Case Report Open Access
Assessing Oxygenation Response to Eribulin in a Patient with Recurrent Breast Cancer after Resistance to Endocrine Therapy
Shigeto Ueda1, Toshiaki Saeki1*, Tomohiko Yamane2, Ichiei Kuji21Department of Breast Oncology, International Medical Center, Saitama Medical University, Hidaka, 350-1298, Japan
2Department of Nuclear Medicine, International Medical Center, Saitama Medical University, Hidaka, 350-1298, Japan
- *Corresponding Author:
- Toshiaki Saeki
Department of Breast Oncology
International Medical Center, Saitama Medical University, 1371-1 Yamane
Hidaka, 350-1298, Japan
Tel: +81-42-984-4670/8758
Fax: +81-42-984-4672
E-mail: syueda2000@yahoo.co.jp
Received Date: January 23, 2017; Accepted Date: January 25, 2017; Published Date: January 30, 2017
Citation: Ueda S, Saeki T, Yamane T, Kuji I (2017) Assessing Oxygenation Response to Eribulin in a Patient with Recurrent Breast Cancer after Resistance to Endocrine Therapy. OMICS J Radiol 6:250. doi: 10.4172/2167-7964.1000250
Copyright: © 2017 Ueda S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
We present our initial experience with a novel method of functional hypoxia imaging. 18F-fluoromisonidazole-positron emission tomography/computed tomography and diffuse optical spectroscopic imaging were used to noninvasively evaluate the biological effects induced by eribulin monotherapy in a patient treated for recurrent breast cancer with acquired resistance to endocrine therapy. Eribulin monotherapy clearly induced reoxygenation, indicated by the markedly reduced 18F-fluoromisonidazole uptake and enhanced oxygen saturation levels in the lesion. These observations suggest that the reversal of hypoxia can be captured utilizing 18F-fluoromisonidazole positron emission tomography/computed tomography and diffuse optical spectroscopic imaging.
Keywords
Eribulin; FMISO; Optical imaging; Hypoxia; Positron emission; Tomography
Introduction
Eribulin mesylate (eribulin) is a first-in-class halichondrin B-based inhibitor of microtubule dynamics. In a randomized phase III clinical trial (EMBRACE) in patients with metastatic disease, eribulin yielded significant improvements in overall survival when compared to physician-selected treatment [1]. Consequently, it was approved as a monotherapeutic agent for patients with metastatic breast cancer and a history of treatment with anthracycline and taxane chemotherapy. Recently, basic and clinical studies have revealed that eribulin induces vascular remodeling and subsequent tissue reoxygenation, thus stabilizing the cancer microenvironment and reversing the epithelial– mesenchymal transition associated with malignancy. These responses lead to the suppression of cancer invasion and metastasis [2-5].
Endocrine therapy is the mainstay of treatment for patients with Hormone Receptor (HR)-positive breast cancer. However, the long-term effectiveness of endocrine therapy is limited by the development of endocrine resistance, which is strongly associated with hypoxia in the tumor microenvironment [6]. A noninvasive technology for quantifying tumor hypoxia is 18F-fluoromisonidazole (FMISO) positron emission tomography/computed tomography (PET/CT) imaging [7]. Investigators have reported FMISO uptake as a robust measure of intracellular hypoxia, and reduced hypoxic activity after endocrine therapy has been identified as a good predictive marker of clinical response in patients with HR-positive metastatic breast cancer [8]. Tissue hypoxia can also be noninvasively measured using Diffuse Optical Spectroscopic Imaging (DOSI) with near-infrared light, which can enhance the characterization of vascularity and tissue oxygenation [9].
Here we present a case of a premenopausal woman with a recurrence of breast cancer in the Parasternal Lymph Node (PLN) after adjuvant endocrine therapy. Following eribulin monotherapy, we observed tissue reoxygenation in the recurrent PLN lesion via FMISO-PET/ CT and DOSI.
Case Presentation
A 38-year-old premenopausal woman underwent breast-conserving surgery with axillary dissection to treat left breast cancer at our hospital (SMU International Medical Center, Saitama, Japan). A postsurgical pathological examination revealed a 3.6-cm tumor with an invasive ductal carcinoma component. Immunohistochemistry revealed estrogen receptor (ER) positivity (Allred score: 8), progesterone receptor positivity (Allred score: 3), and HER2 negativity (1+), as well as nodal involvement (pN 2/18). She received standard-of-care adjuvant chemotherapy, including epirubicin and cyclophosphamide followed by docetaxel, and breast irradiation.
