microns (PM2.5 and PM10), nitrogen dioxide (NO2), ozone (O3) and carbon monoxide (CO) in China, Italy, and the United States of America (USA) with the number of SARS-CoV-2 infections [4,5]. This relationship has been confirmed by subsequent studies that have shown that exposure to high levels of pollution may increase the vulnerability of the population to the effects of COVID-19 [6]. This is based on the fact that chronic exposure to high concentrations of PM2.5 has been associated with the development and/or exacerbation of respiratory diseases such as asthma, bronchitis and Chronic Obstructive Pulmonary Disease (COPD) [7]. Because of their size and aerodynamic capacity, PM2.5 are able to evade the filtration system of the respiratory system, reach the alveoli and accumulate by diffusion, which generates an inflammatory and thrombogenic response, as well as increasing the number of Angiotensin-2 Converting Enzyme (ACE-2) receptors in the respiratory epithelium, which is the same receptor the protein S blinds to the SARS-CoV-2 [8,9]. In addition, the relation between the PM2.5 to COVID-19 mortality could have other explanations as these particles are composed of a mixture of organic and inorganic substances such as sulfates, nitrates, ammonium, sodium chloride, coal, dust, and water, which could serve as a vector increasing air transmissibility [7,10-14].
The aim of this study is researching the probable association between chronic exposure to elevated environmental levels of PM2.5 (greater than 20 μg/m3) and COVID-19 mortality in Mexico City inhabitants. In addition, as a secondary objective, studying this association with other pollutants such as PM10, NO2 and O3 was proposed.
At present, the method based on Nucleic Acid Amplification Technology (NAAT), as Real-Time reverse transcriptase Polymerase Chain Reaction (RT-PCR), is considered the gold standard for detecting SARS-CoV-2. The RT-PCR could detect the SARS-CoV-2 genetic materials in many types of samples, including sputum, nasopharyngeal or oropharyngeal swabs, and respiratory secretions, with a high sensitivity and specificity [4]. However, a RT-PCR test is expensive, takes at least 2 hours-3 hours to obtain the result, and requires well-equipped facilities and experienced laboratory workers. These disadvantages limit its use for fast and massive diagnostics in controlling the virus spread. Alternative methods, such as rapid antigen test, with the ability to identify the virus in a fast, cheap way is needed.
Rapid Antigen Diagnostic tests (RAD) detect viral antigen in samples by the immobilized coated SARS-CoV-2 antibody on the device [5]. The test can provide a result in 15 minutes-20 minutes and can be operated and interpreted by individuals without specialized instrument and knowledge. The RADs assays have been used for the diagnosis of SARS-CoV-2 infection in Point-of-Care (POC) settings worldwide [6- 9]. After two years of COVID-19 pandemic, many countries chose to lift or remove the pandemic restrictions, and the PCR test was only given to the groups that need it the most, such as patients, and health care and elderly care staff. Some countries, such as Sweden, recommended that you take self-antigen tests if you develop symptoms of COVID-19 [10], which underlined that there is growing importance of the utilization of SARS-CoV-2 RAD tests to combat the pandemic.
With the progression of COVID-19, many new SARS-CoV-2 variants with increased transmissibility, disease severity are emerging [11]. These new variants will bring additional challenges to current diagnosis methods, including the RAD test. There are more than 300 RAD kits that have been certified in European Union (EU) as of April 2022 [12]. The EU Technical Working Group is continuously monitoring the performance of current RAD tests, especially in the context of emerging SARS-CoV-2 variants and potential breakthrough infections among vaccinated individuals [13]. To address these concerns, there is a need to update the evaluation of the clinical performance of commercial RAD kits for COVID-19 diagnosis. In this work, two independent studies were carried out to evaluate the filed performance of the all Test SARS-CoV-2 Antigen Rapid Test (COVID- 19 Antigen Rapid Test) (Swab). Its efficacy was compared with that of the Fia Test, Abbott Panbio, and Siemens COVID-19 antigen rapid test kits, and with RT-PCR results in Sweden. Another set of comparative trials to evaluate the clinical effectiveness of the candidate kits was conducted in Rome.
