Research Article Open Access
Appropriate Head Position for Nasotracheal Intubation by Using Lightwand Device
Yozo Manabe1*, Shigeru Iwamoto2, Mika Seto3 and Kazuna Sugiyama41Department of Systemic Management for Dentistry, Kagoshima University Medical and Dental Hospital, Kagoshima, Japan
2Section of Anesthesiology, Department of Diagnostics and General Care, Fukuoka Dental College, Fukuoka, Japan
3Department of Dentistry and Oral Surgery, Fukuoka University, Fukuoka, Japan
4Department of Dental Anesthesiology, Kagoshima University, Graduate School of Medical and Dental Sciences, Kagoshima, Japan
- Corresponding Author:
- Yozo Manabe
Department of Systemic Management for Dentistry
Kagoshima University Medical and Dental Hospital
Kagoshima, 8-35-1, Sakuragaoka
Kagoshima 890-8544, Japan
Tel: +81- (0) 99-275-6561
Fax: +81- (0) 99-275-6288
E-mail: manabey@dent.kagoshima-u.ac.jp
Received Date: December 12, 2013; Accepted Date: January 20, 2014; Published Date: January 22, 2014
Citation: Manabe Y, Iwamoto S, Seto M, Sugiyama K (2014) Appropriate Head Position for Nasotracheal Intubation by Using Lightwand Device. J Interdiscipl Med Dent Sci 2:109. doi: 10.4172/2376-032X.1000109
Copyright: © 2014 Manabe Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Background: The purpose of this study was to determine the relationship between the head position and the subsequent ease of nasotracheal intubation by using lightwand device TrachlightTM (TL).
Methods: Patients requiring nasotracheal intubation were subdivided into three groups according to the intubated head position (Group S: sniffing position, Group E: extension position, Group N: neutral position). The number of attempts, the total intubation time, and the failures of the TL intubation were recorded. Intubation difficulty by means of TL was assessed by the original 6-point scale.
Results: Of total 300 patients enrolled in the study, TL intubation was successful in the patients of 91.3%. No correlation between the original scale and the head position was observed.
Conclusion: TL is an effective alternative for patients who require nasotracheal intubation. We could not find the favorable head position for nasotracheal intubation with TL, so we recommend that the nasotracheal intubation with TL should be started with neutral position and have to find the appropriate head position individually.
Keywords
Nasotracheal intubation; Light wand device (trachlight™); Appropriate head position
Introduction
Nasotracheal intubation is often indicated in oral and maxillofacial surgery. An alternative orotracheal intubation technique using a lightwand device Trachlight™ (TL; Laerdal Medical, Armork, NY) has been reported to facilitate tracheal intubation in patients with difficult airways [1]. Some reports discussing the validity of using TL for nasotracheal intubation are available [2,3]. In addition, the incidence of complications with light-guided intubation is reported to be low because elevation of the epiglottis by the laryngoscope blade is not required [4,5].
The sniffing position is widely considered essential to the performance of orotracheal intubation for the direct laryngoscopy. In most cases fiber optic nasotracheal intubation would be started with neutral head position. But there is no report about the difficulty of nasotracheal intubation using TL in relation to the head position.
This study was designed to determine the relationship between the head position and the subsequent ease of nasotracheal intubation by TL.
Methods
This study was approved by the Institutional Review Board at the Fukuoka Dental College (Fukuoka Dental college, 2-15-1 Tamura, Sawara-Ku, Fukuoka, Japan, approved April 4, 2005, Approval number: 66), and written informed consent was obtained from each patient.
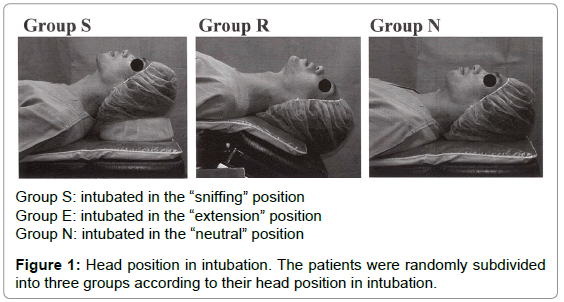
This study included patients (ASA 1 or 2) scheduled to undergo elective oral and maxillofacial surgery under general anesthesia that required nasotracheal intubation and the patients who had past history of the upper airway surgery and BMI>30 kg/m2 were excluded from the study. They were randomly assigned to three equal-sized groups (n=100) according to their head position for lightwand nasotracheal intubation: Group S intubated in the sniffing position; Group E intubated in the extension position; Group N intubated in the neutral position. The sniffing position was obtained by placement of a 9-cm cushion under the head of the patient [6]. The extension position was obtained by bending the head part of the bed at an angle of 30 degrees posteriorly and the neutral position was obtained by just lying on the flat bed without cushion (Figure 1). They underwent a preoperative airway assessment that included a Mallampati score [7,8] and mouth opening with the mouth fully opened (the interincisor gap was measured in millimeters) by an attending anesthesiologist. Demographics such as age, gender, weight, and height were also recorded.
