Case Report Open Access
Arteriovenous Malformation of the Oral Cavity: A Case Report
Stephanie Tan* and Phillip MarshRoyal Brisbane and Womens Hospital, Australia
- *Corresponding Author:
- Stephanie Tan
B. Pharm, MBBS
Royal Brisbane and Womens Hospital
Brisbane, Queensland, Australia
Tel: +61-438817733
E-mail: stephtan88@gmail.com
Received Date: January 14, 2015; Accepted Date: March 10, 2015; Published Date: March 17, 2015
Citation: Stephanie Tan, Phillip Marsh (2015) Arteriovenous Malformation of the Oral Cavity: A Case Report. J Oral Hyg Health 3:174. doi: 10.4172/2332-0702.1000174
Copyright: © 2015 Tan and Marsh. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Arteriovenous malformations (AVMs) are part of a group of vascular anomalies which can be further sub classified into neoplasms and malformations, characterized by specific morphology, pathophysiology, clinical behaviour and management. AVMs in the oral and maxillofacial region are rare but potentially life-threatening vascular lesions. Bleeding, facial asymmetry, loose teeth and headache are commonly seen at presentation.
Management of maxillofacial AVMs remains challenging, as total excision is required to ensure complete cure and to prevent recurrence, as the remnant AVM has the potential to grow quickly and exceed pre treatment size. Surgical excision however, carries the risk of massive life threatening intraoperative bleeding due to replacement of normal tissue with disease vessels. This case describes a 76 year old female who presented with a bleeding AVM involving the left buccal mucosa who underwent surgical excision.
Keywords
Arteriovenous malformation; Vascular malformation; Vascular lesion; Vascular tumour; Oral cavity; AVM (Arteriovenous malformations); Vascular anomalies
Introduction
Arteriovenous malformations (AVMs) are developmental anomalies that occur when the embryonic vascular network fails to differentiate. The prevalence of vacsular malformations is approximately 1% of births, however the majority of these do not seek treatment. While AVMs are usually present at birth, they commonly manifest in childhood or adolescence, and can occur at any area of the body [1,2]. The most common site of presentation in the oral cavity includes the anterior two thirds of tongue, palate, and gingival and buccal mucosa, however any site may be affected [3].
Although AVMs can be asymptomatic or cause local functional disturbance, complications include severe haemorrhage which can result in significant morbidity and mortality. Diagnosis of these lesions is essential to determine treatment, and includes plain radiography, computed tomography (CT) scans, magnetic resonance imaging (MRI), doppler ultrasound or angiography. Current literature still supports surgical treatment, combined with embolization and some sclerosing agents. This case describes a 76 year old female who presented with a bleeding AVM involving the left buccal mucosa who underwent surgical excision.
Case Report
A 76 year old female was referred privately to an oral & maxillofacial surgeon by her GP for investigation of a rapidly enlarging left buccal lesion. The lesion started as an ulcer three months prior and continued to grow and bleed profusely at times, causing difficulty eating solid foods. There was no history of trauma. Past medical history included: hypertension, high cholesterol, diverticulitis and osteoarthritis. Current medications included: Candesartan 16/8mg, atorvastatin 10mg and aspirin 100mg. Spontaneous bleeding had increased up to 6-7 times daily, with overnight hospitalisation recently required for control, and she was advised to cease aspirin until further review.
