Assessment of Outcome of Training of Paramedical Staff in Nebulization Techniques at a Tertiary Care Hospital
Received: 02-Mar-2018 / Accepted Date: 05-Mar-2018 / Published Date: 12-Mar-2018
Abstract
Nebulization is one of the important modalities in the management of obstructive airway diseases (OADs). COPD and Asthma are common OADs. Inhalation therapy is the best recommended route for drug delivery in OADs. Nebulization is one of the modes of delivering inhaled medication. Paramedical staff plays important role in administration of nebulization and explaining nebulization technique to the patients and their relatives. Hence proper training of paramedical staff in nebulization technique and device maintenance is essential. The prospective study was conducted at Bharati Vidyapeeth Medical College Hospital, Pune, and Maharashtra, India. It included training in the form of demonstrations, lecture, videos and hands on training. Staff was assessed with the help of pre and post training questionnaires and technical assessment. Assessment of training and knowledge of paramedical staff is important to achieve good out come and success of treatment in patients with OADs. Such activity should be continuous and ongoing in the form of periodic reassessment and training sessions for sustained improvement in nebulization practices. Training of the staff in clinical practice is crucial.
Keywords: Obstructive airway diseases; Chronic obstructive pulmonary disease; Asthma; Nebulization; Paramedical staff; Nebulization technique; Pre and post training assessment
Introduction
Nebulization is one of the important modalities in the management of obstructive airway diseases (OADs) [1]. COPD and Asthma are most common OADs in clinical practice. Global burden of OADs shows an increasing trend day by day. There are 334 million cases of Asthma and 384 million cases of chronic obstructive pulmonary disease (COPD) estimated worldwide [2,3]. In India, the prevalence of both asthma and COPD are on the higher side and rising as one of the major health problems [2,3]. COPD is currently the third most common cause of death globally and second leading cause of death in India [4,5]. Inhalation therapy is the best-recommended route for drug delivery in OADs and consists of pressurized metered-dose inhalers (pMDIs), dry powder inhalers (DPIs), breath-actuated inhalers (BAIs), soft mist inhalers (SMIs) and nebulizers. The choice of inhaler device depends upon efficacy and safety of the medication, available clinical setting and patient’s ability to use the device properly [6]. Especially, when a patient of OADs requires emergency room visit or when gets hospitalized, may not be in the state of using handheld inhaler device. In such clinical scenarios, nebulization could be preferred and appropriate route for delivery of aerosol-based medications. Nebulization can also be useful in pediatric patients with asthma [7]. Nebulization may be useful in administrating certain antibiotics, like colistin, tobramycin etc., in patients with lower respiratory tract infection. It is a rationale to administer antibiotics in inhaled form. This achieves maximum drug delivery of an antibiotic to the targeted site and potential for systemic side effects of these antibiotics can be limited [8]. A process by which liquid medication is converted into a fine mist that can be inhaled by the patient is known as nebulization [9]. Paramedical staffs of the hospital are trusted hand of doctors for patient care. Aerosol-based inhaled medications are nebulized to the patient usually by paramedical staffs of the hospital. They take the care of nebulizer and its accessories i.e., nebulizer maintenance, nebulization-set cleaning, and disinfection etc. Paramedical staff in the emergency room and wards provides nebulization to patients with OADs, where it is a mainstay of patient’s management. Paramedical staff plays important role in explaining nebulization technique and maintenance to patients and their relatives, who require home nebulization. So they should know proper techniques of giving nebulization and nebulizer maintenance with disinfection of nebulizer accessories. For this purpose, proper training of paramedical staff in nebulization technique and device maintenance is a must.
Methods
It was prospective study, conducted at Bharati Vidyapeeth Medical College Hospital, Pune, and Maharashtra, India. The sample size was n-372, a total number of paramedical staff working at above maintained tertiary care hospital. List of the paramedical staff was obtained by the HR department of the hospital. Study duration was over 3 months. All the participants were divided into 5 batches. It was a structured workshop of around 2 hours each session, which included training of paramedical staff in nebulization techniques and care of nebulizer. Training was done with help of (1) Demonstrations, (2) Lecture, (3) Videos and (4) hands-on training and experience. An assessment was made on the basis of self-administered pre and posttraining session questionnaire and nebulization technique assessment. It was a qualitative data. Collection of data for this study was started after the approval of the Ethical Committee. The collected data were coded and entered into Microsoft Excel sheet. Various rates, ratios, and percentage (%) were calculated. The data was analyzed by using McNemar's test and Wilcoxon sign rank test.