Group S: intubated in the √ʬ?¬?sniffing√ʬ?¬Ě position
Group E: intubated in the √ʬ?¬?extension√ʬ?¬Ě position
Group N: intubated in the √ʬ?¬?neutral√ʬ?¬Ě position
Figure 1: Head position in intubation. The patients were randomly subdivided into three groups according to their head position in intubation.
Each patient was routinely monitored during the entire procedure. A rapid-acting anesthetic (propofol, 1–1.5 mg/kg, or thiamylal, 3–5 mg/kg) was administered intravenously, mask ventilation was ensured, and vecuronium bromide (0.1 mg/kg) was administered. The nasal mucosa of both nostrils was disinfected and probed with absorbent cotton immersed in 10% povidone-iodine with 1:100,000 epinephrine and the wider patent nostril was chosen for intubation. Then, lidocaine jelly was used as a lubricating jelly for nasopharyngeal airway tubes, which had increasing caliber sizes to dilate the meatus of the selected nasal cavity. The laryngoscopy was performed in all cases by using a size 3 Macintosh laryngoscope blade for topical anesthesia on the supraglottic region and the vocal cords using 8% lidocaine spray. This process is standardized in our department [9]. Glottis visualization during laryngoscopy was assessed by using the Cormack and Lehane classification [10] by an attending anesthesiologist with at least 3 years of anesthesia experience. All direct laryngoscopy were performed in sniffing position.
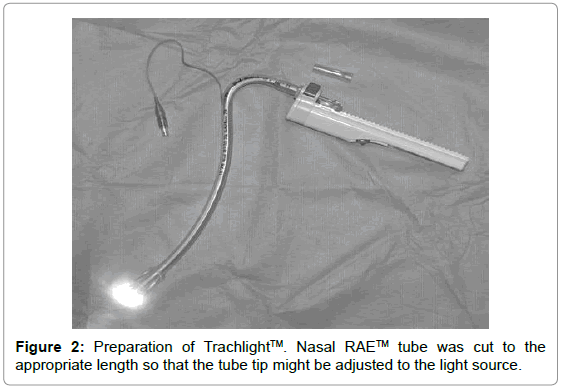
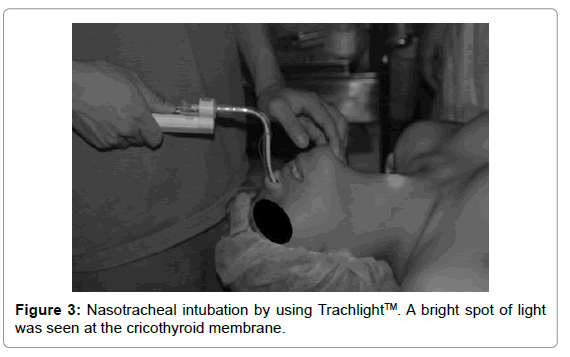
Nasal RAE™ endotracheal tubes (NTT; Mallinckrodt, Glens Falls, NY) were used in this study. Each NTT was cut to the appropriate length so that the tube tip could be adjusted to the light source. The NTT was inserted with the TL after removal of the stylet (TL-NTT) (Figure 2) and soaking in warm sterilized normal saline to reduce epistaxis and nasal damage [11]. The TL-NTT was inserted into the nostril and advanced until light was seen in the oropharynx. After further advancing, a blurred light was seen in the sub-mandibular area. The TL-NTT tip was maneuvered anteromedially until a bright spot of light was seen at the cricothyroid membrane (Figure 3); the TL was then withdrawn and the NTT advanced into the trachea. The cuff of the tracheal tube was inflated with air at the peak airway pressure of 25 cm H2O immediately after intubation to prevent leaks. The location of the NTT tip was confirmed by palpation of the pilot balloon at the level of the suprasternal notch and by capnography. If the intubation was not performed within 60 s or a decrease in arterial oxygen saturation by pulse oximrtry below 98% was observed, the TL was withdrawn, the opposite nostril and mouth were covered by hand, and ventilation through the NTT was resumed. Three attempts were permitted with ventilation interposed. If the TL intubation was unsuccessful after three consecutive attempts, intubation was performed using direct laryngoscopy. Only one anesthesiologist with 20 years’ experience who was blinded to the preoperative assessment and Cormack and Lehane classification results performed all of the intubations using TL. Intubation difficulty was assessed by the original 6-point scale (Table 1). The number of attempts, the total intubation time, and the failures of the TL intubation were recorded by another anesthesiologist. The total intubation time was defined as the sum of all intubation attempt durations, but the total time of interposed ventilation was excluded. The duration of each attempt was defined as the time from inserting the TL-NTT into the nostril to the time when the TL was removed from the NTT.