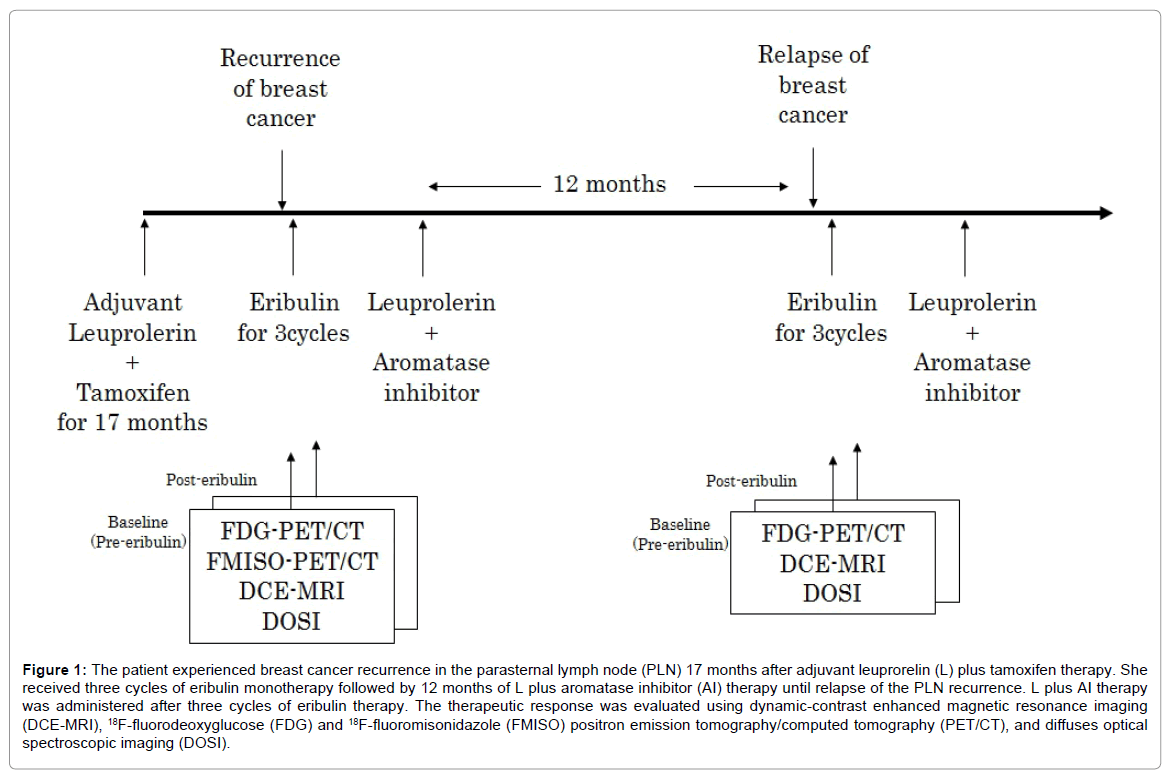
Seventeen months after finishing adjuvant chemotherapy and while receiving adjuvant leuprorelin (L) plus tamoxifen therapy, she complained of chest pain; recurrence of breast cancer in the PLN was subsequently diagnosed by fine-needle biopsy. Dynamic-contrast enhanced magnetic resonance imaging (DCE-MRI) and a baseline 18F-fluorodeoxyglucose (FDG)-PET/CT revealed PLN metastasis and plural breast cancer dissemination, as well as increased glycolytic activity [maximal standardized uptake value (SUVmax): 11.3]. The patient wished to continue endocrine therapy, which had a minimal risk of side effects and minimal financial burden. Therefore, we suggested three cycles of eribulin monotherapy (1.4 mg/m2, day 1; 8 per 21-day cycle), followed by additional endocrine therapy (Figure 1).
Figure 1: The patient experienced breast cancer recurrence in the parasternal lymph node (PLN) 17 months after adjuvant leuprorelin (L) plus tamoxifen therapy. She received three cycles of eribulin monotherapy followed by 12 months of L plus aromatase inhibitor (AI) therapy until relapse of the PLN recurrence. L plus AI therapy was administered after three cycles of eribulin therapy. The therapeutic response was evaluated using dynamic-contrast enhanced magnetic resonance imaging (DCE-MRI), 18F-fluorodeoxyglucose (FDG) and 18F-fluoromisonidazole (FMISO) positron emission tomography/computed tomography (PET/CT), and diffuses optical spectroscopic imaging (DOSI).