Training protocol
1. Pre training questionnaire: 15 minutes.
2. Pre training nebulization technique assessment: 10 minutes.
3. Training program-Lecture, Videos and hands on experience of nebulization techniques and cleaning and disinfection: 50 minutes.
4. Demonstration of Nebulization techniques with care of Nebulizers: 30 minutes.
5. Post training questionnaire: 15 minutes.
Results
372 paramedical staff participated in this study, n-80 (21.5%) of the paramedical staff was not aware of preferred route of administration for asthma drugs in an emergency. After a training program, n-371 (99.7%) gave right answer (P<0.001).
In this study, n-109 (29.3%) was not certain about the proper device used to give bronchodilators in critical patients, n-57 (15.3%) answered DPI in the pre-training analysis. In post-training analysis n-370 (99.5%) answered correctly, i.e., nebulization (P<0.001). They also become aware of other handheld delivery devices used. In this study, we noted that n-368 (98.9%) did not know about types of nebulizer machines and which one is used commonly. After a training program, n-354 (95.2%) gave the correct answer (P<0.001). In this study, we observed that n-369 (99.2%) were poor in their knowledge about parts of nebulizer-set. In the post-training assessment, n-346 (93.0%) showed improvement in their knowledge (P<0.001).
In our study, n-196 (52.7%) were not aware of the appropriate volume of medication filled in nebulization chamber, n-144 (38.7%) used very low volume (1 to 2 ml) of medication, n-37 (9.9%) used very high volume (10 ml) of medication. In post-training evaluation n-370 (99.5%) answered correctly i.e., 3 to 5 ml (P<0.001). In this study, we found that n-268 (72.0%) had no idea about the appropriate duration for giving nebulization i.e., 5 to 10 minutes. 97.3% (362) answered rightly in the post-training analysis (P<0.001).
In this study, n-344 (92.5%) was oblivious to correct position of the patient for giving nebulization. After a training program, n-348 (93.5%) answered correctly (P<0.001). In this study, we noted that (n-351) 94.4% preferred face mask for giving nebulization and were unaware of benefits of a mouthpiece. In the post-training assessment, n-358 (96.2%) preferred using a mouthpiece for giving nebulization and were aware of its benefits (P<0.001).
In this study, n-253 (68.0%) didn't know the appropriate disinfection methods and duration of which nebulizer accessories should be soaked in medical disinfectant for disinfection. n-356 (95.7%) answered correctly in post-training evaluation (P<0.001). In this study, we noted that n-332 (89.2%) had no idea about the filter in the nebulizer and when to change it. In the post-training analysis, n-359 (96.5%) become aware of the presence of the filter and need to change it when discolored totally (P<0.001).
In this study, n-369 (99.2%) were not certain about which nebulization medication to start in the patient of acute exacerbation of asthma or COPD. n-143 (38.7%) used Normal saline with oxygen flow and n-99 (26.9%) used Budesonide with oxygen flow in pre-training assessment. In the post-training assessment, n-213 (57.3%) gave correct answer i.e., Salbutamol (P<0.001).
In this study, we observed during pre-training assessment that only 9.7% of the paramedical staff had correct knowledge of nebulization technique. Post-training assessment during the study showed that 99.2% of paramedical staff gained correct knowledge of nebulization technique (P<0.001) by training (Tables 1 and 2).
