Appropriate Timing of Enteral Nutrition in Comatose Acute Stroke Patients
Received: 22-Apr-2020 / Accepted Date: 06-May-2020 / Published Date: 13-May-2020 DOI: 10.4172/2476-2024.1000164
Abstract
Too early initiation of enteral nutrition (EN) is not advantageous for comatose acute stroke patients. In those patients, the reduction of total protein and albumin was little at day 2 of admission. But the reduction became significant after day 3. Therefore, appropriate nutritional support should be initiated within day 2 after admission in comatose acute stroke patients. When EN started from day 4, recovery of hypoptoteinemia was poor. On the other hand, rapid recovery from hypoptoteinemia was recognized when total parenteral nutrition (TPN) and 20% glucose tube feeding were administered to the patients from Day 4. And incidence of diarrhea was extremely high when EN was initiated from day 4, causing hypoproteinemia, hypovolemia, and unbalance of electrolytes. In acute phase, hypercatabolism occurs in severe stroke patients, and active administration of amino acids and protein may adversely affect nitrogen balance. In hypercatabolism condition, a simple glucose solution is more acceptable than EN. Therefore, for comatose acute stroke patients, TPN and glucose tube feeding should be initiated within 48 hours.
Keywords: Comatose; Acute; Stroke; Enteral nutrition; Hypoptoteinemia; Hypercatabolism
Nutritional status in acute stroke patients
Poor nutritional conditions in acute stroke patients lead to unfavorable functional recovery [1-3]. However, the nutritional status in acute stroke patients may steadily deteriorate during hospitalization in spite of adequate nutritional support [4,5], and half of the patients admitted to inpatient rehabilitation stroke centers are undernourished [6]. Some papers tried early initiation of enteral tube feeding to those patients, initiating enteral nutrition (EN) within 24 or 48 hours after admission; however, they concluded there were little advantage in early initiation of EN [7-9].
An article mentioned that too early initiation of enteral nutrition is not nutritionally advantageous for comatose acute stroke patients [10]. Two things should be disclosed to maintain a good nutritional condition in comatose acute stroke patients; 1) when nutritional intervention should start and 2) what type of intervention should be employed: total parenteral nutrition (TPN) or EN.
Deterioration of serum total protein (TP) and albumin in acute phase of stroke, and appropriate timing to start nutritional intervention
The patients who fulfilled the following criteria were nominated in our study:
1) Who is older than 40 years,
2) Whose consciousness level is less than 12 (E3V4M5) on the Glasgow Coma Scale, and
3) Who is unable to eat or drink for at least 21 days.
And the following patients were excluded from the study:
1) Who underwent emergency operation under general anesthesia,
2) Who had hypoproteinemia (<6.0 g/dL TP or <3.0 g/dL albumin) on admission because of complications,
3) Who had aspiration pneumonia on admission,
4) Who showed watery diarrhea after initiating EN, and
5) Who died within 21 days. Two hundred seventy three patients with acute stroke were enrolled and 164 patients completed our study.
The day of admission was defined as day 0. The patients were received intravenous low-calorie solutions of 10 kcal/kg/day until day 3. The blood glucose level was controlled at less than 150 mg/dL using rapid-acting insulin. Concentrations of serum TP and albumin were measured on Day 0, 2, 3, and 4. Microsoft Office Excel 2010 was used for statistical analysis. The Student t-test was applied to determine statistically significant differences between two groups. To identify statistically significant differences between more than 2 variables, the Steel-Dwass test was used. In all tests, P (probability) values less than 0.05 (P<0.05) were considered statistically significant.
As shown in Figure 1A, reductions in the serum TP and albumin concentrations were not significant on Day 2, but both concentrations decreased significantly after Day 3 (P<0.01) and decreased further on Day 4 (Figure 1A). More than 80% of the reduction of the serum TP was a result of a loss of albumin. Age was not a risk factor for proteinenergy reduction because no significant differences were identified in the reduction of either serum TP or albumin concentrations between the patients who are younger than 70 years old (<70) and 70 years or older (≧ 70) (Figures 1B and 1C). According to Unosson et al., the serum albumin concentration is related to nutritional risk as follows: >3.5 g/dL, no risk; 3.0 to 3.5 g/dL, low risk, 2.5 to 3.0 g/dL, moderate risk; and <2.5 g/dL, high risk [11]. Appropriate nourishments should be provided to the stroke patients in a low risk of nutritional condition. Based on our data, the nutritional support should be initiated by Day 2 (within 48 hours).