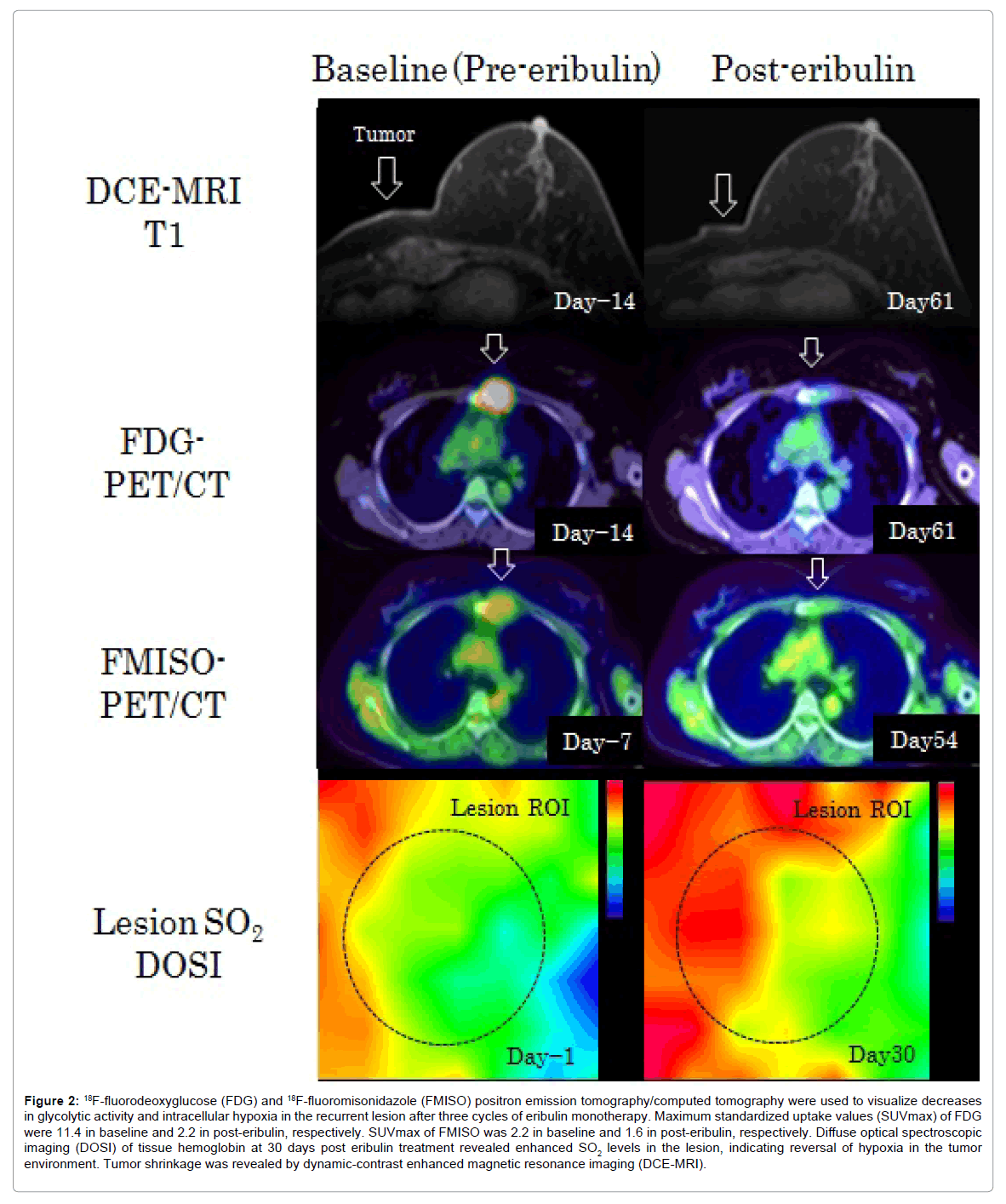
One week prior to the initiation of eribulin, she the patient participated in an Institutional Review Board (IRB)-approved FMISO-PET/ CT imaging study (UMIN06802). After providing informed consent, she was intravenously administered the FMISO tracer (7.4 MBq/kg), and simultaneous PET/CT scans were performed 120 min later. The pre-eribulin FMISO PET/CT scan demonstrated high hypoxic activity in the PLN lesion (SUVmax: 2.2). She also participated in an IRB-approved DOSI study (TRS20; Hamamatsu Photonics K.K., Hamamatsu, Japan) (UMIN15839), which indicated an average oxygen saturation (SO2) level of 66.4%. Details of the FMISO-PET/CT and DOSI procedures were described previously [10,11]. After three cycles of eribulin treatment, repeated FDG-PET/CT, FMISO-PET/CT, and DOSI scans indicated reduced SUVs and an increased SO2 level (Figure 2).