Materials and Methods
With cut-off date of August 27, 2021, a transversal secondary analysis of the open database of the National Epidemiological Surveillance System of the General Directorate of Epidemiology of the Mexican Ministry of Health was conducted, where the total number of confirmed cases and deaths by COVID-19 in residents of the city Halls of Mexico City were included. In addition, residents of the capitals of the states of Aguascalientes, Chiapas, Chihuahua, Durango, Oaxaca, Queretaro and Yucatan were included; as well as residents of the municipalities of Abasolo, Celaya, Guanajuato, Irapuato, Leon, Salamanca, San Luis de la Paz, San Miguel de Allende and Silao in the State of Guanajuato; as well as Atononilco, Atitalaquia, Pachuca, Tizayuca, Tepeji del Rio, Tula, Huichapan, Tulancingo and Tepeapulco in the State of Hidalgo. On the number of cases and deaths by COVID-19, information was obtained, as well as on the main demographic variables and population comorbidities. Subsequently, the environmental levels of PM2.5 were recorded, as well as PM10, NO2 and O3 corresponding to the subject municipalities or mayors, which was obtained from the reports of the automatic environmental monitoring networks of the National air quality information system from January 1 2018, to August 27, 2021. Cases of immigrants and those in which SARS-CoV-2 infection could not be confirmed were excluded, such as studies invalidated by the laboratory, cases without confirmatory evidence, suspicious cases or with negative test, as well as the reports of mayors or municipalities with measurements of absent or incomplete environmental pollutants, for which the criterion of the Mexican Official Standard NOM-025-SSA1-2014 was taken. In this case, it is established that there must be at least three quarters with at least 75% of the data [15].
For univariate analysis, quantitative variables are presented in measures of central tendency and dispersion according to their type of distribution, and qualitative variables are presented in percentages. For the bivariate statistical analysis, the U Mann Whitney and Squared Chi tests were used. To establish a comparison between groups, average exposure to more than 20 μg/m3 for PM2.5, average exposure to more than 35 μg/m3 for PM10, average exposure to more than 10 ppb for NO2, and average exposure to more than 45 ppb for O3 were established as cutoff points. To adjust the main confounders, a multiple logistic regression model was performed considering the main comorbidities associated with mortality from COVID-19 such as diabetes, arterial hypertension, obesity, asthma, Cardiovascular Disease (CVD), Chronic Renal Disease (CRD), Chronic Obstructive Pulmonary Disease (COPD) and immunosuppression. For all tests, the values of p ≤ 0.05 were considered as statistically significant. RStudio statistical software version 4.1.0 © 2009-2021 was used.
The present study was evaluated and approved by the Local Research Committee of the High Specialty Medical Unit “Luis Castelazo Ayala” of the Mexican Social Security Institute under number R-2021-3606-011. Since it was carried out based on reviewed documentary files, and in accordance with the General Health Law on Research, it was classified as presenting a “lower risk to the minimum”.
Results
1,083,175 confirmed cases of COVID-19 were studied in the selected regions, of which 759,087 people (70.1%) were residents of Mexico City, and 324,039 people (29.9%) were residents of the country’s inland. Of the total population, 57,384 deaths were recorded (5.3%), which represents a mortality rate of 310.7 per 100,000 inhabitants and a case fatality rate of 0.05%. The general characteristics of the study population are presented in Table 1. Furthermore, the distribution of confirmed cases, prevalence (per 100,000 inhabitants), deaths, mortality rate (per 100,000 inhabitants) and annual average of PM2.5 per Mayor or Municipality of study is presented in Table 2.
| Variable | PM2.5<20 μg/m3 | PM2.5>20 μg/m3 | p |
|---|---|---|---|
| Age in years, median (IQR) | 38 (27, 52) | 40 (28, 53) | <0.01* |
| Female sex, N (%) | 274,748 (25.4) | 252,477 (23.3) | <0.01** |
| Comorbidities, N (%) | |||
| Arterial hypertension | 70.427 (6.5) | 66,961 (6.2) | <0.01** |
| Obesity | 57,167 (5.3) | 57,875 (5.3) | <0.01** |
| Diabetes | 52,480 (4.8) | 51,130 (4.7) | <0.01** |
| Smoking | 45,761 (4.2) | 46,013 (4.2) | <0.01** |
| Asthma | 10,566 (1.0) | 10,532 (1.0) | <0.01** |
| Cardiovascular disease | 5,828 (0.5) | 6,361 (0.6) | <0.01** |
| Chronic renal disease | 5,053 (0.5) | 5,183 (0.5) | <0.01** |
| Chronic obstructive pulmonary disease | 3,894 (0.4) | 4,342 (0.4) | <0.01** |
| Immunosuppression | 3,275 (0.3) | 3,259 (0.3) | <0.01** |
| Deaths, N (%) | 26,823 (2.5) | 30,561 (2.8) | <0.01** |
| Survivors, N (%) | 540,765 (49.9) | 485,026 (44.8) | <0.01** |
Note: *:U Mann Whitney; **:Squared Chi; IQR:Interquartile Range
Table 1: Baseline characteristics of the study population (N=1,083,175).
