Assessment of Drug Use Pattern by Using WHO Core Drug Use Indicators at Public Hospitals in Ethiopia
Received: 17-May-2017 / Accepted Date: 06-Oct-2017 / Published Date: 09-Oct-2017 DOI: 10.4172/2161-0711.1000559
Abstract
Background: Drug use is a complex subject involving the prescriber, the dispenser, the patient and pharmaceutical institutions. It is influenced by factors such as drug availability, prescriber’s experience, and knowledge of dispensers, health budget, cultural factors and many more. Inappropriate drug use is the problem of the whole world; however the degree of the problem is higher in developing countries like Ethiopia.
Objective: To assess drug use pattern by using who core drug use indicators at public hospitals in Gamo Gofa Zone, Southern Ethiopia September 2013.
Methods: Retrospective and prospective cross sectional study were used to collect data from prescriptions dispensed through the general outpatient pharmacies and Information for patients respectively. A pretested structured questionnaire was employed to collect information from prescription papers and respondents after obtaining a verbal consent. Data was entered, cleaned, edited and analysed using SPSS Version 16.0 statistical software package.
Results: The average number of drugs per prescription was 1.77 in Arba Minch General Hospital and 1.95 in Chencha District hospital ranging from 1-5. Percentage of encounter with antibiotics was 292 (48.67%) and 360 (60.20%) respectively. The Percentage of drugs prescribed by generic name and from an essential drug list was 100%. The mean consultation time spent between the prescriber and patient was 3.82 minutes and 3.66 minutes respectively and the mean pharmacy dispensing time was 1.18 minutes and 1.33 minutes respectively. More than half Patients had knowledge on drug dispensed to them 60.0% and 52.0% respectively and none of drugs dispensed were adequately labelled.
Conclusion: In our study the labelling status of prescribed medicines was very poor and needs special attention. Dispensing time is very short and it could have influenced patient’s knowledge on dispensed drugs. Furthermore designing strategies to improve availability of key essential drugs; establishing antimicrobial stewardship committee in both hospitals and improving drug and therapeutics committee by responsible bodies.
Keywords: Drug use; Prescribing indicator; Patient care indicators; Facility indicators, Gamo gofa
Abbreviations
ADR: Adverse Drug Reaction; DTC: Drug and therapeutics committee; EDL: Essential Drug List; EP: Emergency Pharmacy; FMHACA: Food Medicine and Health Care Administration and Control Authority; HAI: Health Action International; INRUD: International Network for the Rational Use of Drugs; IPP: In Patient Pharmacy; LIDE: List of Drugs for Ethiopia; OPD: Out Patient Department; RDU: Rational drug use; SNNPR: South Nations Nationalities and Peoples Region; USP: United States Pharmacopoeia; WHO: World Health Organization
Introduction
The International Network for the Rational Use of Drugs (INRUD) generated indicators in three main drugs use areas namely prescribing, patient care and drug systems [1,2]. Rational Use of Drug (RUD) requires that patients acquire medications appropriate to their clinical needs, in doses that meet their own requirements, for an adequate period of time, and at lowest cost to them and their community (WHO) conference at Nairobi 1985 [3].
Rational use of medication saves life and economy of health care costs. It limits undesired toxicity and adverse events and maximizes on the benefits that can be derived from optimal use of medications [4]. Misuse of drugs occurs in all countries mainly in developing countries and common types of irrational medicine use are: the use of too many medicines per patient (polypharmacy); inappropriate use of antimicrobials; inadequate dosage; over-use of injections when oral formulations would be more appropriate; failure to prescribe in accordance with clinical guidelines and inappropriate self-medication, often of prescription only medicines [5].
Over-use of antimicrobials is leading to increased antimicrobial resistance and it can stimulate inappropriate patient demand, and lead to reduced access and attendance rates due to medicine stock-outs and loss of patient confidence in the health system [6,7]. Worldwide more than 50% of all medicines are prescribed, dispensed, or sold inappropriately, while 50% of patients fail to take them correctly. Moreover, about one-third of the world’s population lacks access to essential medicines [8].
Essential medicines are not affordable to majority of the population in developing countries. This results in situations where a family ends up sharing medicines that were prescribed to treat one person [9]. According to surveys conducted by health action international (HAI) Africa and WHO in 11 Sub-Saharan Africa countries in 2004, the median availability of the essential medicines in public health facilities was below 70% [10].
Drugs are major components of pharmaceutical care. Hence, current expenditure on drugs rises up to 20% to 50% of total investment on health in developing countries [11-13]. Study conducted in Nepal showed that nearly 42% of the health budget is spent on drugs and international donors spend another three times, 80% of medicinal products are imported to Nepal however, the availability of drugs in the health posts and clinics are sporadic resulting into the prevalence of inappropriate drug use [14,15].