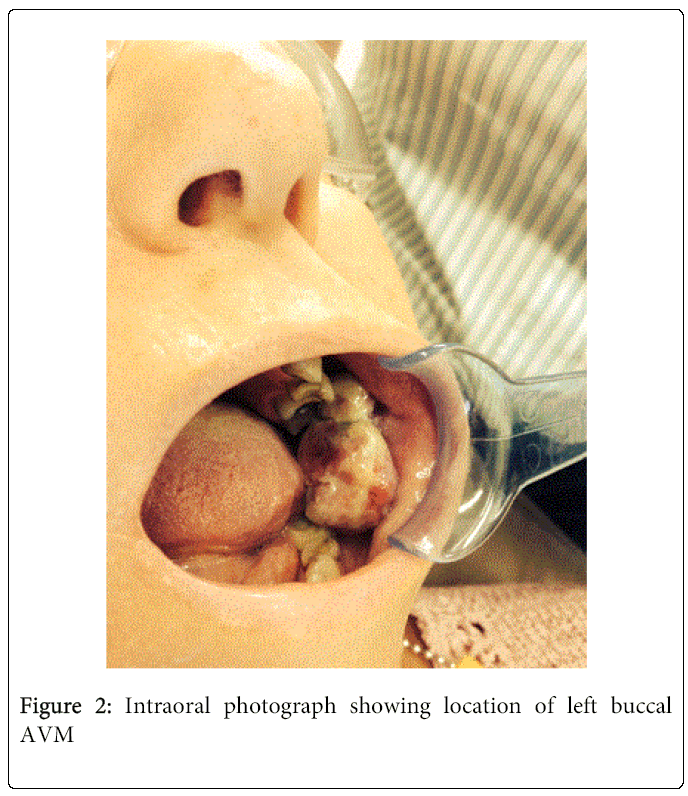
On examination, a 6x6 cm, ulcerated pedunculated mass on the left buccal mucosa on a 1 cm pedicle was noted, with a palpable pulse and bruit on its base. On palpation, it had a soft consistency and was easily compressible. There was minimal extraoral and soft tissue swelling, with no obvious asymmetry. There was no lymphadenopathy and the remainder of the examination was unremarkable. A small biopsy of the left buccal mucosal lesion was reported as an ulcerated benign haemangioma involving apparent deep margins. A single vicryl suture maintained haemostasis. No bleeding complications arose.
A CT angiogram (Figure 1) was subsequently performed, which reported a high flow AVM feeding from the transverse facial and facial arteries.
The patient was referred to the Royal Brisbane and Women’s Hospital, where she underwent surgical excision of the left buccal AVM. Bleeding was locally controlled with suction and diathermy, without the need for blood transfusion, sclerosing agents or pre-operative embolisation. The AVM was clamped and ligated and transfixed with 3-0 vicryl sutures. The patient remained in hospital for 2 days post operation with nil further bleeding and recovered uneventfully. Histopathological diagnosis confirmed an AVM (Figure 2).
At one week review the wound was healing well with no signs of residual AVM or bleeding. On 6 monthly review she continued to be well, and was planned for yearly follow up until further notice.
Discussion
Classification of vascular anomalies has since evolved from early classifications by Virchow and Wagner, which characterised vascular lesions according to the vessel’s pathological appearance. Lesions were divided into angiomas and lymphangiomas, without consideration of their biological behaviour. Mulliken and Glowacki [4,5] extended the classification of vascular birthmarks into two major classifications: hemangiomas and malformations. These were differentiated by clinical appearance, histopathological features and biological behaviour. Several modifications have now been made. Due to ongoing confusion, inaccurate diagnoses and potential mismanagement from older nomenclature, the currently accepted classification by the International Society for the study of Vascular Anomalies (ISSVA) divides vascular lesions into neoplasms (vascular and vasoproliferative) (Table 1) and malformations [6,7]. The major distinction between the 2 categories is whether there is increased endothelial cell turnover, as seen with vasoproliferative neoplasms, whereas vascular malformations are structural abnormalities [7].
| Vascular (Vasoproliferative) Neoplasm | Vascular Malformations |
|---|---|
| Infantile hemangioma | Slow flow vascular malformations |
| Congenital hemangioma | Capillary malformations |
| RICH | Venous malformations |
| NICH | Lymphatic malformations |
| Kaposiform Hemangioendothelioma and tufted angiomas (with or without Kasabach-Merritt syndrome) | Fast flow vascular malformations |
| Spindle cell Hemangioendothelioma | Arterial malformations |
| Epitheloid Hemangioendothelioma | Arteriovenous malformations |
| Other rare Hemangioendotheliomas (i.e, composite, retiform, and others) | Arteriovenous fistula |
| Angiosarcoma | Combined vascular Malformations (various combination of the above) |
| Dermatologic acquired vascular tumors (i.e, pyogenic granuloma) | |
| RICH, rapidly involuting congenital hemangioma; NICH, noninvoluting congenital hemangioma | |
Table 1: International Society for the Study of Vascular Anomalies Classification System
Vascular malformations are either slow flowing (capillary, lymphatic, venous) or high flow (arterial). AVMs are defined as high flow lesions with direct communication between the arterial and venous supply, bypassing the intervening capillary bed (arteriovenous shunting) [2]. This bypass results in progressive vascular engorgement, venous hypertension, expansion and tissue destruction, causing aesthetic concerns and rarely, cardiac decompensation due to the high output state .
AVMs may be found in any site of the body, most commonly in the intracranial cavity. While rare, AVMs of the oral cavity pose a persistent and progressive benign disease process, with potentially life threatening complications including massive haemorrhage. This may occur spontaneously or during traumatic procedures such as dental extractions, tooth eruption or biopsy [8].