| Questionnaire Used For Assessment | Answers | Pre Training Assessment | Post Training Assessment | P-Value |
|---|---|---|---|---|
| Q1 | Correct | 292 | 371 | <0.001 |
| Preferred route of administration for anti-asthma drugs | Incorrect | 80 | 1 | |
| Q2 | Correct | 263 | 370 | <0.001 |
| Method used to give bronchodilators in critical patients | Incorrect | 109 | 2 | |
| Q3 | Correct | 4 | 354 | <0.001 |
| Enumerate types of nebulizers available and which one is commonly used | Incorrect | 368 | 18 | |
| Q4 | Correct | 3 | 346 | <0.001 |
| Enumerate parts of nebulizer set | Incorrect | 369 | 26 | |
| Q5 | Correct | 176 | 370 | < 0.001 |
| What should be the volume of medication filled in nebulization Chamber | Incorrect | 196 | 2 | |
| Q6 | Correct | 104 | 362 | <0.001 |
| How much is the appropriate time period for nebulization | Incorrect | 268 | 10 | |
| Q7 | Correct | 21 | 358 | <0.001 |
| Which one is preferred to give nebulization mouth piece or face mask and why? | Incorrect | 351 | 14 | |
| Q8 | Correct | 119 | 356 | <0.001 |
| How long nebulizer accessories should be soaked in medical disinfectant for disinfection | Incorrect | 253 | 16 | |
| Q9 | Correct | 40 | 359 | <0.001 |
| When the filter of nebulizer is to be changed | Incorrect | 332 | 13 | |
| Q10 | Correct | 28 | 348 | <0.001 |
| In which position should patient be kept while using nebulizer | Incorrect | 344 | 24 | |
| Q11 | Correct | 3 | 213 | <0.001 |
| In patient of acute attack of OADs, you will first start nebulization with | Incorrect | 369 | 159 |
Table 1: Observations and assessment of paramedical staff with the help of pre and post training questionnaire (total number of correct and incorrect answers).
| Technical Assessment | Pre Training Assessment | Post Training Assessment | P- Value | ||||
|---|---|---|---|---|---|---|---|
| Poor | Good | Best | Poor | Good | Best | ||
| How to clean the nebulizer? | 360 | 12 | 0 | 3 | 289 | 80 | <0.001 |
| Enumerate steps of nebulization? | 336 | 36 | 0 | 3 | 269 | 100 | <0.001 |
Table 2: Technical assessment of paramedical staff (number of paramedical staff).
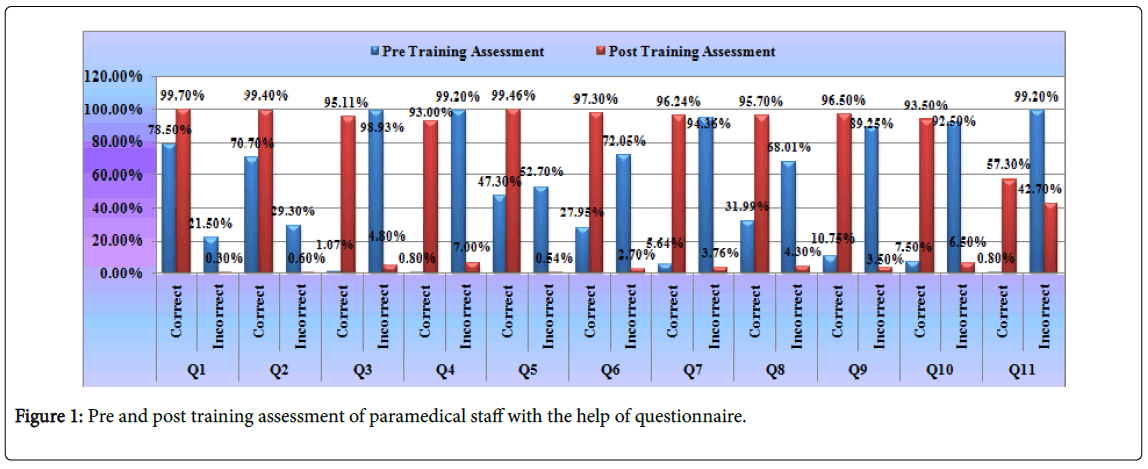
In this study, pre-training assessment showed that only 3.2% of the paramedical staff had correct knowledge about disinfection of nebulizer. Post-training assessment showed that 99.2% of paramedical staff gained correct knowledge about disinfection of nebulizer (P<0.001) (Figure 1).