| State | Municipality or mayor | Confirmed cases* | Prevalence | COVID-19 deaths | Mortality rate | PM2.5 levels** |
| Mexico City | Alvaro Obregon | 1,27,394 | 16,781.40 | 3,137 | 413.2 | 17.4 |
| Mexico City | Azcapotzalco | 45,424 | 10,509.80 | 2,554 | 590.9 | 23.5 |
| Mexico City | Benito Juarez | 30,459 | 7,015.70 | 1,373 | 316.2 | 20.1 |
| Mexico City | Coyoacan | 48,684 | 7,923.20 | 2,546 | 414.4 | 19.7 |
| Mexico City | Cuajimalpa | 16,013 | 7,356 | 556 | 255.4 | 17.5 |
| Mexico City | Cuauhtemoc | 45,448 | 8,325.60 | 2,506 | 459.1 | 24 |
| Mexico City | Gustavo A. Madero | 1,01,198 | 8,624.70 | 5,792 | 493.6 | 23.7 |
| Mexico City | Iztapalapa | 1,40,013 | 7,628.10 | 7,491 | 408.1 | 23.2 |
| Mexico City | Miguel Hidalgo | 30,270 | 7,303.30 | 1,333 | 321.6 | 25 |
| Mexico City | Tlalpan | 85,176 | 12,169.30 | 2,013 | 287.6 | 18.9 |
| Mexico City | Venustiano Carranza | 41,809 | 9,422.70 | 2,144 | 483.2 | 23.8 |
| Mexico City | Xochimilco | 47,208 | 10,676.20 | 1,331 | 301 | 16.7 |
| Aguascalientes | Aguascalientes | 25,661 | 2,704.00 | 2,256 | 237.7 | 11.1 |
| Chiapas | Tuxtla Gutierrez | 8,085 | 1,338.30 | 730 | 120.8 | 17 |
| Chihuahua | Chihuahua | 20,028 | 2,135.90 | 1,941 | 207 | 13.6 |
| Durango | Durango | 24,721 | 3,589.50 | 1,242 | 180.3 | 16.45 |
| Guanajuato | Abasolo | 748 | 812.7 | 98 | 106.5 | 14.6 |
| Guanajuato | Celaya | 13,595 | 2,608.60 | 958 | 183.8 | 19.8 |
| Guanajuato | Guanajuato | 6,176 | 3,175.30 | 374 | 192.3 | 12.6 |
| Guanajuato | Irapuato | 15,248 | 2,571.50 | 1,224 | 206.4 | 19.7 |
| Guanajuato | Leon | 50,651 | 2,942.70 | 4,167 | 242.1 | 20.6 |
| Guanajuato | Salamanca | 7,471 | 2,732.50 | 604 | 220.9 | 21.9 |
| Guanajuato | San Luis de la Paz | 2,744 | 2,134.80 | 214 | 166.5 | 11.5 |
| Guanajuato | San M. de Allende | 3,558 | 2,037.60 | 230 | 131.7 | 13.1 |
| Guanajuato | Silao | 3,763 | 1,848.60 | 397 | 195 | 25.1 |
| Hidalgo | Atotonilco de Tula | 880 | 1,408.70 | 126 | 201.7 | 32.4 |
| Hidalgo | Atitalaquia | 649 | 2,058.70 | 119 | 377.5 | 23 |
| Hidalgo | Pachuca | 11,291 | 3,592.10 | 1,277 | 406.3 | 21.7 |
| Hidalgo | Tizayuca | 4,091 | 2,430.70 | 457 | 271.5 | 21.7 |
| Hidalgo | Tepeji del Rio | 2,130 | 2,352.40 | 261 | 288.3 | 20.9 |
| Hidalgo | Tula de Allende | 2,718 | 2,361.30 | 402 | 349.2 | 19.3 |
| Hidalgo | Huichapan | 798 | 1,682.70 | 91 | 191.9 | 15.5 |
| Hidalgo | Tulancingo | 4,098 | 2,433.90 | 507 | 301.1 | 14.6 |
| Hidalgo | Tepeapulco | 2,001 | 3,557.60 | 206 | 366.3 | 14.2 |
| Oaxaca | Oaxaca | 16,846 | 6,217.30 | 835 | 308.2 | 11.9 |
| Queretaro | Queretaro | 57,996 | 5,524.60 | 3,169 | 301.9 | 12.3 |
| Yucatan | Merida | 38,092 | 3,827.80 | 2,735 | 274.8 | 12.8 |
Note: *:National Epidemiological Surveillance System; **:Annual average levels between 2018-2021
Table 2: Distribution of cases and deaths from COVID-19 and average exposure to PM2.5 levels.