The origin and pathogenesis of AVMs still remains largely unknown. Genetic mutations and defective TGF-beta signalling have been proposed. Growth of the lesion and triggering of its symptoms can be exacerbated by trauma, ischemic events secondary to thrombosis, ectasia, hormonal changes and puberty. Studies have reported isolation of progesterone receptors in AVMs, accounting for their expansion during puberty [9]. Although 40-60% of AVMs are usually present at birth, about 30% become clinically apparent during childhood or adolescence [10]. Onset and progression is usually gradual, in proportion to physical growth. AVMs occur in equal frequency in males and females [10]. In certain cases, vascular malformations can be associated with underlying disease of systemic anomalies. Syndromes associated with AVMs include Bonnet-Dechaume-Blanc syndrome or Wyburn-Mason syndrome, Parkes-Weber syndrome, Capillary malformation- AVM syndrome, and Cobb syndrome [11] (Figures 3-8).
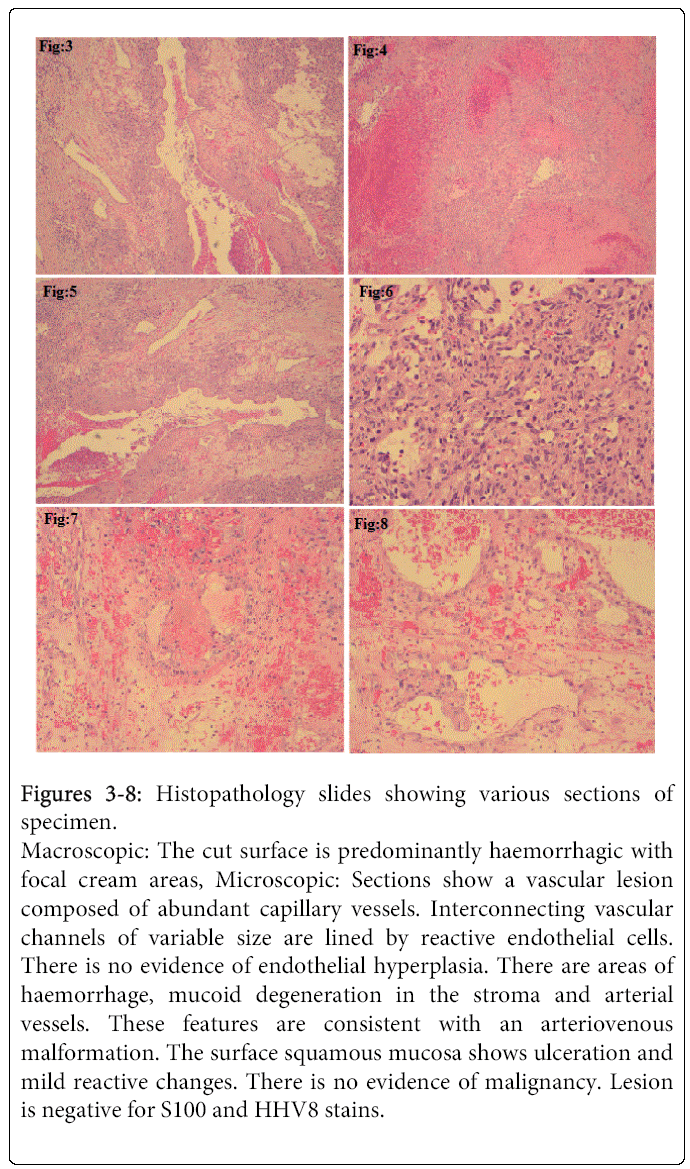
Figure 3-8: Histopathology slides showing various sections of specimen.
Macroscopic: The cut surface is predominantly haemorrhagic with focal cream areas, Microscopic: Sections show a vascular lesion composed of abundant capillary vessels. Interconnecting vascular channels of variable size are lined by reactive endothelial cells. There is no evidence of endothelial hyperplasia. There are areas of haemorrhage, mucoid degeneration in the stroma and arterial vessels. These features are consistent with an arteriovenous malformation. The surface squamous mucosa shows ulceration and mild reactive changes. There is no evidence of malignancy. Lesion is negative for S100 and HHV8 stains.