Figure 1: A: TP and Albumin: At Day 2, reduction of TP and albumin was less than 0.5g/dL. But both TP and albumin decreased significantly after Day 3 (P<0.01). B: TP: There is no difference in TP reduction between younger than 70 years old (<70) and 70 and older ( ≧ 70). C: Albumin: No statistical difference was identified in Albumin decrease between younger than 70 years old (<70) and 70 and older ( ≧ 70).
What kind of nutrition should be employed for early nutritional intervention?
From day 4, nutrition of 25 kcal/kg/day was initiated. Concentrations of serum TP and albumin were measured on Day 10, 14, and 21.
The patients were assigned into the following four groups in order of hospitalization;
Group 1: TPN and 20% glucose tube feeding from Day 4 to 13, and changed to EN from Day 14,
Group 2: TPN was start on Day 4 and continued to Day 21,
Group 3: TPN was administered on Day 4 through 13, and 400 kcal/day of EN was begun on Day 14. The volume of EN was increased step-wise with concurrent tapering of the TPN, to maintain a total caloric intake of 25 kcal/kg/day,
Group 4: EN (25 kcal/kg/day) was started on Day 4 and continued until Day 21.
For tube feeding, a 14-French nasogastric tube was inserted into a patient’s stomach from the nostril up to a length of 55 to 60 cm at the time of admission.
The patients were in a head-up position of 45°-to-60° during EN feedings and kept in this position for 1 hour after finishing the feeding. In order to avoid diarrhea, the EN of 1 kcal/mL was diluted to 1.5 times with warm water and administered in the diluted form.
Instead of EN, 20% glucose was used in Group 1 based on a report in a dog mentioning that 20% glucose solution stimulates bowel movements and increases the blood flow of the superior mesenteric artery [12].
Recovery of Total protein
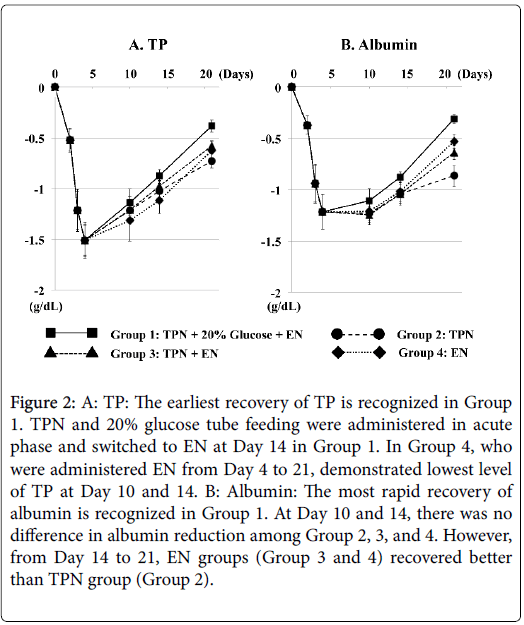
The most rapid recovery in serum TP was recognized in Group 1 (TPN and 20% glucose tube feeding). At Day 10 and 14, statistical differences were not identified among Groups 1, 2, 3, and 4 (Figure 2). However, at Day 21, TP level was significantly higher in Group 1 than in any other groups [Group 1:Group 2 P<0.05, Group 1:Group 3 P<0.01, Group 1:Group 4 P<0.05, Group 2:Group 3 P>0.05, Group 2:Group 4 P>0.05, Group 3:Group 4 P>0.05]. Group 2, only TPN, demonstrated same recovery of TP as Group 3 and Group 4 until Day 14; however, TP level was lowest at Day 21. Group 4, EN from Day 4, showed poorest recovery until Day 14, but recovery of TP and albumin was better than Group 2 or Group 3 from Day 14 to Day 21.
Figure 2: A: TP: The earliest recovery of TP is recognized in Group 1. TPN and 20% glucose tube feeding were administered in acute phase and switched to EN at Day 14 in Group 1. In Group 4, who were administered EN from Day 4 to 21, demonstrated lowest level of TP at Day 10 and 14. B: Albumin: The most rapid recovery of albumin is recognized in Group 1. At Day 10 and 14, there was no difference in albumin reduction among Group 2, 3, and 4. However, from Day 14 to 21, EN groups (Group 3 and 4) recovered better than TPN group (Group 2).
Recovery of Albumin
Group 1 demonstrated the earliest serum albumin recovery and the level of albumin was significantly higher in Group 1 than in any other Groups after Day 10. At Day 10 and 14, there are no difference between Group 2, 3, and 4; however, Group 2, only TPN, demonstrated the lowest level of albumin at Day 21 [Group 1:Group 2 P<0.05, Group 1:Group 3 P<0.01, Group 1:Group 4 P<0.05, Group 2:Group 3 P<0.05, Group 2:Group 4 P<0.05, Group 3:Group 4 P>0.05].