The result of the bivariate analysis (using Pearson’s Squared Chi), which establishes the association between mortality caused by COVID-19 and the average exposure to more than 20 μg/m3 of PM2.5, more than 35 μg/m3 of PM10, more than 10 ppb of NO2, and more than 45 ppb of O3 in the study population, as well as the main comorbidities associated with COVID-19 mortality are presented in Table 3. In addition, the Population Attributable Risk (PAR) values, expressed in percentage, are presented.
| Deaths N=57,384 (%) | Survivors N=1,025,742 (%) | OR* | 95% IC | PAR (%) | ||
|---|---|---|---|---|---|---|
| Environmental pollutant | >20 μg/m3 PM2.5 | 30,561 (53.2) | 485,026 (47.2) | 1.27 | 1.25-1.29 | 14.7 |
| >35 μg/m3 PM10 | 38,151 (66.5) | 596,079 (58.1) | 1.81 | 1.78-1.83 | 21.1 | |
| >10 ppb NO2 | 45,334 (79) | 854,257 (83.2) | 1.32 | 1.29-1.34 | 13.9 | |
| >45 ppb O3 | 30,230 (52.6) | 680,182 (66.3) | 0.57 | 0.52-0.58 | - | |
| Comorbidities | Diabetes | 20,324 (35.4) | 83,286 (8.1) | 6.21 | 6.09-6.32 | 28.4 |
| Arterial hypertension | 24,985 (43.5) | 112,403 (10.9) | 6.27 | 6.16-6.38 | 34.8 | |
| Obesity | 12,059 (21.1) | 102,983 (10.1) | 2.38 | 2.33-2.43 | 11.6 | |
| Cardiovascular disease | 2,699 (4.7) | 9,480 (0.9) | 5.29 | 5.06-5.52 | 3.5 | |
| Chronic renal disease | 3,656 (6.4) | 6,580 (0.6) | 10.5 | 10.1-11.0 | 5.4 | |
| COPD | 2,568 (4.4) | 5,668 (0.5) | 8.43 | 8.04-8.84 | 3.7 | |
| Immunosuppression | 1,150 (2.1) | 5,384 (0.5) | 3.88 | 3.63-4.13 | 1.4 | |
| Male sex | 33,493 (58.4) | 463,406 (45.2) | 1.88 | 1.84-1.91 | 28.5 | |
Note: COPD:Chronic Obstructive Pulmonary Disease; PAR:Population Attributable Risk; *:Squared Chi
Table 3: Risk of death from COVID-19 according to exposure to environmental pollutants and the presence of comorbidities.
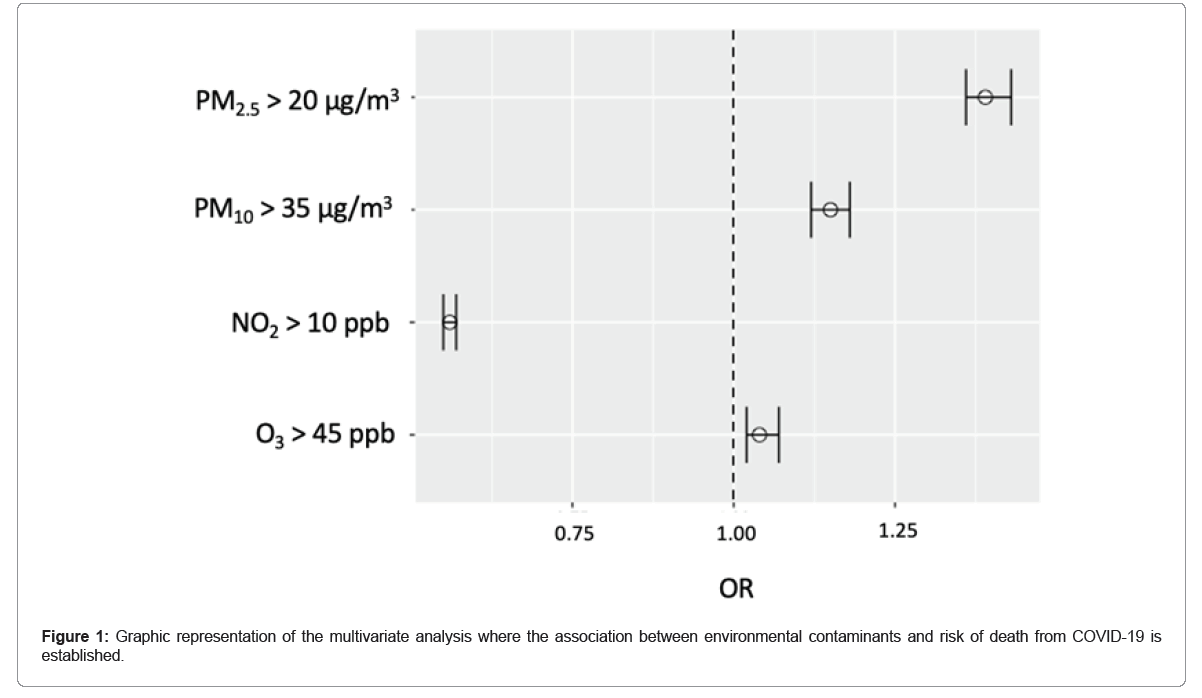
For the multivariate analysis, a logistic regression model was performed, which included the pollutants studied and the main comorbidities associated with COVID-19 (Table 4 and Figure 1). COVID-19 mortality was found to have an adjusted OR of 1.39 (95% CI: 1.36 to 1.43) when exposure was greater than 20 μg/m3 of PM2.5, as well as OR of 1.15 (95% CI 1.12 to 1.18) for exposure greater than 35 μg/ m3 of PM10, of 1.02 (95% CI 1.02 to 1.07) for exposure of more than 10 ppb of NO2, and OR of 0.56 (95% CI 0.55 to 0.57) for exposure of more than 45 ppb of O3.