Figure 2: 18F-fluorodeoxyglucose (FDG) and 18F-fluoromisonidazole (FMISO) positron emission tomography/computed tomography were used to visualize decreases in glycolytic activity and intracellular hypoxia in the recurrent lesion after three cycles of eribulin monotherapy. Maximum standardized uptake values (SUVmax) of FDG were 11.4 in baseline and 2.2 in post-eribulin, respectively. SUVmax of FMISO was 2.2 in baseline and 1.6 in post-eribulin, respectively. Diffuse optical spectroscopic imaging (DOSI) of tissue hemoglobin at 30 days post eribulin treatment revealed enhanced SO2 levels in the lesion, indicating reversal of hypoxia in the tumor environment. Tumor shrinkage was revealed by dynamic-contrast enhanced magnetic resonance imaging (DCE-MRI).
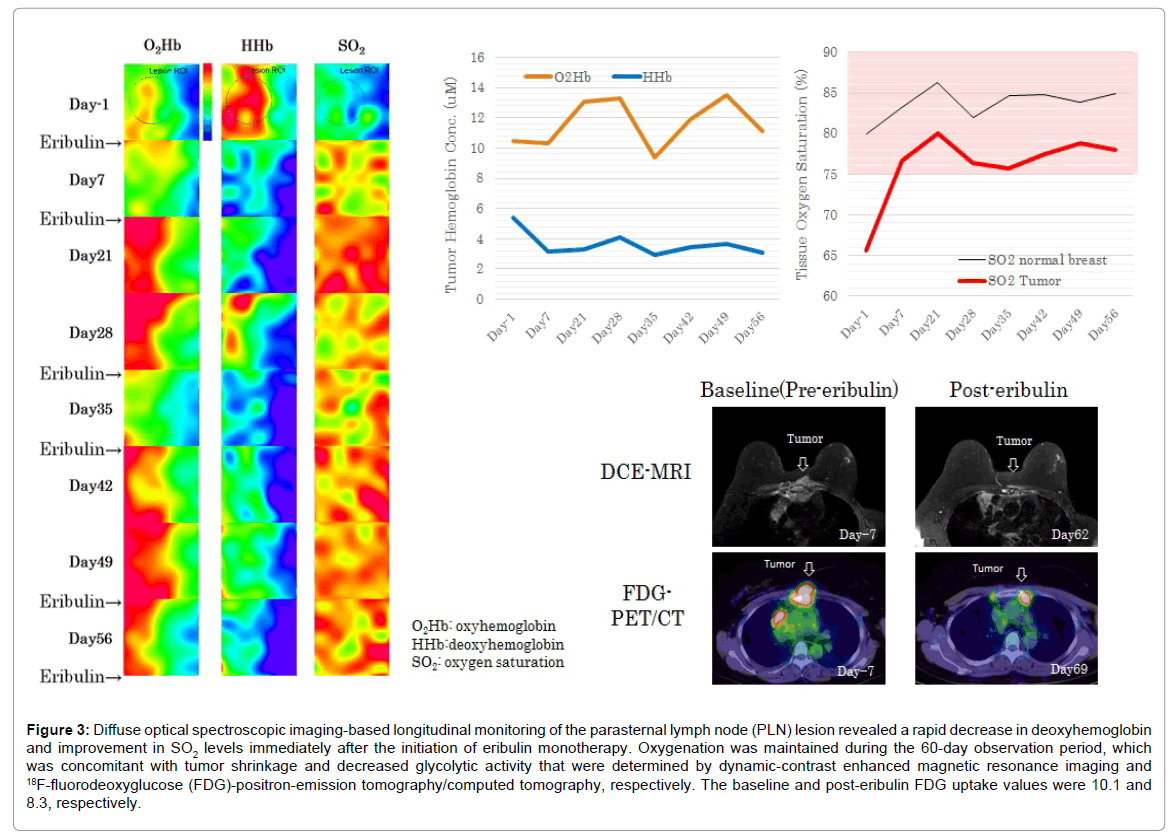
The unequivocal regression and re-oxygenation of the target lesion encouraged us to switch the patient’s endocrine therapy. She received further L therapy plus aromatase inhibitor (AI) (letrozole 2.5 mg; daily) for 12 months, until another relapse of pleural dissemination with PLN tumor growth was observed following complaints of chest pain and cough. At the time, the FDG-PET/CT scan yielded an SUVmax of 10.1 in the recurrent PLN lesion. The average SO2 level measured by DOSI was 65.1%. Because the patient wished to receive another course of eribulin monotherapy, we suggested that she be treated with eribulin for three cycles, with a subsequent endocrine therapy rechallenge. Tumor shrinkage and a decreased SUVmax were observed on DCE-MRI and FDG-PET/CT, respectively, after three cycles of eribulin treatment. DOSI monitoring of SO2 levels in the PLN lesion revealed enhanced tissue oxygenation immediately after initiating eribulin therapy, and this level was maintained during a 60-day observation period (Figure 3). The patient’s symptoms simultaneously disappeared with the observed effects. She has continued L plus AI (anastrozole, 1 mg; daily) therapy since concluding the three cycles of eribulin therapy, with no tumor regrowth or cancer-related symptoms.
Figure 3: Diffuse optical spectroscopic imaging-based longitudinal monitoring of the parasternal lymph node (PLN) lesion revealed a rapid decrease in deoxyhemoglobin and improvement in SO2 levels immediately after the initiation of eribulin monotherapy. Oxygenation was maintained during the 60-day observation period, which was concomitant with tumor shrinkage and decreased glycolytic activity that were determined by dynamic-contrast enhanced magnetic resonance imaging and 18F-fluorodeoxyglucose (FDG)-positron-emission tomography/computed tomography, respectively. The baseline and post-eribulin FDG uptake values were 10.1 and 8.3, respectively.
