Case Report Open Access
Aspergillosis of Gastrointestinal Tract Mimicking Malignancy: A Case Report
Mishra P*, Gupta Divya, Mishra S and Srinivas V
Department of Pathology, Tata Memorial Centre, Parel, Mumbai, 400012, India
- *Corresponding Author:
- Mishra P
Department of Pathology
Tata Memorial Centre Parel
Mumbai, 400012, India
E-mail: psmofi2@gmail.com
Received date: May 27, 2017; Accepted date: June 20, 2017; Published date: June 26, 2017
Citation: Mishra P, Gupts G, Mishra S, Srinivas V (2017) Aspergillosis of Gastrointestinal Tract Mimicking Malignancy: A Case Report. J Clin Exp Pathol 7:311. doi:10.4172/2161-0681.1000311
Copyright: © 2017 Mishra P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
A variety of infectious diseases can have clinical, radiological and histopathological findings that mimic various malignancies. We report a case of a 53 year old immunocompetent man admitted initially as a case of perforation peritonitis with strong clinical suspicion of a gastric malignancy. Histologically, the biopsy from the stomach perforation site showed necrotic gastric wall with scattered atypical cells in muscularis. Initially suspected to be neoplastic, these cells could not be characterized definitively by an immunohistochemistry panel. However, special stains for fungi done on account of necrosis, demonstrated presence of numerous fungal hyphae of Aspergillus in the gastric ulcer slough. Systemic antifungal treatment was instituted after which the patient showed significant clinical improvement and was discharged from the hospital following an uneventful recovery. To the best of the author’s knowledge, this is the first report of a case of Aspergillus infection mimicking gastric malignancy in a non-immunocompromised individual from India.
Keywords
Suspected malignancy; Atypical cells; Immunohistochemistry; Special stains; Aspergillosis
Introduction
Medical literature is replete with reports of cases where infectious diseases are seen to mimic malignancy especially in an immunocompromised individual. Most commonly affected are the pulmonary, soft tissues, haematolymphoid and gastro-intestinal systems and a mass lesion is the usual mode of presentation. Inspite of advances in imaging studies, serologic/microbiologic testing and histopathology techniques, an accurate diagnosis remains challenging in many cases [1,2]. The diversity of causative agents, including bacteria, mycobacteria, fungi and viruses adds to the overall difficulty in diagnosis of these cases. Fungal infections account for a sizable proportion of these cases causing substantial mortality and morbidity in the developing countries, though data in this regard are scarce at best. Importantly, in a proportion of these cases, this is both preventable and curable [1-4].
Fungal infections are common accompaniments or complications seen during or after the course of therapy for various gastrointestinal tract (GIT) malignancies. Rarely, disseminated fungal infections in an immunocompromised individual can mimic as a malignancy of the GIT. However, such cases in an immunocompetant person are very rarely reported in the literature [4-6]. Common opportunistic fungi associated in such cases are mucor, pneumocystis or basidiomycoses. A handful of cases of aspergillosis, seen to mimic carcinoma of the GIT, have been reported in the literature [4,5,7-9]. However, no such case report or study has emanated from the Indian sub-continent where Aspergillus is a common mould accounting for 0.1%–22% of all fungal spores in hospital air samples.
Here, we report a case of multiple gastric and intestinal perforations with features of peritonitis in an immunocompetant adult man strongly suspected to have a primary GIT malignancy by the clinicians. He was finally diagnosed as a case of Aspergillus infection on histopathologic evaluation of biopsy tissue from the gastric perforation site. This is possibly the first report of a gastric aspergillosis mimicking malignancy in an immunocompetant individual from India. This case also emphasizes that a timely and accurate diagnosis of infections mimicking malignancies can save lives and avoids unnecessary vagaries of diagnostic and therapeutic procedures and their complications for the patient.