| COVID-19 deaths (n= 57,384) | ||||
|---|---|---|---|---|
| B | OR | 95% IC | p | |
| >20 μg/m3 PM2.5 | 0.33 | 1.39 | 1.36-1.43 | <0.01 |
| >35 μg/m3 PM10 | 0.14 | 1.15 | 1.12-1.18 | <0.01 |
| >10 ppb NO2 | 0.04 | 1.04 | 1.02-1.07 | 0.002 |
| >45 ppb O3 | -0.56 | 0.56 | 0.55-0.57 | <0.01 |
| Diabetes | 1.08 | 2.95 | 2.89-3.02 | <0.01 |
| Arterial hypertension | 1.17 | 3.22 | 3.15-3.29 | <0.01 |
| Obesity | 0.38 | 1.47 | 1.43-1.51 | <0.01 |
| Cardiovascular disease | 0.51 | 1.68 | 1.59-1.77 | <0.01 |
| Chronic renal disease | 1.16 | 3.2 | 3.05-3.37 | <0.01 |
| Chronic obstructive pulmonary disease | 1.23 | 3.45 | 3.26-3.65 | <0.01 |
| Immunosuppression | 0.67 | 1.95 | 1.80-2.11 | <0.01 |
Note: Nagelkerke R2=0.16, p<0.001
Table 4: Multivariate model with the adjustment of contaminants and the main comorbidities associated with COVID-19.
Discussion
It has been observed that COVID-19 mortality has a relationship with the presence of comorbidities such as arterial hypertension, diabetes, heart disease, COPD, renal disease, or immunosuppression. However, there are other factors as environmental pollutants, which can play a relevant role. In this sense, and based on the results of our study, we observed that chronic exposure to high levels of PM2.5, PM10 and NO2 represents an increased risk of death from SARS-CoV-2 infection, which when expressed in terms of the Population Attributable Risk (PAR) represented a 14.7% for PM2.5, 21.1% for PM10, and 13.9% for NO2. It is worth mentioning that the PAR represents the disease incidence proportion that would be avoided in the general population if exposure to the risk factor were eliminated. In this case, it was related to the environmental pollutants. Unlike the ratio of possibilities (OR) and Relative Risk (RR), the PAR takes into account the number of individuals exposed in the population. The usefulness of the PAR calculation is that it can be used to plan public health policies in which specific disease prevention strategies need to be identified. In other words, based on our study, it could serve to identify the population impact of COVID-19 deaths when implementing environmental measures (PM2.5, PM10 and NO2) aimed at reducing the levels of environmental pollutants below the limits studied [16,17].