| Score | Description | Classification criterion |
|---|---|---|
| 1 | Very easy | Successfully intubated within 15 sec. at the first attempt |
| 2 | Easy | Successfully intubated between 15 and 30 sec. at the first attempt |
| 3 | Moderate | Successfully intubated more than 30 sec. at the first attempt |
| 4 | Difficult√?¬†√?¬†√?¬†√?¬†√?¬† | Successfully intubated at the second attempt |
| 5 | Very difficult√?¬†√?¬† | Successfully intubated at the third attempt |
| 6 | Unsuccessful | Intubation could not be achieved with three attempts of using the lightwand devise |
Table 1: Original 6-point scale of nasotracheal intubation difficulty Abbreviations same as Figure 1.
Statistics
Ratio of gender, nostril side, distribution of Mallampati class, Cormack and Lehane classification between groups were analyzed using χ2-test. Intubation difficulty between groups was analyzed using Kruskal-Wallis test. For the comparison of other data, ANOVA with Sheffe’s post-hoc test was performed. All statistical analyses were performed using Stat View version 5.0 (SAS Institute Inc., Cary, NC, USA). Data are presented as number of patients and mean (SD). P<0.05 was considered statistically significant.
Results
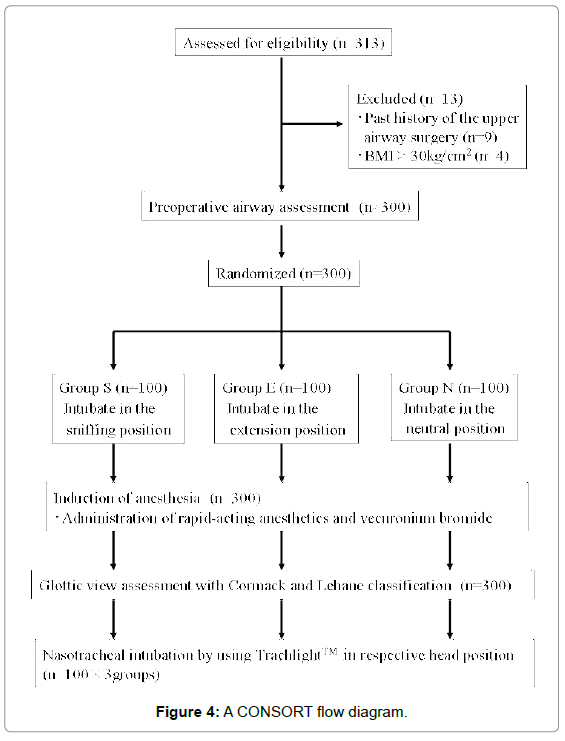
A total of 300 patients were enrolled into the study (Group S: n=100, Group E: n=100, Group N: n=100). There were no significant differences among the three groups in terms of height, weight, or the ratio of gender (Table 2). A CONSORT flow diagram is shown in Figure 4. There were no significant differences in the ratio of the nostril side, cuff volume, interincisor gap, and the tube size (Table 3). TL intubation was successful in 274 of the 300 patients (91.3%), and it failed in 26 (8.7%). Two hundred forty patients (80.0%) were intubated at the first attempt, 19 (6.3%) required a second attempt, and 15 (5.0%) required a third attempt. There was no significant difference in the success rate of the first attempt between the groups. The total intubation time was not significantly different among the three groups (Table 3). Distribution of Mallampati score and Cormack and Lehane grade in each groups were not significantly different (Tables 4 and 5). There were 9 unsuccessful cases in Group S, 7 unsuccessful case in Group E, and 10 unsuccessful cases in Group N. No significant differences in the ratio of unsuccessful cases were found among the groups (Table 6). In all cases, tracheal intubation was performed without severe hemodynamic instability. There were no adverse outcomes.
| No.of patients | Group S (n=100) | Group E (n=100) | Group N (n=100) |
|---|---|---|---|
| Gender (M/F) | 44/56 | 38/62 | 39/61 |
| Age (yr) | 35.5±15.3 | 36.0±16.1 | 33.0±17.4 |
| Height (cm) | 163±7.8 | 162.5±8.5 | 162.6±8.0 |
| Weight (kg) | 56.4±9.5 | 57.2±10.7 | 56.4±9.3 |
Table 2: Patient demographics. Abbreviations same as Figure 1. Data are presented as mean ± SD.