Case Report
A fifty-three year old male with no known co-morbidities and a past history of medically treated duodenal ulceration, was admitted to our hospital with acute onset pain abdomen and black discoloration of his stools for 15 days duration. For the last three days, he reported an exacerbation of his symptoms. His nutritional status was satisfactory. Local examination revealed a distended tender abdomen. Local guarding was elicitable and bowel sounds were sluggish. An erect X-ray abdomen followed by an ultra sonogram (USG) of the abdomen revealed excessive bowel gas in the abdominal cavity with multiple air-fluid levels signifying intestinal perforation.
The patient underwent emergency exploratory laparotomy along with peritoneal lavage. Graham’s patch repair of a gastric and ileal perforation was done along with draining gastrostomy, feeding jejunostomy and T-tube drainage. The per-operative laparotomy findings included presence of 800 ml of bilious yellow fluid in the peritoneal cavity, one 1.5 cm pre-pyloric gastric ulcer on the anterior wall close to the lesser curvature and another 2.5 cm large longitudinally oblique post pyloric ulcer involving D1 with active bile leak. A small proximal ileal perforation was also noted. The caecum, appendix and the large bowel were normal. The tissue from the gastric ulcer was sent for histopathological evaluation.
The general condition of the patient deteriorated during the course of his admission, the patient was put on ventilator and on respiratory examination revealed presence of decreased breath sounds on the left side of his chest. An emergency re-exploration with repair of a leak with falciform ligament patch at the site of the gastric perforation was done. Another small linear defect measuring 0.5 cm was seen on the pylorus parallel to the previously repaired gastric defect and was similarly repaired.
Histopathologic Examination
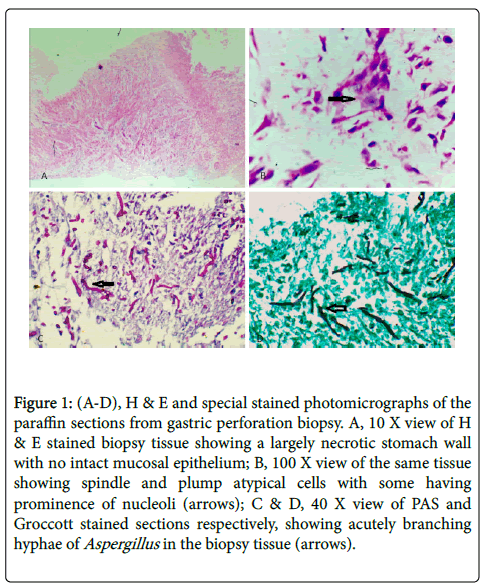
On gross examination, the biopsy comprised of fragmented, fragile, necrotic grayish-pink tissue which was fully submitted for further processing. The routine hematoxylin and eosin (H & E) stained sections examined from the tissue showed necrotic gastric tissue with few scattered atypical cells seen in the remnant muscular layer of the stomach. These cells were spindled to plump with large hyperchromatic nuclei having prominent nucleoli and were haphazardly scattered across the width of the muscularis (Figure 1). Mucosal epithelium was not seen and no apparent distinction was possible between mucosal or serosal aspects of the tissue due to extensive necrosis and inflammation. No bacterial colonies, fungi or other organisms could be seen on microscopy. No granulomas were detected either. In view of the atypical appearing cells and a clinical suspicion of malignancy as offered by the treating clinicians, an obvious differential diagnosis of a malignancy or an infective process was offered. Special stain results which were available the next day showed broad based, acutely branching, fungal hyphae on Groccott’s and periodic acid-Schiff (PAS) staining. Following the report, a systemic antifungal treatment was instituted. Meanwhile, even after extensive immunohistochemical (IHC) evaluation inclusive of AE1/ AE3, S100, SMA, vimentin, desmin, LCA, CD34, CD99 & MIB1 (Ki67), no final characterization could be attributed to the ‘atypical’ cells. The same could not be pursued further due to tissue depletion.
Figure 1: (A-D), H & E and special stained photomicrographs of the paraffin sections from gastric perforation biopsy. A, 10 X view of H & E stained biopsy tissue showing a largely necrotic stomach wall with no intact mucosal epithelium; B, 100 X view of the same tissue showing spindle and plump atypical cells with some having prominence of nucleoli (arrows); C & D, 40 X view of PAS and Groccott stained sections respectively, showing acutely branching hyphae of Aspergillus in the biopsy tissue (arrows).
