Assessment of Traumatic Dental Injury in Visually Impaired Children and its Association with Relevant Factors
Received: 06-Jul-2018 / Accepted Date: 26-Jul-2018 / Published Date: 06-Aug-2018 DOI: 10.4172/2161-1165.1000350
Keywords: Traumatic dental injury; Health problems; Trauma; Crown fractures
Introduction
The term “disability” has been defined as any impairment that restricts or limits daily activity in some manner. One of the common disabilities being discussed here is visual impairment. Visual impairment encompasses both “low vision and blindness” [1].
The severity and burden of the disability being discussed is estimated to be 180 million people around the world. Four out of five visually impaired people are living in developing countries. According to the census report 2011 of India a total 5.03 lakh were visually impaired, and visually impaired consisted of 18.8% of all the disabled population ranking as the 3rd highest disability in the country [2].
Traumatic injuries are more prevalent in children with disabilities compared with normal children. Blind individuals suffer from many health problems including oral health, which consist of mainly orofacial trauma, dental caries and periodontal diseases, of this orofacial trauma consist of main health hazards for these individuals [3]. Trauma along with fracture of a permanent front tooth is a disturbing experience for the young patient and is a problem whose management requires experience, judgment, and skill perhaps incomparable to any other segment of the dental practice [4].
Many national and international agencies have been set up for the welfare of the blind, this includes “National association for the blind (NAB)”, “The Royal Commonwealth Society for Blind” and “International Agency for prevention of Blindness”, and however there are no separate measures taken for dental health of visually impaired children [5]. Thus it is imperative to assess a part of dental health i.e. traumatic dental injuries (TDI) experienced by this group and associate it with oral health related factors. This is the aim of our study.
Materials and Method
The present study consists of 200 visually impaired children between 8-15 years of age from the area of Pune and Pimpri-Chinchwad [6]. The sampling technique used for selection of students was simple random sampling.
Inclusion criteria were:
• Children with visual impairment as per Revised WHO definition 2006,
• Children between the ages of 8-15 years,
• All those participants who are willing for the survey.
Exclusion criteria were:
• Children on medication that alter salivary flow,
• Children unwilling to participate in the study,
• Children with concomitant handicaps or any systemic medical conditions,
• Children undergoing orthodontic treatment or with history of similar treatment.
The schools selected were such that they were equitably distributed over the area of the city. The study was conducted in 3 schools for blind: Pune school and Home for blind boys- Koregaon Park, Pune School and Home for Blind Girls- Kothrud, Patashibai school and Home for Blind Boys- Bhosari.
Prior to the commencement of the study a permission letter was obtained from the respective school authorities to carry out the study. A Tentative date of the study was mentioned and a brief outline of methodology was verbally explained. The Scientific and Ethical clearance was obtained from the institutional review, Scientific and Ethical committee of Dr. D. Y. Patil Dental College and Hospital, Pimpri. A written informed consent was obtained for every student of the school [7]. The consent was filled in the local (Marathi) language or English depending on the comfort of the guardian.
One principle examiner was trained and calibrated for conducting oral examination using WHO Oral Health Assessment Form in the Department of Public Health Dentistry, Dr. D.Y. Patil Dental College and Hospital, Pimpri, Pune. A pilot study was carried out that was representative of the total sample and was carried out on 20 students. Complete infection control was maintained by the examiner by wearing of mouth mask, gloves, eye ware and an apron. The examination area was arranged for maximum efficiency and ease of operation. The exact arrangement was determined by the physical condition of the site, however certain features were constant. There was a table placed and 3 chair for the subject, examiner and assistant respectively. Lighting was consistent throughout the examination procedure [8,9]. The examination was carried out during the daytime and natural sunlight was used for examination. On rare occasions artificial torch light was used. Data was recorded as per ‘Oral Health assessment form 2013’.
The data was entered in excel sheet and analyzed using SPSS software (version 17). Demographic data like age, sex, class and region were obtained. Parameter of the ‘WHO Oral Health assessment form for Children-2013’ was collected [10]. For association of oral health status with the relevant parameters Chi- square test was performed.