Study conducted in teaching hospitals of India showed that only one-fourth of the participants claimed that they always prescribed Essential Medicine; only 15.1% of the clinicians wrote the generic names of drugs on the prescription slip [9]. Another study carried out in India reported that 46.2% of the drugs were prescribed by generic name, but 45.6% of the prescribed drugs were irrational drug combinations. Only 45.7% of the prescribed drugs were according to the WHO model list of essential drugs.
Study conducted in Nigeria at a university teaching hospital showed that the prescription of several drugs per patients (poly pharmacy) is a serious problem with the average number of drugs per prescription is 2.8 (range 2.2-3.8) [16-18] and in other study conducted in Niger, almost 100% of the prescriptions in the name of essential and generic drug in the national drug list were [12].
Even though irrational drug uses are common in both developed and developing countries, the degree of the problem is higher in developing countries like Ethiopia where practices such as poly pharmacy, the use of wrong or ineffective drugs, under use or incorrect use of effective drugs and overuse of antimicrobials and injections are very common [19].
Currently there are few pocket studies are conducted on rational drug use in developing countries including Ethiopia [10]. However there is no similar study in Public Hospitals of Gamo Gofa Zone. There for this study was aimed to describe drug use pattern factors at public Hospitals in Gamo Gofa Zone and it would help to improve prescribing and dispensing practice drugs. It would also provide baseline information for researchers who are interested to conduct further studies to determine factors drug use pattern in these facilities.
Research Methodology
Study area and period
The study was conducted at the general outpatient of Arbaminch and Chencha hospital which are two hospitals among three hospitals found in Gamo Gofa zone, in SNNPR, from September 1 to 30, 2013. These hospitals provide outpatient, inpatient, emergency and other specialized services to a total population of about 3,741,304 (Gamo Gofa Zone) extrapolated from CSA 2007 data.
Arbaminch Hospital is located in Arbaminch Town which is 505 km to South of Addis Ababa. The hospital has 7 specialists, 15 General Practitioners, 13 Health Officers, 70 Nurses, 4 Pharmacists, 7 Druggists, 10 Laboratory Technologists, 10 Laboratory Technicians and 2 environmental health professionals.
Chencha Hospital is located in Chencha Town, which is about 547 km to South of Addis Ababa. The hospital has 4 General Practitioners, 7 Health Officers, 26 Nurses, 1 Pharmacists, 4 Druggists, 10 Laboratory Technologists, 4 Laboratory Technicians and 1 environmental health professional.
Source population: All patients who were visiting Arbaminch and Chencha Hospital during the study period were source populations.
Study population: All Patients visiting the general OPD with a prescription from the two hospitals during the study were enrolled in the study.
Study Design: Retrospective and prospective cross sectional study were used to collect data from prescriptions dispensed through the general outpatient pharmacies and Information for patients respectively.
Eligibility Criteria
Inclusion criteria
Patients 18 years and above, willing to participate, Prescriptions written in year 2013 and Legible and complete
Exclusion criteria
Patients below 18 years of age, Unwilling to participate and incomplete prescription
Sampling technique and sample size
The "minimum" recommended sample size for a prescription indicator is 600 encounters for study carried out in a single health facility [6]. For this study, prescriptions dispensed through the general outpatient pharmacy during 2013 were retrieved and arranged chronologically based on the date of dispensing. A total of 1198 prescriptions; 600 from Arba Minch General Hospital and 598 from Chencha District were drawn by systematic random sampling method. Data for patient care indicators were collected prospectively for randomly selected 100 outpatient encounters getting service in the outpatient pharmacy.
Variables
Dependent variable
Rational drug use based on WHO indicators
Independent variables
Socio-economic Variables: age, sex, educational status, marital status, religion, ethinicity occupational status, economic status
Prescribing indicators: Average number of drugs per encounter; Percentage of drugs prescribed by generic name; Percentage of encounters with an antibiotic prescribed; Percentage of encounters with an injection prescribed; Percentage of drugs prescribed from the essential drug list or formulary
Patient care indicators: Average consultation time; Average dispensing time; Percentage of drugs actually dispensed; Percentage of drugs adequately labelled; Patient’s knowledge of correct dosage;
Health facility indicators: Availability of copy of essential drug lists; Availability of copy of drug formulary; Availability of key drugs in the facility; Availability of Drug therapeutics committee and Availability Antimicrobial stewardship committee
Data collection tools
Standardized tool used by WHO/INRUD (International Network of Rational Use of Drugs) containing three major groups of indicators was adapted to consider current situation of the country and global agenda specially antimicrobial resistance, so we included two more indictors in facility indicators previously used;- these are Availability of drug and therapeutics committee and Availability of antimicrobial stewardship committee. Standardized tool in this contain the following three domains; 1) Prescribing indicators include: Average number of drugs per encounter; Percentage of drugs prescribed by generic name; Percentage of encounters with an antibiotic prescribed; Percentage of encounters with an injection prescribed; Percentage of drugs prescribed from the essential drug list or formulary; 2) Patient care indicators: Average consultation time; Average dispensing time; Percentage of drugs actually dispensed; Percentage of drugs adequately labelled; Patient’s knowledge of correct dosage;3) Health facility indicators: Availability of copy of essential drug lists; Availability of copy of drug formulary; Availability of key drugs in the facility; Availability of Drug therapeutics committee and Availability Antimicrobial stewardship committee.