Based on the above findings, a final diagnosis of disseminated Aspergillus infection with involvement of stomach was rendered. Systemic antifungal treatment with injection. Liposomal Amphotericin B (150 mg intravenous three times a day for 6 days) was instituted to which the patient responded very well and showed features of significant recovery. At the time of this writing the patient had been discharged from the hospital and was on a close follow up.
Discussion
Differentiating infective conditions from malignant neoplasms, in some instances, may be very challenging for the clinician, and a radio-pathological correlation is often warranted. Problem arises when both the radiologist and the pathologist also find it difficult to distinguish between the two. A rare example is a systemic fungal infection masquerading as a malignancy, and posing a huge diagnostic dilemma for the clinicians, radiologists and the pathologists alike [1,3,5,6]. Our case is a classical example of a combination of all these factors, the patient presented with ambiguous symptoms and signs with radiologic findings of GIT perforation; he had no underlying or predisposing medical conditions and a malignancy could not be excluded in this context even after initial histopathologic examination.
In terms of mortality and morbidity, systemic fungal infections are second only to tuberculosis in India and are unusually seen to afflict immunocompetant individuals also [1,3]. The index case too is an immunocompetant individual with no significant past or family history of serious illness. His nutritional status was also satisfactory at the time of presentation. A high index of suspicion for malignancy is imperative in such cases, though the possibility of disseminated infections is always an important consideration in this part of the globe [4-6].
Cases of pulmonary fungal infections mimicking malignancy are not uncommon. In a study by Rolston et al. including nearly 3000 cases of suspected malignancies, fungal infections were seen to mimic malignancy in approximately 46% of diagnosed infections, accounting for about one-fourth of all cases [2]. The clinical manifestations and radiographic findings of such infections are indistinguishable from those produced by pulmonary neoplasms [3]. Likewise, these fungal organisms are a potential mimic of numerous other non-pulmonary neoplastic conditions.
Diversity of clinical features and overlapping clinico-radiological findings in this case were indications for a histopathological examination to rule out the possibility of a lurking abdominal malignancy [5]. Though, no radiologic features of a mass lesion was identified in this case, this was in part attributable to the acute nature of his presentation due to which early intervention and a diagnostic biopsy were more imperative than further search for a possible visceral malignancy. The role of a pathologist is vital in this regard as the final diagnosis may often guide the further course of treatment and outcome for the patient. The criticality of a high index of suspicion and meticulous follow up to rule out a differential diagnosis of malignancy cannot be overemphasized owing to vastly different outcomes in the two scenarios [6].
Histopathology remains the gold standard for tissue diagnosis of most infective and neoplastic diseases. However, it is important to realize the limitations of the pathologists. Sensitivity and specificity of a histopathologic report improves significantly in ambiguous cases, like the index case, if other inputs are also available to the pathologist. Apart from histopathological examination, appropriate samples should also be sent, where relevant, for serologic and microbiologic investigations to aid the final diagnosis [1,2,4]. Albeit, a lavage sample sent for culture, in this case, was negative for any bacterial or fungal organisms and thus non-contributory in our case.
Extensive necrosis in biopsy tissue can make a pathologist’s task even more difficult as was amply evident in this case. The cause of infection and the blood supply to the involved organ are important factors deciding the extent and speed of necrosis [1,7,8]. In this case, transmural necrosis was seen at the site of gastric perforation. That necrosis attracts inflammation is a common knowledge, and the resultant tissue response is often rich in vasculature comprising of proliferating endothelial cells and inflammatory cells [7]. In this case, the atypical cells which were initially suspected to be malignant may possibly be ascribed to the endothelial cells or macrophages seen as part of this inflammatory process. This also explains why a panel of IHC antibodies, as described above, could not help in characterizing the ‘atypical cells’.