Typical presentation includes a pulsatile mass with a thrill, bruit, occasionally local hyperthermia, ulceration, or bleeding. Skin necrosis, ulceration and bleeding can result from shunting of blood, which reduces flow of nutrients. An erythematous blush or port wine stain may be present on the overlying skin [12]. Symptoms of AVMs are related to site of the lesion. In the oral cavity the anterior two thirds of tongue is the most common site, followed by the palate, gingiva and buccal mucosa [3]. This can interfere with mastication, speech and deglutition as a result of macroglossia. Pericoronal and gingival bleeding, occlusal anomalies and tooth mobility are often associated with intraosseous AVMs near the alveolar bone [13]. Diagnosis of AVM with plain radiography and computed tomography is limited. Radiographic features of an AVM include a poorly defined radiolucency, with a honeycomb or soap bubble appearance. However many may also appear normal on plain film. MRI is the investigation of choice as it shows the extent and lack of invasion in addition to the presence of “fast flow” vessels. Angiography is beneficial for embolization prior to surgery and in poorly defined cases as it depicts flow characteristics, parent vessels and dangerous anastomoses. Screening can be done by auscultation of the lesion and bedside doppler scanners. Flow characteristics can initially be assessed by ultrasound and colour doppler [9,14].
Histologically there is a mixture of abnormal thick and thin walled veins and arteries in close proximity to each other. Internal elastic lamina of arteries may be reduplicated, interrupted and distorted. The muscularis mucosa has a significant variation in thickness. Secondary changes include atherosclerosis, focal thrombosis, secondary dystrophic calcification, organisation and mild inflammation [15]. Vascular malformations have a normal endothelial cell cycle and mast cell population, compared to hemangiomas (vascular neoplasms), which are described as having a high endothelial cell turnover and mast cell proliferation [7,16]. Grossly, AVMs appear as hemorrhagic lesions with a spongy appearance on cross section. There is a non-encapsulated aggregation of intertwining, torturous medium or large sized arteries and veins in the submucosal tissues. Excessive or dilated lymphatic channels may be seen [16].
AVMs present a challenge to manage, due to high recurrence rates and replacement of normal tissue with disease vessels. In addition, vascular malformations such as AVMs are often associated with consumption coagulopathy, which can affect the use of sclerotherapy or embolization in treatment. Successful treatment may not be possible due to severe deficiency of normal clotting factors. Some cases have reported the use of cryoprecipitate, platelets or fresh frozen plasma in patients with chronic coagulopathy (low platelets, low fibrinogen, positive d dimers) prior to sclerotherapy or embolization [17].
Surgical resection of AVM can be associated with extensive blood loss, however incomplete resection may lead to tumour regrowth larger than its original size, which may be more difficult to manage. Proximal ligation of the parent vessel is ineffective and should be avoided as it can make future endovascular therapy difficult or impossible. Given the risks associated with surgical resection, conservative treatment may be indicated if an AVM is asymptomatic (Table 2).
| Location | Percentage Localisation |
|---|---|
| Cheek | 31% |
| Ear | 16% |
| Nose | 10% |
| Forehead | 10% |
| Upper lip | 7% |
| Mandible | 5% |
| Neck | 5% |
| Scalp | 4% |
| Maxilla | 4% |
Table 2: Locations of head and neck AVMs
However treatment is warranted for complications such as bleeding, pain, ulceration, excessive enlargement or heart failure, which have potentially life threatening consequences. Untreated lesions risk massive haemorrhage especially if subject to accidental trauma, or even during biopsy [16,17]. Multiple treatment, such as preoperative embolization and complete surgical resection is still the most conventional modern approach according to current literature [6].
There has been limited success with highly selective embolization as a single treatment modality for high flow lesions due to the later development of new vascular pathways. However it can be beneficial in significantly reducing blood flow within the vascular tumour, decreasing operative blood loss and permitting complete tumour resection [18]. Sclerosing agents such as sodium morrhuate and bleomycin provoke a severe intimal inflammatory reaction leading to thrombosis and shrinkage of the vascular anomaly [19]. They are associated with limited blood loss compared to surgical resection, with immediate venogram and control angiogram showing thrombosis of the lesion. Some studies have reported positive results when combined with surgical treatment, however more research is needed to determine the role of agents these in conventional treatment. Ethanol embolization of AVMs via direct puncture has been reported in several cases with some success, however in high-flow AVMs, ethanol can quickly wash through toward the venous side, losing its thrombogenic properties [20]. Minor complications such as skin and transient peripheral nerve injuries have also been documented [21]. In this case, given the extent of bleeding and increasing size of the lesion affecting quality of life, surgery was the treatment of choice for our patient. The surgical approach should be large enough to allow complete removal of the lesion. Regular follow up on a yearly basis was recommended for this patient, to monitor any signs of recurrence.