When analyzing the findings of the present study, we observed that they are consistent with those documented in other scientific reports that, although they are based on different methodologies, they have confirmed the relationship between death by COVID-19 and exposure to high levels of environmental pollutants. Frontera’s publication was one of the first ones, who in May 2020 observed a greater number of cases of death by COVID-19 in the most polluted regions of northern Italy, being up to twice as many compared to less polluted areas [18]. On their behalf, Wu and collaborators at Johns Hopkins University conducted quantitative research on the role of PM2.5 and COVID-19 mortality, and reported that by the increase in 1 μg/m3 of PM2.5, the risk of death by SARS-CoV-2, increase in 8%, being this study one of the most important, since it included the study of 3,000 US counties (representative of 98% of the population) and whose results give rise to the present research [19]. In Italy, Coker also observed that the 1 μg/m3 increase in PM2.5 was associated with 9% (95% CI: 6%-12%) increased risk of death from COVID-19. These results are below the level of risk found in our study, which could be due to the statistical methodology and the higher levels of PM2.5 of our study regions [20]. In Latin America, Vasquez-Apestegui and collaborators were the first to study the population exposure to PM2.5 between 2010 and 2016 in 24 Lima districts, and to establish their relationship with COVID-19 they applied a multivariate regression model, noting a significant association between cases and deaths with high exposure to PM2.5. In Mexico, Cabrera-Cano and collaborators conducted an ecological study in 25 cities, in which they found a non-significant association between levels of PM2.5 and mortality by COVID-19, which differs from our results [21]. In this study, only the pollutant reports of five months of the year 2020 were considered. Due to the fact that, we could present the discrepancy [22].
Regarding the study of PM10, Márques and collaborators studied in Barcelona the effect of high chronic exposure to this pollutant, in which they observed a higher death risk caused by COVID-19 (OR 2.37, 95% CI 1.71-3.32) than some comorbidities such as asthma, obesity, diabetes or COPD, concluding that per 1 µg/m3 increase in PM10, the death risk caused by COVID-19 increases by 2.68% (95% CI 0.53%-5.58%). Additionally, when studying 55 Italian provinces, Coccia observed a higher number of COVID-19 infections in regions that exceeded the PM10. limit levels by more than 100 days [23]. By measuring global exposure to fine atmospheric particles by satellite, Pozzer estimated that environmental pollution contributes 15% to COVID-19 mortality [24]. Although the afore mentioned studies were carried out under different methodologies, their results are compatible with the findings of our study, in which we observed a 15% increase in death risk caused by COVID-19 in regions whose exposure to PM10 is equal to or greater than 35 μg/m3 [25].
In the case of studies that include NO2, in China, Zhu observed that due to the increase of every 10 μg/m3 of NO2, there was a 6.94% increase of COVID-19 daily cases. In addition, in the United States, Liang and collaborators reported that due to the increase in the inter-quartile range of NO2 (4.6 ppb), there was an 11.2% increase (95% CI 3.4 to 19.5%) in mortality due to COVID-19 [26]. In this way, it coincides with our study, in which we observed a PAR of 13.9% and a discrete increase of 4% in the death risk caused by COVID-19 with chronic exposure to more than 10 ppb of NO2 [27]. In their respective studies, Zoran and Bashir documented results different from ours, finding no association between the death risk and the exposure to high levels of NO2 [28, 29].
Few studies have explored the effect of O3 on mortality caused by COVID-19. One of them was that of Ayoub, who reported that due to the increase in 1 unit of ozone, there were 4.4% more deaths caused by SARS-CoV-2. In New York, Adhikari and collaborators observed that acute exposure to high ozone concentrations, along with weather variables such as wind speed, temperature, and humidity, was associated with more cases of COVID-19 [30]. These results differ from our study findings, where not only we could not verify the association between ozone exposure and mortality caused by COVID-19, but we also observed an apparent protective effect (OR 0.56, 95%CI; 0.55 to 0.57), which should be taken with reservation, since the methodological design of our study did not include the evaluation of atmospheric and environmental variables [31].
One of the challenges in developing the methodological design of the present study was the choice of cut-off points for PM concentrations as the WHO, in its Guide to Global Air Quality 2021 states that the recommended levels for avoiding health risks are 5 μg/m3 for PM2.5, and 15 μg/m3 for PM10. However, these references cannot be applied in our country context, since no region studied has registered equal or lower levels than those recommended, which could be interpreted as the need to establish more realistic cut-off points according to the current context, or that national environmental policies need to be thoroughly reviewed and improved [8,15].