Discussion
Herein we highlight our initial experience with multiple functional modalities, including novel hypoxic imaging technologies based on FMISO-PET/CT and DOSI, which can noninvasively evaluate eribulin monotherapy-induced oxygenation in patients with metastatic breast cancer. In our case, eribulin led to tumor reoxygenation of the recurrent PLN lesion, characterized by markedly reduced FMISO uptake and enhanced tissue SO2 levels; these parameters reflected a stable oxyhemoglobin concentration and reduced deoxyhemoglobin concentration. Our observations suggest that the dynamic biological interplay between intracellular hypoxia and the tissue-hypoxic microenvironment within an eribulin-treated patient with recurrent breast cancer is captured utilizing FMISO-PET/CT and DOSI, respectively. The reduction in tumor glycolysis, as measured by FDG-PET/ CT, further suggested a reversal of hypoxia. In short, multiple functional imaging modalities revealed the transformation of an aggressive, hypoxic tumor to a weaker, oxygenized tumor.
Hypoxia, which strongly reduces ER expression and induces HIF1a upregulation, is strongly associated with acquired resistance to endocrine therapy [6]. Although DOSI is useful for monitoring blood oxygen levels in tissues, it is only applicable to surface lesions. FMISO-PET/ CT has been useful for quantitatively measuring hypoxic activity in reoxygenated metastatic lesions after chemotherapy. In a clinical study using FMISO-PET/CT for breast cancer patients treated with endocrine therapy, Cheng et al. [8]., reported a trend toward decreased hypoxic activity measured by tumor-to-background ratio of SUV 4 h (TBR4h) in clinical responders, whereas strong TBR4h activity was observed in nonresponders. The authors concluded that a high FMISO uptake level was associated with resistance to endocrine therapy [8].
Tissue SO2 levels are a sensitive indicator to changes in blood oxygen levels, which reflect the relative difference between oxyhemoglobin and deoxyhemoglobin and consequently, tissue oxygen consumption [12].
Repeated measurements of tissue SO2 levels enable the assessment of oxygenation responses immediately after treatment initiation [10]. In our patient, eribulin monotherapy remarkably reduced deoxyhemoglobin levels and consequently improved SO2 levels in the tumor, phenomena that are attributable to improved venous drainage and restored blood perfusion.