Results
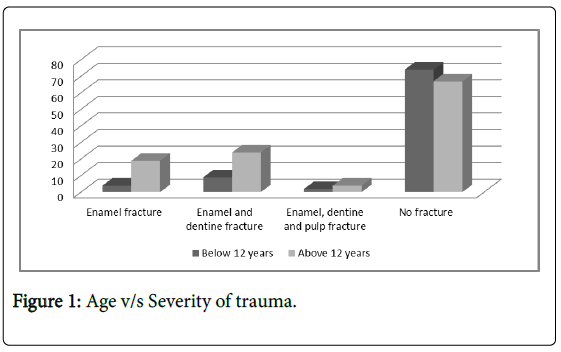
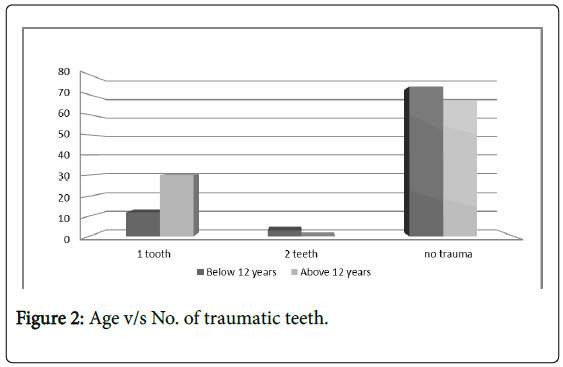
A total of 203 patients were examined for traumatic dental injuries and oral health status. Demographic details of the sample are summarized in Tables 1 and 2. Children were in the age ranging from 8-15 years with a mean age of 12. The sample consisted of 161(79.3%) males and 42(20.7%) females. Total prevalence of traumatic dental injuries in the population was 30.54%. Descriptive statistics were applied to assess severity of trauma and numbers of teeth subjected to trauma, the values were as follows 0.83 ± 0.36 & 0.40 ± 0.66 (Figures 1 and 2).
| Severity of trauma | Total | ||||||
|---|---|---|---|---|---|---|---|
| No fracture | Enamel fracture | Enamel and dentine fracture | Enamel, dentine and pulp fracture | ||||
| Age | Children <12 | Count | 74 | 4 | 9 | 2 | 89 |
| Percentage | 36.50% | 2.00% | 4.40% | 1.00% | 43.80% | ||
| Children >12 | Count | 67 | 19 | 24 | 4 | 114 | |
| Percentage | 33.00% | 9.40% | 11.80% | 2.00% | 56.20% | ||
| Total | Count | 141 | 23 | 33 | 6 | 203 | |
| Percentage | 69.50% | 11.30% | 16.30% | 3.00% | 100.00% | ||
Chi- Square test value: 14.760; significance: 0.002 (significant)
Table 1: Severity of Traumatic Dental Experience and Age.
| No. of teeth in trauma | Total | |||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | ||||
| Age | Children <12 | Count | 74 | 12 | 3 | 89 |
| Percentage | 36.50% | 5.90% | 1.50% | 43.80% | ||
| Children >12 | Count | 67 | 30 | 17 | 114 | |
| Percentage | 33.00% | 14.80% | 8.40% | 56.20% | ||
| Total | Count | 141 | 42 | 20 | 203 | |
| Percentage | 69.50% | 20.70% | 9.90% | 100.00% | ||
Chi- Square test value: 15.011; significance: 0.001 (significant)
Table 2: Association of Traumatic Dental Experience and Age.