Discussion
Delivery of inhaled bronchodilator and corticosteroids for patients with acute exacerbation of OADs (Bronchial Asthma or COPD) in emergency settings through appropriate route and device play important role in the initial management of disease [10]. In a country like India, where doctor to patient ratio is low [11], infrequently paramedical staff plays a crucial role in the initial management of a patient in emergency conditions. Hence they should have proper knowledge about an appropriate and effective route, device and drugs to be used in such critical and emergency situations. It is an absolute necessity that paramedical staff should know about types of nebulizer machines available, one commonly used and its working technology. They should also be aware of parts of nebulization set.
As for cleaning and disinfection purpose, all the parts of nebulization set are separated. For re-assembling the device a proper and correct knowledge is essential. This knowledge helps in appropriate functioning of nebulizer machine and eventually, for proper drug delivery [10,12]. Paramedical staff should be aware of various factors related to nebulizers, such as output rates, performance variability and effects of nebulization on various drug formulations [10]. Appropriate quantity of the drug in medication chamber of nebulization set (3 to 5 ml), proper sitting upright position of the patient while giving nebulization, adequate duration of nebulization to the patient (5 to 10 minutes) and use of mouthpiece over face mask for nebulization significantly improves drug delivery [13], reduces side effects of medication and improves patients’ comfort. This will eventually improve the efficacy of the treatment. The British Guidelines on Asthma Management and European Respiratory Society Guidelines on the use of nebulizers have also recommended the same [14-16]. Most of the paramedical staff was unaware of these factors. In the posttraining assessment of this study, there was a noticeable improvement.
Nebulization should be given preferably with air flow nebulizer machines rather than giving with oxygen flow in a patient of acute exacerbations of COPD. If 6 nebulization is given with oxygen, it may lead to carbon dioxide retention and further worsening especially in patients’ of COPD. Edwards et al. in their study found a greater incidence of carbon dioxide retention in COPD patients taking nebulization with oxygen [17] whereas, in patients with acute exacerbations of Asthma, it is preferred to give nebulization with oxygen flow. Gleeson et al. suggested similar conclusions in their study. In the present study, we found that most of the paramedical staff was not performing proper cleaning and disinfection practices for nebulization set and nebulizer maintenance on regular basis. Nebulization set should be dried properly. This prevents contamination of 6 nebulization set, mainly by fungal growth. If nebulization is given through a dirty and contaminated nebulization set, it may spread infection. A study done by Jadhav and co-authors concludes that nebulizer chambers need to be cleaned more frequently with disinfectants, to control the possible nosocomial fungal infections. The filter of nebulizer should be checked periodically for total discoloration. It should be changed when nebulization, as it may affect air exchanges in nebulizer machine [18-21]. Regular cleaning and disinfection of nebulization set and nebulizer maintenance are very important. Ideally, nebulization set should be cleaned and disinfected after every use. Most of the time device cleaning after every use may not be possible practically. Hence it is recommended that nebulization set must be cleaned and disinfected at least once daily at night. Nebulizer maintenance and cleaning should be done according to manufacturer’s advice [10]. After undergoing a detailed training session there was a remarkable improvement in the knowledge of paramedical staff about cleaning and disinfection practices.
In this present study, paramedical staff had very poor knowledge about the basic elements mentioned in the study showed significant improvement in post-training assessment. In the present study, we found that most of the nursing staff before this training program was not aware of good nebulization practices. Hence we stringy promote and encourage proper education about the care of nebulization set and nebulizer machines. Even after a detailed training program, we strongly feel the scope for improvement as 0.8% staff showed very poor performance and 73.1% staff answers were not in the best interest of nebulization techniques in post-training assessment respectively. Though number of staff giving an incorrect answer in post-training assessment may not be statistically significant, but they are solely responsible for patients’ safety and treatment. Hence we suggest that such programs should be repeated periodically to achieve and sustain improvement in proper nebulization practices.
Conclusion
Training of paramedical staff and demonstration of correct techniques had a very good outcome in improving the knowledge of the staff about nebulization techniques. This will have a positive impact on nursing practices and will improve the overall patient care. Every newly appointed staff requires training in nebulization techniques. Hence such activity should be continuous and ongoing in the form of periodic reassessment and training sessions.