Of all the fungal infections mimicking malignancy, Aspergillus has been studied in the maximum detail [1-6]. On tissue sections, as seen in this case, the Aspergillus hyphae characteristically appear as uniform, narrow (3-6 micrometer in width), tubular and regularly septate (usually 45°C) filaments (Figure 1). Special stains for fungi, like PAS and Gomori Methamine Silver (GMS) or Groccott are superior to H & E for the characterization of hyphal morphology and the Aspergillus hyphae were seen to be highlighted by these special stains in this case (Figure 1A-D).
Fungal infections are very rarely seen, as in this case, to mimic GIT malignancies and they need to be differentiated for a swift and specific treatment for patients [9]. Though, mortality in disseminated fungal infections has been reported even in immunocompetant cases treated at best of the centers, it remains significantly lower compared to visceral malignancies [10]. At the same time, it is critically important to avoid unnecessary high risk procedures, toxic chemotherapy, radiotherapy and expensive targeted therapies required for the treatment of cases of malignancy.
Conclusion
To conclude, the authors report the first case from India of a suspected malignancy in a patient having disseminated aspergillosis and presenting with multiple GIT perforations with features of peritonitis. The non-specific radiological and clinical findings in such a case can lead to a misdiagnosis of malignancy and an accurate diagnosis may be elusive even on histopathologic evaluation. Distinguishing these infectious lesions from malignancies remains one of the important diagnostic challenges for the pathologist. A high index of suspicion helps in diagnosing the condition accurately. Precise diagnosis is crucial for a prompt and appropriate treatment and to avoid unnecessary high-risk surgical procedures/adjuvant therapy needed for malignancy.
and presenting with multiple GIT perforations with features of peritonitis. The non-specific radiological and clinical findings in such a case can lead to a misdiagnosis of malignancy and an accurate diagnosis may be elusive even on histopathologic evaluation. Distinguishing these infectious lesions from malignancies remains one of the important diagnostic challenges for the pathologist. A high index of suspicion helps in diagnosing the condition accurately. Precise diagnosis is crucial for a prompt and appropriate treatment and to avoid unnecessary high-risk surgical procedures/adjuvant therapy needed for malignancy.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Madhusudhan KS, Gamanagatti S, Seith A, Hari S (2007) Pulmonary infections mimicking cancer: report of four cases. Singapore Med J 48: 327–31.
- Rolston KV, Rodriguez S, Dholakia N, Whimbey E, Raad I (1997) Pulmonary infections mimicking cancer: a retrospective, three-year review. Support Care Cancer 5: 90–93.
- Schweigert M, Dubecz A, Beron M, Ofner D, Stein HJ (2013) Pulmonary infections imitating lung cancer: clinical presentation and therapeutical approach. Ir J Med Sci 182: 73–80.
- Eggimann P, Chevrolet JC, Starobinski M, Majno P, Totsch M, et al. (2006) Primary invasive aspergillosis of the digestive tract: report of two cases and review of the literature. Infection 34: 333–338.
- Stevens DA, Melikian G (2011) Aspergillosis in the ‘Nonimmunocompromised’ Host. Immunol Invest 40: 751-766.
- Pfeiffer RB, Hashimoto LA, Subramony C, Chen F (2003) Pseudomembranous gastritis: a complication from Aspergillus infection. Am Surg 69: 536–538.
- Trésallet C, Seman M, Hoang C, Meneqaux F (2010) Gastric perforation from potential primary digestive aspergillosis. Surgery 148: 158–159.
- Franciosi CM, Romano F, Caprotti R, Uggery F (2002) Multiple gastric perforations in an immunodepressed child. Surgery 131: 685–686.
- Gefter WB (1992) The spectrum of pulmonary aspergillosis. J Thorac Imaging 7: 56–74.
- Dalal Nemenqani, Nausheen Yaqoob, Hatem Khoja, Osama Al Saif, Nasir K Amra, et al. (2009) Gastrointestinal basidiobolomycosis: An unusual fungal infection mimicking colon cancer. Archives of Pathology & Laboratory Medicine 133: 1938-1942.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 3289
- [From(publication date):
June-2017 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 2476
- PDF downloads : 813