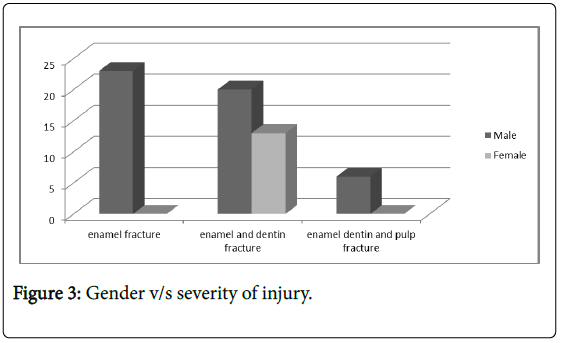
For association of traumatic experience with age, chi square test was applied. It was found that children above 12 years of age had a greater traumatic experience than children below 12 years of age. Crown fractures were most commonly seen form of traumatic injuries, this included enamel fracture, enamel and dentin fracture, enamel dentin and pulp fractures. The occurrence of enamel fractures of children below 12 years (2%) was less than those above 12 years (9.4%). The occurrence enamel and dentine fracture of children below 12 years (4.4%) was less than those above 12 years (11.8%). The occurrence of enamel, dentine and pulp fractures of children below 12 years (1%) was less than of children above 12 years (2%) (Figure 3).
The most common fracture seen was enamel and dentin fracture (16.3%). There were various numbers of teeth that were fractured ranging from 0-2, however 1 tooth (20.7%) was most commonly included in the fracture.
On comparison of gender with traumatic dental injuries, males (24.1%) showed higher prevalence of dental injury than females (6.4%). The most common type of fracture for both males and females was enamel and dentin fractures [11].
Discussion
Prevalence of TDI in normal children differs considerably among various epidemiological studies across the country and around the world. Prevalence of TDI within the country ranges from 8.79 to 18.25%. This wide variation among the studies can be explained by differences in various factors like trauma classification used, dentition status of children, geographical variation & also behavioral difference. Incisors have an important role in aesthetics, phonation, psychological aspect and functional activities. Upper permanent incisors are the most frequently affected teeth by trauma, over 90%, according to Saroglu et al. even 95.72%. Morphology and location make them liable to traumatic injuries. The supporting tissues are more exposed in mixed dentition [12]. Crown fractures without the injury of supporting structures can be found most likely in the permanent dentition. The highlights are on non-complicated crown fractures affecting only the enamel. In the present study traumatic dental experience of the population was evaluated in terms of prevalence and severity. It was found that total prevalence of traumatic injury was 30.54%. A variety of fractures were seen which included enamel fracture, enamel and dentin fracture, and enamel dentine and pulp fractures. The prevalence of traumatic dental experience in visually impaired individuals is found to be of a wide range i.e. from 9%-37%. The prevalence of our study was in accordance with various studies conducted in India by Bhat et al. (32.5%), Agrawal et al. (34.9%), Varghese et al. (37.8%), and O’Donnell et al. (36.4%) which was a study conducted internationally. The prevalence was much higher than that found in sighted individuals. This is proven by studies conducted in India by Baldava et al. (14.9%) and Tangade PS (4.41%). In the above study it was noted that the highest degree of fracture seen was that of enamel and dentine and pulp fracture. The most frequent fracture seen was enamel and dentine fracture, this was in accordance to an international study conducted by O’Donnelled et al. where enamel and dentine fractures were more prevalent than enamel fractures. This is due to the fact that visually impaired children unlike sighted children cannot save themselves from the impact of a fall.
School-age children (7-15 years) are considered to be a risk group to traumatic injuries of the teeth. Trauma in the mixed dentition occurs most frequently between 6 and 9 and between 10 and 12 years of age, and is less frequent in older children (1-5). In our study the age of the patient was correlated with prevalence of trauma. It was found that adolescents above 12 years of age were more prone to trauma as compared to children below 12 years of age [13]. This was in accordance with study conducted by O’Donnelled et al. in Hong Kong. This can be explained by the fact that children indulge in reckless and boisterous activities during this period and are not aware of personal safety.