Data on socio-demographic characteristics of patients were collected by semi-structured questionnaire by face-face interview. Labelling information and patient knowledge on dispensed drugs of the patients was collected after dispensing by observation and interview. The data were collected in five working days with about 20 patient encounters covered per day at peak working hours. Data on Availability of facility indicators was made interviewing and professionals working outpatient pharmacy and supported by observations by data collectors performed to ensure the availability of essential guidelines and key drugs in the stock. One day training for eight pharmacy technicians for data collection and two pharmacists were given by principal investigators on data collection tools and principles.
Data collection procedures and quality control
The questionnaire was Pre-tested on 10% of sampled patients to reduce bias related to measurement, misclassification. Questionnaire was reviewed by Data collectors and supervisors for completeness and for logical consistency, and counter checked by the principal investigator on daily basis and the collected data were appropriately coded, recorded, stored and processed.
Data analysis
Data were coded, checked for completeness and consistency. Then the data were entered and analyzed using SPSS for windows version 16.0 statistical software program. For descriptive statistics, results were expressed in terms of means and percentages and presented using tables and graphs according to the types of tool used. Values of the indicators obtained were compared with international standards, WHO, and results of other similar studies.
Ethical considerations
The study was ethically cleared by south nations and nationalities people’s regional health office ethical committee and permission was obtained from officials of both hospitals. Interview was carried out only with full consent of the patient/caregiver and parent being interviewed. Each respondent was assured that the information provided by him/ her would be confidential and used only for the purpose of research.
Operational definitions
Complete prescription: superscription (prescription which contains name of the patient, date of prescription, card number, sex and age); inscription (drug name, strength, route, frequency, duration of treatment) and subscription (Prescriber name, signature date; Dispenser initials, date, Signature) otherwise incomplete.
Dispensing time: is the time interval between the patients giving the prescription to dispenser and leaving the dispensary.
Drug Knowledge: respondents will be labelled to adequate drug knowledge if they are able to tell the correct dose, frequency of administration and length of therapy/duration, storage condition and precautions of prescribed medicine at exit interview unless poor.
Drug: means any substance or mixture of substances used in the diagnosis, treatment, mitigation or prevention of a disease in man or animal.
Generic drug: non-proprietary name of drugs and some commonly used brand names of known drug combinations such as Coartem, Terracortril, and Augmentin® were considered as generic names.
Labelling: is adequate if the label contains; the generic name of drug, Strength, dose, quantity dispensed, frequency of administration, direction for use, expiry date, name of the patient, name, storage conditions and special precautions.
Number of drugs per prescription: Known combination therapies like triple therapy for H.Pylori was not counted as 3 and diuretic, ACEI and spiranolactone for cardiac failure was not counted as 3 in recording the number of drugs per prescription and medical supplies like Gloves and syringes were not counted as drugs.
Prescription: means any order for drug written and signed by a duly licensed or authorized medical practitioner issued to a patient in order to collect drug from dispensing unit.
Results
Socio-demographic characteristics of Patients
A total of one hundred (100) patients from each hospital were participated in the study. Regarding socio-demographic characteristics Majority of participants from both hospitals were males 76 and 58 in Arba Minch General hospital and Chencha district hospital respectively. Majority of participants were Gamo by ethnicity and about one half of the participants were in age group of 25-34 years (Table 1).
| Socio-demographic characteristics | Arba Minch Hospital (n=100) | Chencha Hospital (n=100) | |||
|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | ||
| Sex | Male | 76 | 76 | 58 | 58 |
| Female | 24 | 24 | 42 | 42 | |
| Age | 15-24 | 3 | 3 | 5 | 5 |
| 25-34 | 52 | 52 | 48 | 48 | |
| 35-44 | 28 | 28 | 32 | 32 | |
| ³ 45 | 17 | 17 | 15 | 15 | |
| Religion | Orthodox | 52 | 52 | 42 | 42 |
| Muslim | 12 | 12 | 8 | 8 | |
| Protestant | 33 | 33 | 45 | 45 | |
| Catholic | 3 | 3 | 5 | 5 | |
| Ethnicity | Gamo | 45 | 45 | 86 | 86 |
| Gofa | 32 | 32 | 5 | 5 | |
| Wolayita | 13 | 13 | 7 | 7 | |
| Gurage | 8 | 8 | 2 | 2 | |
| Others | 2 | 2 | 0 | 0 | |
| Marital status | Single | 17 | 17 | 12 | 12 |
| Married | 70 | 70 | 82 | 82 | |
| Separated | 6 | 6 | 4 | 4 | |
| Divorced | 5 | 5 | 2 | 2 | |
| Widowed | 1 | 1 | 0 | 0 | |
| Residence | Urban | 64 | 64 | 32 | 32 |
| Rural | 36 | 36 | 68 | 68 | |
| Educational status | Illiterate | 36 | 36 | 46 | 46 |
| Completed primary school | 29 | 29 | 25 | 25 | |
| Completed secondary school | 15 | 15 | 16 | 16 | |
| Above secondary school | 18 | 18 | 13 | 13 | |
| Income | 1000-2500 birr | 17 | 17 | 37 | 37 |
| 2501-4500 birr | 30 | 30 | 42 | 42 | |
| 4501-6500 birr | 39 | 39 | 15 | 15 | |
| greater than 6500 birr | 14 | 14 | 6 | 6 | |
Table 1: Socio-demographic characteristics of outpatient attendants at public hospitals in Gamo Gofa Zone Southern Ethiopia September 2013(n=100).