Conclusion
The pandemic is not over, so our results have a limitation inherent in its final course, as well as other variables that may affect mortality by COVID-19 and that were not included in the study, such as the socioeconomic stratum, population mobility, vaccination coverage, the effect of seasons and the temperature. Another limitation of the study was the measurement of pollutants levels, since not all are consistent and homogeneous in the different monitoring stations, so four Mexico City Mayors could not be included (Iztacalco, Magdalena Contreras, Milpa Alta and Tlahuac). For the same reason, it was not possible to explore other pollutants such as carbon monoxide, nitric oxide or sulphur dioxide. However, the measurements of PM2.5, PM10, NO2 and O3 that were included in the study filled the national Air Quality Standards established in the “Official Mexican Environmental Health Standard Permissible limit values for the concentration of suspended particles PM10 and PM2.5 in air and criteria for their assessment”. Therefore, more studies will be needed to help differentiate the role of confounders and environmental pollutants as risk factors in COVID-19 mortality. Chronic exposure to elevated levels of PM2.5, as well as PM10 and NO2 is associated with increased death risk caused by COVID-19 in Mexico City residents.
Acknowledgment
Escuela Superior de Medicina. Instituto Politécnico Nacional, Mexico.
References
- Wang C, Horby PW, Hayden FG, Gao GF (2020) A novel coronavirus outbreak of global health concern. Lancet 395:470-473.
[Crossref] [Google Scholar] [PubMed]
- Yesudhas D, Srivastava A, Gromiha MM (2021) COVID-19 outbreak: History, mechanism, transmission, structural studies and therapeutics. Infection 49:199-213.
[Crossref] [Google Scholar] [PubMed]
- COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU), John Hopkins University and Medicine Coronavirus Resource Center, 2021.
- Bellali H, Chtioui N, Chahed M (2020) Factors associated with country-variation in COVID-19 morbidity and mortality worldwide: An observational geographic study COVID-19 morbidity and mortality country-variation. MedRxiv 5:1-37.
- Biktasheva IV (2020) Role of a habitat’s air humidity in COVID-19 mortality. Sci Total Environ 736:138763.
[Crossref] [Google Scholar] [PubMed]
- Pansini R, Fornacca D (2020) Initial evidence of higher morbidity and mortality due to SARS-CoV-2 in regions with lower air quality. MedRxiv 5:1-16.
- Amnuaylojaroen T, Parasin N (2021) Association between COVID-19, air pollution, and climate change. Front Public Health 9:662499.
[Crossref] [Google Scholar] [PubMed]
- Ambient air pollution: A global assessment of exposure and burden of disease, World Health Organization, 2016.
- Shin S, Bai L, Burnett RT, Kwong JC, Hystad P, et al. (2021) Air pollution as a risk factor for incident chronic obstructive pulmonary disease and Asthma: A 15-year population-based cohort study. Am J Respir Crit Care Med 203:1138-1148.
[Crossref] [Google Scholar] [PubMed]
- Cole MA, Ozgen C, Strobl E (2020) Air pollution exposure and COVID-19 in Dutch municipalities. Environ Resour Econ (Dordr) 76:581-610.
[Crossref] [Google Scholar] [PubMed]
- Xing Y-F, Xu Y-H, Shi M-H, Lian Y-X (2016) The impact of PM2.5 on the human respiratory system. J Thorac Dis 8(1):E69-E74.
[Crossref] [Google Scholar] [PubMed]
- Beyerstedt S, Casaro EB, Rangel EB (2021) COVID-19: Angiotensin-Converting Enzyme 2 (ACE2) expression and tissue susceptibility to SARS-CoV-2 infection. Eur J Clin Microbiol Infect Dis 40:905-919.
[Crossref] [Google Scholar] [PubMed]
- Travaglio M, Yu Y, Popovic R, Selley L, Santos N, et al. (2021) Leal Links between air pollution and COVID-19 in England. Environ Pollut 268:115859.
[Crossref] [Google Scholar] [PubMed]
- Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, et al. (2018) The Lancet commission on pollution and health. Lancet 391:462-512.
[Crossref] [Google Scholar] [PubMed]
- Official Mexican STANDARD NOM-025-SSA1-2014, environmental health. Permissible limit values for the concentration of suspended particles PM10 and PM2.5 in ambient air and criteria for their evaluation. RedBoa, 2014.