According to the majority of authors, teeth traumas are more frequent in boys than in girls only in permanent dentition. In mixed dentition no statistically significant differences have been recorded between the genders. There are a number of factors that cause TDI’s. The dominant factors most likely to cause trauma are fall, sports injuries and accidents met at home or outside. The major risk factor for dental injuries is increased overjet and inadequate lip coverage [14]. In our study also a comparison of traumatic injuries experienced by males and females was compared. Males showed a higher rate of traumatic experience than females. Even in sighted population is the same ratio of greater males than females. This may be due to the reason than boys indulge in more aggressive outdoor activities than girls. Moreover, these children being in hostels and not homes do not have constant parental guidance all day long; this may also lead to traumatic dental injuries.
Limitation
The study does not include data on the orthodontic impact on trauma and corresponding links of malocclusion with dental trauma.
Conclusion
The present data suggests that TDIs are prevalent in blind in pune and pimpri chinchwad area. The prevalence is higher in males than in females. The prevalence is also higher in children above 12 years of age than below 12 years of age. There is a positive correlation between age and gender and TDIs. This study provides a baseline data for further related research and implementation of policies in this area.
Acknowledgement
I would like to thank Dr. Ladu Singh Rajpurohit from the department of Public health Dentistry, Dr. DY Patil Dental College, Dr. DY Patil Vidyapeeth for all his help and guidance in this study.
References
- Agrawal A, Bhatt N, Chaudhary H, Singh K, Mishra P, et al. (2013) Prevalence of anterior teeth fracture among visually impaired individuals, India. Indian Journal of Dental Research 24: 664-668.
- Baccetti T, Antonini A (1998) Dentofacial characteristics associated with trauma to maxillary incisors in the mixed dentition. J Clin Pediatr Dent 22: 281-284.
- Baldava P, Anup N (2007) Risk factors for traumatic dental injuries in an adolescent male population in India. J Contemp Dent Pract 8: 35-42.
- Bhat N, Agrawal A, Nagrajappa R, Roy SS, Singh K, et al. (2011) Teeth fracture among visually impaired and sighted children of 12 and 15 years age groups of Udaipur city, India–a comparative study. Dental Traumatology 27: 389-392.
- Hegde R, Agrawal G (2017) Prevalence of traumatic dental injuries to the permanent anterior teeth among 9-to 14-year-old schoolchildren of Navi Mumbai (Kharghar-Belapur Region), India. Int J Clin Pediatr Dent 10: 177.
- Kaba AD, Marechaux SC (1989) A fourteen-year follow-up study of traumatic injuries to the permanent dentition. ASDC J Dent Child 56: 417-425.
- Meštrović S, Pandurić DG, Milošević SA, Ribarić D (2008) Risk factors of traumatic injuries to the upper incisors. Acta stomatologica Croatica 42: 3-10.
- O'Donnell D (1992) The prevalence of nonrepaired fractured incisors in visually impaired Chinese children and young adults in Hong Kong. Quintessence int 23: 363-365.
- Park K (2009) Park's textbook of preventive and social medicine. Jabalpur : M/S Banarsidas Bhanot.
- Ramaiah SD, Maraiah PK (2014) Prevalence of traumatic dental injuries among blind school children in South Karnataka. J Dent Med Sci 13: 18-22.
- Şaroğlu I, Sönmez H (2002) The prevalence of traumatic injuries treated in the pedodontic clinic of Ankara University, Turkey, during 18 months. Dental Traumatology 18: 299-303.
- Shulman JD, Peterson J (2004) The association between incisor trauma and occlusal characteristics in individuals 8–50 years of age. Dental traumatology 20: 67-74.
- Tangade PS (2007) The prevalence of anterior teeth fracture and its relation to malocclusion in 12 and 15 year old school children Belgaum City, India. J Oral Health Commun Dent 1: 7-11.
- Varghese RK, Agrawal A, Mitra A, Fating C (2011) Anterior teeth fracture among visually impaired individuals, India. J Adv Oral Res 2: 39-44.
Citation: Gidwani K (2018) Assessment of Traumatic Dental Injury in Visually Impaired Children and its Association with Relevant Factors. Epidemiology (Sunnyvale) 7: 350. DOI: 10.4172/2161-1165.1000350
Copyright: © 2018 Gidwani K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3238
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 2439
- PDF downloads: 799