Prescription indicators
A total of 1198, prescriptions were used for the evaluation of the prescribing pattern from two hospitals; 600 From Arba Minch General Hospital and 598 from Chencha District Hospital. From total prescriptions examined in Arba Minch hospital 269(44.83%) contained one drug per prescription, 224 (37.3%) contained two drugs per prescription and 84 (14.00%) contained three drugs per prescription. On the other hand from total prescriptions evaluated in Chencha Hospital 207 (34.62%) contained one drug per prescription, 268 (44.82%) contained two drugs per prescription and 79 (13.21%) contained three drugs per prescription. The average number of drugs per prescription was 1.77 in Arba Minch and 1.95 in Chencha Hospital ranging from 1 to 5 drugs per prescription. Regarding route of administration majority of patients in both hospitals were treated with orally followed by injections. Antibiotics were the most commonly prescribed drugs in both hospitals 292 (48.67%) and 360 (60.20%) respectively. All drugs are prescribed by their generic name from essential drug list of Ethiopia and only 484 (45.5%) of prescribed drugs in Arba Minch General hospital and 628 (53.9%) of prescribed drugs in Chencha hospital were actually dispensed to the patient (Table 2).
| Commonly prescribed antibiotics | Arba Minch General Hospital (n=600) | Chencha District Hospital (n=598) | ||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Number of drugs per prescription | ||||
| One | 269 | 44.83 | 207 | 34.62 |
| Two | 224 | 37.33 | 268 | 44.82 |
| Three | 84 | 14 | 79 | 13.21 |
| Four | 20 | 3.33 | 34 | 5.69 |
| Five | 3 | 0.5 | 10 | 1.67 |
| Route of administration | ||||
| Oral | 514 | 85.67 | 522 | 87.29 |
| Injection | 62 | 10.33 | 58 | 9.7 |
| Rectal | 18 | 3 | 13 | 2.17 |
| Vaginal | 6 | 1 | 5 | 0.84 |
| Commonly prescribed drugs | ||||
| Antibiotics | 292 | 48.67 | 360 | 60.2 |
| Cardiovascular dugs | 108 | 18 | 78 | 13.04 |
| Antidiabetics | 45 | 7.5 | 23 | 3.85 |
| Anti-protozoals | 102 | 17 | 94 | 15.72 |
| Anti-helmentics | 32 | 5.33 | 25 | 4.18 |
| GIT drugs | 21 | 3.5 | 18 | 3.01 |
Table 2: Prescription practice indicators at public hospitals in Gamo Gofa Zone Southern Ethiopia September 2013.
Commonly prescribed antibiotics
The most commonly prescribed Antibiotics in Arba Minch Hospital were Ciprofloxacillin 81(27.74%), Amoxicillin 75(25.68%) and Erythromycin 32(10.96%). While most commonly prescribed Antibiotics in Chencha Hospital were Ciprofloxacillin 118(32.78%), Doxycycline 80(22.22%) and Cotrimoxazole 26(7.22%) (Table 3).
| Commonly prescribed antibiotics | Arba Minch General Hospital (n=292) | Drugs | Chencha District Hospital (n=360) | ||
|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | ||
| Ciprofloxacillin | 81 | 27.74 | Ciprofloxacillin | 118 | 32.78 |
| Amoxacillin | 75 | 25.68 | Doxycycline | 80 | 22.22 |
| Erythromycin | 32 | 10.96 | Cotrimoxazole | 26 | 7.22 |
| Clarithromycin | 28 | 9.59 | Metronidazole | 25 | 6.94 |
| Cephalexin | 19 | 6.51 | Amoxacillin | 24 | 6.67 |
| Ampicillin | 16 | 5.48 | Clarithromycin | 23 | 6.39 |
| Cotrimoxazole | 12 | 4.11 | Ampicillin | 22 | 6.11 |
| Metronidazole | 11 | 3.77 | Cephalexin | 16 | 4.44 |
| Doxycycline | 10 | 3.42 | Cloxacillin | 14 | 3.89 |
| Cloxacillin | 8 | 2.74 | Erythromycin | 12 | 3.33 |
Table 3: Top ten antibiotics prescribed in outpatient departments at public hospitals in Gamo Gofa Zone Southern Ethiopia September 2013.