In Group 1 and 2, there were no patients with watery diarrhea. Watery diarrhea requiring discontinuation of EN was identified in 22 patients among 52 (42.3%) in Group 3, and in 30 patients among 62 (48.4%) in Group 4.
It is obvious in our data that the appropriate nutrition should be initiated within 48 hours in comatose acute stroke patients after the onset. Maintaining good nutritional condition is important; however, more important things for acute stroke patients are controls of blood pressure, water balance, blood glucose, and electrolytes. It is hard to control those factors by EN because it is unsure that how much volume and calories were absorbed from gastrointestinal system. TPN is more convenient to measure water balance and to control blood glucose and electrolytes. Hypercatabolism is common in acute severe stroke patients [13,14] and aggressive nutritional support does not prevent substantial total protein loss during this hypercatabolic state [15]. In hypercatabolic condition, a simple glucose solution is more acceptable than EN, because active administration of amino acids and protein may adversely affect nitrogen balance and increase the concentration of blood urea nitrogen [14]. Another disadvantage of an early start of EN in comatose acute stroke patients was the high incidence of diarrhea. Even with adequate EN supplementation, diarrhea can occur in acute phase of severe stroke. Diarrhea accelerates hypovolemia, hypoproteinemia, and hypoalbuminemia, and might cause unbalance of electrolytes.
Conclusion
Based on this study, the author concluded that EN is not adequate for early nutritional support for comatose acute stroke patients. For comatose acute stroke patients, TPN and 20% glucose tube feeding must be initiated within 48 hours after stroke onset, and should be switched to EN after 7 to 10 days.
References
- FOOD Trial Collaboration (2003) Poor nutritional status on admission predicts poor outcomes after stroke: observational data from the FOOD trial. Stroke 34: 1450-1456.
- Aptaker RL, Roth EJ, Reichhardt G, Duerden ME, Levy CE (1994) Serum albumin level as a predictor of geriatric stroke rehabilitation outcome. Arch Phys Med Rehabil 75: 80-84.
- Belayev L, Liu Y, Zhao W, Busto R, Ginsberg MD (2001) Human albumin therapy of acute ischemic stroke: marked neuroprotective efficacy at moderate doses and with a broad therapeutic window. Stroke 32: 553-560.
- Friedmann JM, Jensen GL, Smiciklas-Wright H, McCamish MA (1997) Predicting early nonelective hospital readmission in nutritionally compromised older adults. Am J Clin Nutr 65: 1714-1720.
- Gariballa SE (2001) Malnutrition in hospitalized elderly patients: when does it matter? Clin Nutr 20: 487-491.
- Foley NC, Salter KL, Robertson J, Teasell RW, Woodbury MG (2009) Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke 40: e66-74.
- Nyswonger GD, Helmchen RH (1992) Early enteral nutrition and length of stay in stroke patients. J Neurosci Nurs 24: 220-223.
- Rowat A (2015) Enteral tube feeding for dysphagic stroke patients. Br J Nurs 2: 142-145.
- Yuan F, Yang F, Zhang W, Jia Y, Ma Y, et al. (2019) OPENS study group. Optimizing early enteral nutrition in severe stroke (OPENS): protocol for a multicentre randomized controlled trial. BMC Neurol 19:24.
- Yamada SM (2015) Too early initiation of enteral nutrition is not nutritionally advantageous for comatose acute stroke patients. J Nippon Med Sch 82: 186-192.
- Unosson M, Ek AC, Bjurulf P, von Schenck H, Larsson J (1994) Feeding dependence and nutritional status after acute stroke. Stroke 25: 366-371.
- Yoshida M, Tajika S, Fujimaki M (1992) An experimental study of the effect of intravenous hyperalimentation and enteral feeding on intestinal blood flow. Jap J Surg Metab Nutr 26: 390-400.
- Wilmore DW (1991) Catabolic illness. Strategies for enhancing recovery. N Engl J Med 325: 695-702.
- Chalela JA, Haymore J, Schellinger PD, Kang DW, Warach S (2004) Acute stroke patients are being underfed: a nitrogen balance study. Neurocrit Care 1: 331-334.
- Dziewas R, Ritter M, Schilling M, Konrad C, Oelenberg S, et al. (2004) Pneumonia in acute stroke patients fed by nasogastric tube. J Neurol Neurosurg Psychiatry 75: 852-856.
Citation: Yamada SM (2020) Appropriate Timing of Enteral Nutrition in Comatose Acute Stroke Patients. Diagn Pathol Open 5: 164. DOI: 10.4172/2476-2024.1000164
Copyright: © 2020 Yamada SM. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3748
- [From(publication date): 0-2020 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 2991
- PDF downloads: 757