Conclusion
The premenopausal women have fewer endocrine therapy options and opportunities than menopausal women. We note that as tumor reoxygenation may be beneficial for restoring sensitivity to endocrine therapies, it would be reasonable to attempt an endocrine therapy rechallenge after treatment with vascular-remodeling agents such as eribulin. These findings could encourage us to conduct a clinical study with eribulin in breast cancer patient with endocrine therapy resistance.
Trial Registration
1. Clinical study for monitoring of therapy effect on breast cancer using 18F-fluoromisonidazole PET/CT (UMIN000006802).
2. Investigation of usefulness of molecular functional imaging to observe vascular remodeling and tumor oxygenation of breast cancer after start of eribulin mesylate (UMIN000015839).
Acknowledgement
The authors thank Noriko Wakui for assistance with optical measurements, and Yukio Ueda and Yutaka Yamashita for technical support regarding TRS20.
Funding Information
This research was supported by Eisai Co. Ltd. JSPS KAKEN grants 25830105 and 26282144, and JRFCP.
Disclosure Statement
Shigeto Ueda and Toshiaki Saeki received a research grant from Eisai Inc. None of the other authors have any conflicts of interest to declare.
References
- Cortes J, O'Shaughnessy J, Loesch D, Blum JL, Vahdat LT, et al. (2011) Eribulin monotherapy versus treatment of physician's choice in patients with metastatic breast cancer (EMBRACE): a phase 3 open-label randomised study. Lancet 377: 914-923.
- Funahashi Y, Okamoto K, Adachi Y, Semba T, Uesugi M, et al. (2014) Eribulin mesylate reduces tumor microenvironment abnormality by vascular remodeling in preclinical human breast cancer models. Cancer Sci 105: 1334-1342.
- Yoshida T, Ozawa Y, Kimura T, Sato Y, Kuznetsov G, et al. (2014) Eribulin mesilate suppresses experimental metastasis of breast cancer cells by reversing phenotype from epithelial-mesenchymal transition (EMT) to mesenchymal-epithelial transition (MET) states. Br J Cancer 110: 1497-1505.
- Dezso Z, Oestreicher J, Weaver A, Santiago S, Agoulnik S, et al. (2014) Gene expression profiling reveals epithelial mesenchymal transition (EMT) genes can selectively differentiate eribulin sensitive breast cancer cells. PLoSOne 9: e106131.
- Ueda S, Saeki T, Takeuchi H, Shigekawa T, Yaane T, et al. (2016) In vivo imaging of eribulin-induced reoxygenation in advanced breast cancer patients: a comparison to bevacizumab. Br J Cancer 114: 1212-1218.
- Kurebayashi J (2005) Resistance to endocrine therapy in breast cancer. Cancer Chemother Pharmacol 56: 39-46.
- Fleming IN, Manavaki R, Blower PJ, West C, Williams KJ, et al. (2015) Imaging tumour hypoxia with positron emission tomography. Br J Cancer 112: 238-250.
- Cheng J, Lei L, Xu J, Sun Y, Zhang Y, et al. (2013) 18F-fluoromisonidazole PET/CT: a potential tool for predicting primary endocrine therapy resistance in breast cancer. J Nucl Med 54: 333-340.
- Nakamiya N, Ueda S, Shigekawa T, Takeuchi H, Sano H, et al. (2014) Clinicopathological and prognostic impact of imaging of breast cancer angiogenesis and hypoxia using diffuse optical spectroscopy. Cancer Sci 105: 833-839.
- Ueda S, Kuji I, Shigekawa T, Takeuchi H, Sano H, et al. (2014) Optical imaging for monitoring tumor oxygenation response after initiation of single-agent bevacizumab followed by cytotoxic chemotherapy in breast cancer patients. PLoS One 9: e98715.
- Ueda S, Nakamiya N, Matsuura K, Shigekawa T, Sano H, et al. (2013) Optical imaging of tumor vascularity associated with proliferation and glucose metabolism in early breast cancer: clinical application of total hemoglobin measurements in the breast. BMC Cancer 13: 514.
- Tromberg BJ, Cerussi AE (2010) Imaging breast cancer chemotherapy response with light. Clin Cancer Res 16: 2486-2488.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 3556
- [From(publication date):
February-2017 - Jul 13, 2025] - Breakdown by view type
- HTML page views : 2674
- PDF downloads : 882