Commonly prescribed injections
Regarding the most commonly used injection medication, Diclofenac sodium is major one 39 (62.90%) followed by procaine penicillin 8 (12.90%) in Arba Minch General Hospital. While in Chencha District Hospital, Procaine Pencillin 39 (67.24%) followed by Diclofenac Sodium 7 (12.07) were commonly prescribed injection medications (Table 4).
| Commonly prescribed injections | Arba Minch General Hospital (n=62) | Drugs | Chencha District Hospital (n=58) | ||
|---|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | ||
| Diclofenac Sodium | 39 | 62.90 | Procaine penicillin | 39 | 67.24 |
| Procaine penicillin | 8 | 12.90 | Diclofenac Sodium | 7 | 12.07 |
| Cloxacillin | 7 | 11.29 | Cloxacillin | 6 | 10.34 |
| Cimetidine | 5 | 8.06 | Cimetidine | 5 | 6.90 |
| Tramadol | 3 | 4.84 | Tramadol | 5 | 3.45 |
Table 4: Commonly used injection medications prescribed at public hospitals in Gamo Gofa Zone Southern Ethiopia September 2013.
Patient care indicators
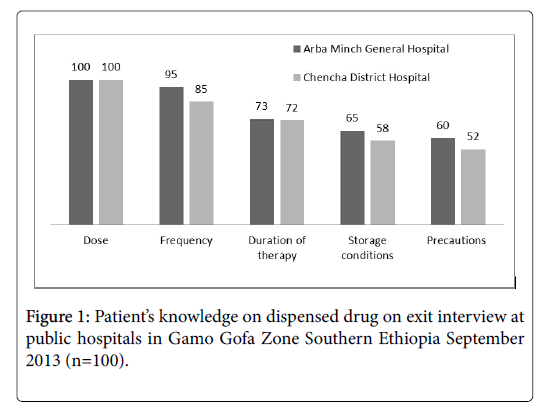
Data from patient exit interview showed that all most all patients knew the dosage of drugs dispensed to them, more than 80% of them knew frequency of administration and only 60% of patients from Arba Minch hospital and 52% of patients new special precautions regarding medicines prescribed for them. The overall knowledge on drugs dispensed was 60% in Arba Minch Hospital and 52% in Chencha Hospital (Figure 1).
Labelling information: Observation during exit about contents of label showed that all labels contain the generic name of drugs, below half of labels contain name of patient. While none of the labels contain information on frequency of administration, storage conditions, expiry date and special precautions. Overall labelling information was not adequate for all prescriptions dispensed to patients in both hospitals during study period (Table 5).
| Information available on label | Arba Minch General Hospital (n=100) | Chencha District Hospital (n=100) |
|---|---|---|
| Yes | Yes | |
| Patient name | 42 | 34 |
| Generic name | 100 | 100 |
| Strength | 28 | 23 |
| Dose | 17 | 12 |
| Quantity dispensed | 35 | 28 |
| Frequency of administration | 0 | 0 |
| Direction for use | 8 | 5 |
| Storage conditions | 0 | 0 |
| Expiry date | 0 | 0 |
| Special precautions | 0 | 0 |
Table 5: Distribution of Information found on Label of dispensed drug observed during exit interview at public hospitals in Gamo Gofa Zone Southern Ethiopia, September 2013.
Facility indicators: Out of 30 key essential drugs only 25 (83.33%) were available in Arba Minch General Hospital and 19 (63.33%) were available during study period. Both of the hospitals had a copy of essential drug list and drug formulary and drug and therapeutics committee which advises health professionals and patients on drug related issues. Both Hospitals had no antimicrobial stewardship committee (Tables 6 and 7).