- Fajardo-Gutiérrez A (2017) Measurement in epidemiology: Prevalence, incidence, risk, impact measures. Rev Alerg Mex 64:109-120.
[Crossref] [Google Scholar] [PubMed]
- García FJN, Urrea AP (1990) Attributable risk: Its forms, uses and interpretation. Gac Sanit 4:112-117.
[Crossref] [Google Scholar] [PubMed]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G (2020) Severe air pollution links to higher mortality in COVID-19 patients: The “double-hit” hypothesis. J Infect 81:255-259.
[Crossref] [Google Scholar] [PubMed]
- Wu X, Nethery RC, Sabath BM, Braun D, Dominici F (2020) Exposure to air pollution and COVID-19 mortality in the United States. 2020:1-36.
[Crossref] [Google Scholar] [PubMed]
- Coker ES, Cavalli L, Fabrizi E, Guastella G, Lippo E, et al. (2020) The effects of air pollution on COVID-19 related mortality in northern Italy. Environ Resour Econ (Dordr) 76:611-634.
[Crossref] [Google Scholar] [PubMed]
- Vasquez-Apestegui BV, Parras-Garrido E, Tapia V, Paz-Aparicio VM, Rojas JP, et al. (2021) Association between air pollution in Lima and the high incidence of COVID-19: Findings from a post hoc analysis. Res Sq 1:39404.
[Crossref] [Google Scholar] [PubMed]
- Cabrera-Cano ÁA, Cruz JCC, Gloria-Alvarado AB, Álamo-Hernández U, Riojas-Rodríguez H (2021) Association between mortality from COVID-19 and air pollution in Mexican cities. Salud Publica Mex 63:1-8.
[Crossref] [Google Scholar] [PubMed]
- Marquès M, Correig E, Ibarretxe D, Anoro E, Arroyo JA, et al. (2022) Long-term exposure to PM10 above WHO guidelines exacerbates COVID-19 severity and mortality. Environ Int 158:106930.
[Crossref] [Google Scholar] [PubMed]
- Coccia M (2020) Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci Total Environ 729:138474.
[Crossref] [Google Scholar] [PubMed]
- Pozzer A, Dominici F, Haines A, Witt C, Münzel T, et al. (2020) Regional and global contributions of air pollution to risk of death from COVID-19. Cardiovasc Res 116:2247-2253.
[Crossref] [Google Scholar] [PubMed]
- Zhu Y, Xie J, Huang F, Cao L (2020) Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ 727:138704.
[Crossref] [Google Scholar] [PubMed]
- Liang D, Shi L, Zhao J, Liu P, Schwartz J, et al. (2020) Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. medRxiv 2020:1-31.
[Crossref] [Google Scholar] [PubMed]
- Zoran MA, Savastru RS, Savastru DM, Tautan MN (2020) Assessing the relationship between ground levels of ozone (O3) and nitrogen dioxide (NO2) with Coronavirus (COVID-19) in Milan, Italy. Sci Total Environ 740:140005.
[Crossref] [Google Scholar] [PubMed]
- Bashir MF, Ma BJ, Bilal H, Komal B, Bashir MA, et al. (2020) Correlation between environmental pollution indicators and COVID-19 pandemic: A brief study in Californian context. Environ Res 187:109652.
[Crossref] [Google Scholar] [PubMed]
- Meo SA, Abukhalaf AA, Sami W, Hoang TD (2021) Effect of environmental pollution PM2.5, carbon monoxide, and ozone on the incidence and mortality due to SARS-CoV-2 infection in London, United Kingdom. J King Saud Univ Sci 33:101373.
[Crossref] [Google Scholar] [PubMed]
- Adhikari A, Yin J (2020) Short-term effects of ambient ozone, PM2.5, and meteorological factors on COVID-19 confirmed cases and deaths in Queens, New York. Int J Environ Res Public Health 17:4047.
[Crossref] [Google Scholar] [PubMed]
Citation: Alberto MSA, Rodolfo RR, Rocio FV, Anali RGI (2023) Association between Environmental Levels of PM2.5 and Mortality from SARS-CoV-2 in Inhabitants of Mexico City. J Infect Dis Ther 11: 529. DOI: 10.4172/2332-0877.1000529
Copyright: © 2023 Alberto MSA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3193
- [From(publication date): 0-2023 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 2759
- PDF downloads: 434