Conclusion
This case demonstrates a rare case of an AVM of the buccal mucosa which was successfully treated by surgical excision. Although rare, clinicians should be aware of their potentially life threatening complications. This can be avoided by early detection and intervention, with adequate follow up to monitor recurrence.
Acknowledgement
Thankyou to the following for input in this case presentation: Dr Matthew Hawthorne (OMFS consultant), Dr Anthony Crombie (OMFS consultant), Dr Rachel Hseih (OMFS Registrar), Prof. Neil Savage (Oral Medicine Specialist)
References
- Martinez F, Immordino V (2009) Arteriovenous malformation of the base of tongue in pregnancy: case report. ActaOtorhinolaryngolItal 29: 274-278.
- Duncan IC, Fourie PA (2004) Vascular malformations. Part 2. Current classification of vascular malformations. SA Journal of Radiology 23-30.
- Shetty DC, Urs AB, Rai HC, Ahuja N, Manchanda A (2010) Case series on vascular malformation and their review with regard to terminology and categorisation. Contemporary Clinical Dentistry 1: 259-262.
- Mulliken JB, Glowacki J (1982) Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. PlastReconstrSurg 69: 412-422.
- Mulliken JB, Glowacki J (1982) Classification of pediatric vascular lesions. PlastReconstrSurg 70: 120-121.
- Garzon MC, Huang JT, Enjolras O, Frieden IJ (2007) Vascular malformations. Part 1. J Am AcadDermatol 56: 353-370
- Lowe LH, Marchant TC, Rivard DC, Scherbel AJ (2012) Vascular Malformations: Classification and terminology the radiologist needs to know. SeminRoentgenol 47: 106-117
- Marler JJ, Mulliken JB (2005) Current management of hemangiomas and vascular malformations. ClinPlastSurg 32: 99-116
- Manjunath MS, Shetty S, Moon NJ, Sharma B, Metta KK, et al. (2014) Case report: Arteriovenous malformation of the oral cavity. Case Reports in Dentistry Article ID 353580.
- Krebs LT, Shutter JR, Tanigaki K, Honjo T, Stark KL, et al. (2004) Haploinsufficient lethality and formation of arteriovenous malformations in notch pathway mutants. Genes Dev 18: 2469-2473.
- Garzon MC, Huang JT, Enjolras O, Frieden IJ (2007) Vascular malformations. Part II: associated syndromes. Journal of the American Academy of Dermatology. 56: 541-564.
- Chiu H. et al. (2011) A giant venous malformation of face and neck: a case report. Taiwan J Oral MaxillofacSurg 22: 110-117.
- Anderson JH, Grisius RJ, McKean TW (1981) Arteriovenous malformation of the mandible. Oral Surg Oral Med Oral Path 52:118-125.
- Dubois J, Garel L (1999) Imaging and therapeutic approach of hemangiomas and vascular malformations in the pediatric age group. PediatrRadiol. 29: 879-893.
- Pujari M, Bahirwani S, Balaji P, Kaul R, Shah B, et al. (2011) Arteriovenous malformation of the tongue: A case report and review of the literature. JIAOMR 23: 139-142.
- Okhan O, Funda Y, Ozenc M, Ulku B, Lacin B, et al. (2007) Arteriovenous malformation of the mandible: A case report. Quintessence international 38: 470-476.
- Noreau G, Landry PE, Morais D (2001) Arteriovenous malformation of the mandible: review of literature and case history. J Can Dent Assoc 67: 646-651.
- Bhandari PS, Sadhotra LP, Bhargava P, Bath AS, Mukherjee MK, et al. (2008) Management focal strategy for facial arteriovenous malformations. Indian J PlastSurg 41: 183-189.
- Jackson IT, Keskin M, Yavuzer R, Kelly CP (2005) Compartmentalisation of massive vascular malformations, PlastReconstr Surg. 115:10-12.
- Fan XD, Su LX, Zheng WJ, Zheng LZ, Zhang ZY (2009) Ethanol Embolization of Arteriovenous Malformations of the Mandible. Am J Neuroradiol 30: 1178-1183
- Do YS, Yakes WF, Shin SW, Lee BB, Kim DI et al. Ethanol Embolisation of Arteriovenoue Malformations: Interim Result. Radiology 235: 674-682.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 25451
- [From(publication date):
March-2015 - Jul 05, 2025] - Breakdown by view type
- HTML page views : 20185
- PDF downloads : 5266