| Essential Drugs | Strength | Availability | |
|---|---|---|---|
| Arba Minch | Chencha | ||
| Acetylsalicylic acid Tablet | 71 mg, 75 mg & 81 mg | √ | √ |
| Activated Charcoal Tablet | 125 mg, 250 mg | X | X |
| Adrenaline Injection | 0.1 mg/ml | √ | √ |
| Albendazole tab | 200 mg | √ | X |
| Aminophylline Injection | 250 mg /10 ml in 10 ml& 20 ml | √ | √ |
| Amoxacillin suspension/tab | 125 mg/5 ml; 250 mg, 500 mg | √ | √ |
| Atropine Sulfate Injection | 1 mg/ml in 1 ml ampoule | √ | √ |
| Arthemether + Lumefantrine tab | 120+ 20 mg | √ | √ |
| Cotrimoxazole tab/suspension | 240 mg/5 ml, 480 mg | √ | √ |
| Dextrose Injection | 5% in 1000 ml, 10% in 1000 ml | √ | X |
| Diclofenac Injection | 25 mg/ml in 3 ml ampoule | √ | X |
| Ergometrine Maleate Injection | 0.25 mg/ml, 0.5 mg/ml | X | X |
| Hydralazine Injection | 20 mg/ml in 1ampule | √ | √ |
| Chloroquine tab | 250 mg | √ | √ |
| Iodine + KI (Lugol’s solution) | 5%+ 10% | √ | X |
| Magnesium Sulfate Injection | 2%, 5%, 10%, 20%, 50% | √ | √ |
| Metoclopramide Drops/injection, tab | 0.2 mg/drop, 5 mg/ml, injection | √ | √ |
| Ferrous sulphate + Folic acid tab | - | √ | √ |
| Oral Rehydration Salt Powder | Sachet | √ | √ |
| Oxytocin Injection | 1 unit/ml, 5 unit/ml, 10 unit/ml | √ | √ |
| Prednisolone tab | 5 mg | √ | X |
| Promethazine Injection | 25 mg/ml | X | X |
| Propranolol Hydrochloride Injection | 1 mg/ml | X | X |
| Rabies Antiserum | 200 units in 5ml | √ | √ |
| Ringer’s Lactate solution | 1000 ml | √ | √ |
| Salbutamol Oral inhalation | 0.1 mg/dose; Nebulizer solution | √ | √ |
| Snake Venoum Antiserum Injection | 10 ml | √ | X |
| Sodium Chloride Injection | 0.9% in 1000 ml, 3% in 500 ml | √ | √ |
| TTC Eye drop/ointment | 0.5%, 1% | X | X |
| Vitamin K Injection | 10 mg/ml in 1ml ampoule | √ | √ |
Note: - “√”: Available and “x”: Not available
Table 6: Distribution of availability of key essential drugs at public hospitals in Gamo Gofa Zone Southern Ethiopia September 2013.
| WHO drug use indicators | Arba Minch Hospital | Chencha Hospital | |
|---|---|---|---|
| Prescribing indicators | Average number of drugs per encounter | 1.77 | 1.95 |
| Percentage of drugs prescribed by generic name | 1064 (100%) | 598 (100%) | |
| Percentageof injections prescribed | 62 (10.33%) | 58 (9.70%) | |
| Percentage ofantibiotics prescribed | 292 (48.67%) | 360 (60.20%) | |
| Percentage of drugs actually dispensed | 484 (45.5%) | 628 (53.9%) | |
| Percentage drugs prescribed from drug list | 1064 (100%) | 1166 (100%) | |
| Patient care indicators | Average consultation time in minutes | 3.82 (Min) | 3.66 (Min) |
| Average dispensing time in minutes | 1.18 (Min) | 1.33 (Min) | |
| Percentage of drugs actually dispensed | 484 (45.5%) | 628 (53.9%) | |
| Percentage of drugs adequately labelled | 0% | 0% | |
| Patient’s knowledge on prescribed drug | 60 (60.0%) | 52 (52.0%) | |
| Facility indicators | Availability of Essential drug list | 1 | 1 |
| Availability of Drug formulary | 1 | 1 | |
| Percentage of Availability of key drugs | 25 (83.33%) | 19 (63.33%) | |
| Availability Drug and therapeutics committee | 1 | 1 | |
| Availability of Antimicrobial stewardship committee | 0 | 0 | |
Note:- “1= Yes” and “0= No”
Table 7: Distribution of WHO drug use indicators at public hospitals in Gamo Gofa zone southern Ethiopia September 2013.
Discussion
This study revealed that the average number of drugs per prescription was 1.77 in Arba Minch General Hospital and 1.95 in Chencha Hospital. The slight increase in Chencha Hospital could be due to variation in prescribers experience because Arba Minch Hospital is General Hospital and there are experienced and physicians and other candidate prescribers. Generally the average number of drugs per prescription is similar to WHO recommendation on rational use of drugs (1.6-1.8) drugs per encounter [19] and Hawassa referral hospital 1.9 drugs per encounter [20].
In this study injection use was found to be 62 (10.3%) in Arba Minch Hospital and 58 (9.7%) in Chencha Hospital which is comparable to the WHO standard value i.e. 13.4-24.1% [19] and report from south West Ethiopia (11.07%) [21]. However it is lower than study done in Hawasa referral hospital 38.1% [20]. This variation could be explained by difference in distribution of disease pattern and level of care provided by professionals. The reduction of percentage of encounters with injections may have an advantageous in reducing the possibility of transmissions of blood born infections like HIV, and hepatitis [22].
The average percentage of patients receiving one or more antibiotics in the hospitals were 292 (48.67%) and 360 (60.20%) in Arba Minch and Chencha Hospital respectively. However this is higher than the WHO standard value 20.0-26.8. This could be explained by variation in geographical location, disease distribution being developing country infectious disease is more prevalent which necessitates Antibiotic prescription while WHO standard Value is average value.