References
- Raimondi AC, Schottlender J, Lombardi D, Molfino NA (1997) Treatment of acute severe asthma with inhaled albuterol delivered via jet nebulizer, metered dose inhaler with spacer, or dry powder. Chest 112: 24-28.
- Jindal SK, Aggarwal AN, Gupta D, Agarwal R, Kumar R, et al. (2012) Indian study on epidemiology of asthma, respiratory symptoms and chronic bronchitis in adults (INSEARCH). Int J Tuberc Lung Dis 16: 1270-1277.
- Gupta D, Agarwal R, Aggarwal AN, Maturu VN, Dhooria S, et al. (2013)Guidelines for diagnosis and management of chronic obstructive pulmonary disease: Joint ICS/NCCP (I) recommendations. Lung India 30: 228-267.
- Burney PG, Patel J, Newson R, Minelli C, Naghavi M (2015) Global and regional trends in COPD mortality, 1990–2010. Eur Respir J 45: 1239-1247.
- Salvi S, Agrawal A (2012) India needs a national COPD prevention and control programme. J Assoc Physicians India 60: S5-S7.
- Vincken W, Dekhuijzen R, Barnes P (2009) The ADMIT series-Issues in inhalation therapy. 4) How to choose inhaler devices for the treatment of COPD. Prim Care Respir J 19: 10-20.
- Cota S, Smith MS (2015) Delivery of nebulized medicines. United States patent US 9,180,262.
- Quon BS, Goss CH, Ramsey BW (2014) Inhaled antibiotics for lower airway infections. Ann Am Thorac Soc 11: 425-434.
- Jasper AC, Mohsenifar Z, Kahan S, Goldberg HS, Koerner SK (1987) Cost-benefit comparison of aerosol bronchodilator delivery methods in hospitalized patients. Chest 91: 614-618.
- Dolovich M, Dhand R (2011) Aerosol drug delivery: Developments in device design and clinical use. Lancet 377: 1032-1045.
- Bagcchi S (2015) India has low doctor to patient ratio, study finds. BMJ: British Medical Journal 30: h5159.
- Jevon P, Humphrey N (2007) Nursing times skills update-use of nebulisers. Nursing Times 103: 24.
- Newman SP, Steed KP, Reader SJ, Hooper G, Zierenberg B (1996) Efficient delivery to the lungs of flunisolide aerosol from a new portable hand-held multi dose nebulizer. J Pharm Sci 85: 960-964.
- British Thoracic Society and Scottish Intercollegiate Guidelines Network (2016) British Guideline on the Management of Asthma-A National Clinical Guideline.
- Boe J, Dennis JH, O'Driscoll BR, Bauer TT, Carone M, et al. (2001) European Respiratory Society Guidelines on the use of nebulizers. Eur Respir J 18: 228-242.
- Sign B (2011) British guideline on the management of asthma: a national clinical guideline. Scottish Intercollegiate Guidelines Network and The British Thoracic Society.
- Edwards L, Perrin K, Williams M, Weatherall M, Beasley R (2012) Randomised controlled crossover trial of the effect on PtCO2 of oxygen-driven versus air-driven nebulisers in severe chronic obstructive pulmonary disease. Emerg Med J 29: 894-898.
- Ghoshal AG, Salvi S, Dhar R, Guleria R, Mahashur A, et al. (2017) Consensus Document on Home Nebulization for Maintenance Treatment of Obstructive Airway Diseases: A Joint Initiative by the National Allergy Asthma Bronchitis Institute (NAABI) and Chest Research Foundation (CRF). J Assoc Physicians India 65: 60-73.
- Jadhav S, Sahasrabudhe T, Kalley V, Gandham N (2013) The microbial colonization profile of respiratory devices and the significance of the role of disinfection: A blinded study. J Clin Diagn Res 7: 1021-1026.
- Jordan S, White J (2001) Bronchodilators: Implications for nursing practice. Nurs Stand 15: 45-52.
- Gleeson JG, Green S, Price JF (1988) Air or oxygen as driving gas for nebulized salbutamol. Archives of disease in childhood 63: 900-904.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4557
- [From(publication date): 0-2018 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 3627
- PDF downloads: 930