This study also revealed that all drugs were prescribed by generic name in both hospitals. This is in line with WHO guideline which expects 100% of drug prescription to be generic. Increasing generic prescription could substantially reduce the cost of drugs for patients and the cost for facilities. Generally, generic prescription is an indicator of prescribing quality and the cost of prescribed medications can determine the level of compliance [23].
All drugs were prescribed from list of national essential drug list in this study. This is similar to study in Jimma University specialized Hospital, almost all drugs prescribed for the health problems were on the essential drug list of the country, but few drugs prescribed out of the list were found in the national drug list of Ethiopia [20].
The overall knowledge on drugs dispensed was 60% in Arba Minch Hospital and 52% in Chencha Hospital. Number factors could be a reason for this barrier such as educational background, cultural factors physical factors such as noises and etc. Moreover, the short dispensing time by itself could be a factor, because the clients have no enough time to get enough information about the drugs they have been dispensed [24].
In this study the average consultation and dispensing time in facilities was 3.82 minute and 3.66 minutes respectively. The probable reason for such smaller time could be the large number of patient flow for which the doctors and pharmacy professionals urged to cover, and the smaller number of manpower. The findings from this study were smaller than the study conducted in South West of Ethiopia 6.14 minute and 1.28 minute respectively [25].
In this study none of labels for the drugs dispensed were adequately labelled. According to WHO a label to be adequate it should contain at least patient name, drug name, strength, dosage (dose and frequency) and duration/quantity of the drug. However findings from similar studies showed that practice of adequate labelling was 67% [26-28]. It could be explained by high patient flow and inadequacy of knowledge and skill in labelling of prescribed drugs could be the major factor for these low results.
Percentage of drugs actually dispensed in this study was 484 (45.7%) and 628 (53.9%) respectively. This is lower than similar studies conducted in North West Ethiopia and in different other countries like Nigeria and Colombia. It could be directly related to inadequate availability of essential drugs. Studies showed that good drug and medical supply management insures continuous supply of drugs and prevents frequent stock outs and wastages [11,26-31].
Limitations of the Study
The findings of this study should be interpreted in light of its limitations. Being cross sectional and retrospective study there might be desirability and information bias; the study was limited in that it was not designed to reveal the factors determining rational drug use.
Conclusions and Recommendations
Conclusions
In our study there was no adequately labelled prescription; low average consultation and dispensing time. About one half of prescribed drugs were actually dispensed to the patients, which were an indicative of frequent stock outs and poor supply management in the facilities. Less than two third of patients had adequate knowledge on drugs dispensed to them. There was no antimicrobial stewardship committee in both hospitals. All drugs were prescribed by generic name from essential drug list and more three forth of key essential drugs were available in the General hospital and about two third of key essential drugs were available in the District hospital.
Recommendations
Based on the findings of this study the following recommendations were made; Zonal health department along with respective hospitals should design strategies to:-
• Improve labelling of prescribed drugs through providing training to pharmacy professionals about labelling and its importance
• Strengthen DTC function and establishing antimicrobial stewardship committee by motivation and empowering staffs to bear extra duties
• Improve availability of key essential drugs on stock through good drug supply management and training on drug supply management
• Improve patient knowledge on prescribed drugs through, improving patient counselling during dispensing
• Further study should also be done to dig out factors contributing irrational drug uses.
Acknowledgments
We would like to pass our heartfelt gratitude to research and publication core process of Arba Minch College of health sciences for valuable support in conducting this research work. Our deepest gratitude also goes to Pharmacy team for the Provision of the opportunity and providing necessary materials to conduct this research work.
We also like to acknowledge Gamo Gofa Zone health department for their provision of necessary information about demographic data of Hospitals and finally we are also thankful for the pharmacy stuffs of the respective hospitals for providing necessary information’s and valuable support during our work.
Competing Interests
There is no financial or personal relationship(s) which may have inappropriately influenced them in writing this article.
Authors’ Contributions
Mende Mensa, conceived the study, analysed the data and prepared the draft for publication and polished the language. Tarekegn Tadesse and Akililu Ayele participated in data analysis and approved the final manuscript.
References
- Kishore J (2006) National health programs of india: National policies & legislations related to health. New Delhi: Century Publications.
- Laing RO (1990) Rational drug use: An unsolved problem. Trop Doct 20: 101–103.
- Enwere OO, Falade CO, Salako BL (2007) Drug prescribing pattern at the medical outpatient clinic of a tertiary hospital in southwestern Nigeria. Pharmacoepidemiol Drug Saf 16: 1244-1249.
- World health organization (1985) The rational use of drugs. Report of a conference of experts Nairobi, 25-29 November 1985. Geneva.
- Alam K, Mishra P, Prabhu M, Shankar PR, Palaian S, et al. (2006) A study on rational drug prescribing and dispensing in outpatients in a tertiary care teaching hospital of Western Nepal. Kathmandu Univ Med J4: 436- 443.
- Otoom S, Batieha A, Hadidi H, Hasan M, Al- Saudi K (2002) Evaluation of drug use in Jordan using WHO prescribing indicators. East Mediterr Health J 8: 537-543.
- World health organization (1993) How to investigate drug use in health facilities: Selected drug use indicators. Geneva.
- Blum NL (2000) Drug information development. A case study Nepal. Rational Pharmaceutical Management Project. United States Pharmacopoeia.
- Essential Medicines and Health Products Information Portal (1993) How to investigate drug use in health facilities: Selected drug use indicators. EDM Research Series No.007. A World Health Organization resource.
- Action programme on Essential drugs and vaccines (1997) Managing drug supply. West Hartford, Connecticut, USA: Kumarian Press.
- Mallet HP, Njikam A, Scouflaire SM (2001) Evaluation of prescription practices and of the rational use of medicines in Niger. Sante 11: 185-193.
- Adebayo ET, Hussain NA (2010) Pattern of prescription drug use in Nigerian army hospitals. Annals of African Medicine 9: 152-158
- Kafle KK, Khanal DP (1995) Prescribing practices at private sectors in Nepal. J Inst Med 17: 147-148.
- Kafle K, Shrestha AD, Kkarkee SB, Prasad RR (2004) District drug use and health profile 2004 international network for rational use of drugs (inrud-nepal) gpo box # 8865.
- Odusanya OO, Oyediran MA (2000) Rational drug use in primary health care centers in Lagos, Nigeria. Nig J Hosp Med 10: 4-7.
- Chima IE (2012) Evaluation of drug use and patient care practices in a referral health facility in yenagoa, bayelsa state, Nigeria. Continental J Pharm Scie 6: 10-16.
- World Health Organization (2011) The world medicines situation 2011: Rational use of medicines. Geneva.
- Karande S, Sankhe P, Kulkarni M (2005) Patterns of prescription and drug dispensing. Indian J Pediatr 72: 117-121.
- Sharif SI, Al-Shaqra M, Hajjar H, Shamout A, Wess L (2008) Patterns of drug prescribing in a hospital in Dubai, United Arab Emirates. Libyan J Med 3: 10-12.
- Elmahalli AA (2012) WHO/INRUD drug prescribing indicators at primary health care centres in Eastern province, Saudi Arabia. Eastern Mediterranean health journal 18: 1091-1096.
- Anteneh AD (2013) Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: A cross-sectional study, BMC health service research 13: 170.
- Massele AY, Ofori-Adjei D, Laing RO (1993) A study of prescribing patterns with special reference to drug use indicators in Dar es Salaam region, Tanzania. Trop Doc 23: 104-107.
- Lamichhane DC, Giri B, Pathak O, Panta O, Shankar P (2006) Morbidity profile and prescribing patterns among outpatients in a teaching hospital in western Nepal. Mcgill J Med 9: 126-133.
- Akinyede AA, Mabadeje AFB, Aliu AA (2000) A comparative study of the patterns of prescription of antibiotics in two health centres in Lagos. J Nig Infect ContAssoc 3: 20-23.
- Federal Ministry of Health in collaboration with the WHO (2003) Essential drugs list, 4th revision. World Health Organization, Geneva.
- Mulugeta TA, Nasir TW, Raju NJ (2011) Assessment of patterns of drug use by using World Health Organization’s prescribing, patient care and health facility indicators in selected health facilities in Southwest Ethiopia. J applied pharma sciences 62-66.
- Acurcio FA, Perini E, Magalhaes SM, Terceiro LG, Vieira Filho JM, et al. (2004) Analysis of medical prescriptions dispensed at health centers in Belo Horizonte, Minas Gerais, Brazil. Cad SaudePublica 20: 72-79.
- Hogerzeil HV, Bimo, Ross-Degnan D, Lang RO, Ofori-Adjei D, et al. (1993) Field tests for rational drug use in twelve developing countries. Lancet 342: 1408-1410.
- Odusanya OO (2004) Drug use indicators at a secondary health care facility in Lagos, Nigeria. Nig J Comm Med Pri Health Care 16: 21-24.
- Guyon AB, Barman AA, Ahmed JU, Ahmed AU, AIam MS (1994) A baseline survey on use of drugs at the primary health care level in Bangladesh. Bjlettin of the world health organization 72: 265-271.
- Chareonku C, Khun LV, Boonshuyar C (2002) Rational drug use in Cambodia: Study of three pilot health centers in Kampong Thom Province. Southeast Asian J trop med Public health 33: 418-424.
Citation: Mensa M, Tadesse T, Ayele A (2017) Assessment of Drug Use Pattern by Using WHO Core Drug Use Indicators at Public Hospitals in Ethiopia. J Community Med Health Educ 7: 559. DOI: 10.4172/2161-0711.1000559
Copyright: © 2017 Mensa M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8138
- [From(publication date): 0-2017 - Nov 14, 2025]
- Breakdown by view type
- HTML page views: 6882
- PDF downloads: 1256