| No.of patients | Group S (n = 100) | Group E (n = 100) | Group N (n = 100) |
|---|---|---|---|
| Interincisor gap (cm) | √?¬†44.6±7.1 | 43.9±7.7 | 45.2±5.8 |
| Tube size (cm) | 7.6±0.4 | 7.5±0.4 | 7.6±0.4 |
| nostril side (right/left) | 62/38 | 66/34 | 75/25 |
| Cuff volume (ml) | 3.6±1.2 | 3.9±1.6 | 4.0±1.5 |
| Total time to Intubate (Sec) | 17.4±29.0 | 16.9±25.6 | 20.7±35.7 |
| Percentage of patients | |||
| √?¬†intubated at the first attempt (%) | 77.0 | 83.0 | 80.0 |
| Percentage of patients | |||
| √?¬†intubated at the second attempt (%) | 4.0 | 8.0 | 7.0 |
| Percentage of patients | |||
| √?¬†intubated at the third attempt (%) | 10.0 | 2.0 | 3.0 |
| Success rate (%) | 91.0 | 93.0 | 90.0 |
Data are presented as mean ±SD. & %
Table 3: Result of measurement. Abbreviations same as Figure 1.
| No.of patients | Group S (n = 100) | Group E (n = 100) | Group N (n = 100) |
|---|---|---|---|
| Mallampati score class 1√?¬† (n=228) | 79 | 77 | 72 |
| Mallampati score class 2√?¬† (n=54) | 15 | 16 | 23 |
| Mallampati score class 3√?¬† (n=9) | 3 | 2 | 4 |
| Mallampati score class 4√?¬† (n=9) | 3 | 5 | 1 |
Table 4: Distribution of Mallampati score in each Head position. Abbreviations same as Figure 1.
| No.of patients | Group S (n = 100) | Group E (n = 100) | Group N (n = 100) |
|---|---|---|---|
| Cormack-Lehane score grade 1√?¬† (n = 247) | 85 | 85 | 77 |
| Cormack-Lehane score grade 2√?¬† (n = 32) | 10 | 9 | 13 |
| Cormack-Lehane score grade 3√?¬† (n =√?¬† 21) | 5 | 6 | 10 |
| Cormack-Lehane score grade 4√?¬† (n =√?¬† 0) | 0 | 0 | 0 |
Table 5: Distribution of Cormack-Lehane grade in each Head position. Abbreviations same as Figure 1.
| No.of patients | Group S (n = 100) | Group E (n = 100) | Group N (n = 100) |
|---|---|---|---|
| Score √Į¬ľ¬?√£¬?¬?“Very easy” (n =216) | 71 | 75 | 70 |
| Score 2√?¬† “Easy” (n = 11) | 2 | 2 | 7 |
| Score 3√?¬† “Moderate”√?¬† (n = 13) | 4 | 6 | 3 |
| Score 4√?¬† “Difficult”√?¬† (n = 19) | 4 | 8 | 7 |
| Score 5√?¬† “Very difficult” (n = 15) | 10 | 2 | 3 |
| Score 6√?¬† “Impossible” (n = 26) | 9 | 7 | 10 |
Table 6: Relation between Original 6-point scale and Head position. Abbreviations same as Figure 1.
Discussion
Nasotracheal intubation using a light guide has been reported since 1959 [12]; however, no report has focused on nasotracheal intubation difficulty using TL in relation to the head position.
Nasotracheal intubation using TL has been performed in several cases and a number of institutions use TL as the first choice of orotracheal intubation method [13]. In “Difficult Airway Algorithm” of American Society of Anesthesiologists [14], TL is also shown to be one of the instruments used as an intubation method for patients who are easy to ventilate manually but found to have difficult laryngoscopy after induction of anesthesia. Park et al. [6] reported that the laryngoscopic view with the 9-cm pillow was significantly superior to that with other pillows and without pillow; therefore we applied 9-cm cushion to the sniffing position. Hung et al. have reported that TL should be avoided in patients with known anatomical abnormalities of the upper airway [15]. Therefore, postoperative patients, who had anatomical abnormalities of the upper airway resulting from oral surgery, were excluded from this study.
TL intubation was successful with an average time of 18.3 sec, and it is very similar to the report (17.6 ± 6.6sec) of Cheng et al. [16]. The success rate of nasotracheal intubation by TL in this study was 91%. Cheng et al. [13] also reported that the success rate of nasotracheal intubation by TL was 96.7% at first attempt, and 100% at second attempt, but they performed tracheal tube cuff inflation technique [17] to the all patients.
One of the reasons for this low success rate is that cases in which the patients could not be intubated in 3 attempts were classified as ‘unsuccessful’ on the basis of the report by Fox et al. [18], which shows that the average number of attempts required for blind nasotracheal intubation by an experienced anaesthesiologist is 3.1 times. However, we have had cases in which TL nasotracheal intubation was successful after four or more attempts in the clinical setting. The other potential reason that can be considered is carrying out the three consecutive attempts in the same head position, because the appropriate head position for nasotracheal intubation with TL may differ among patients, similar to the blind nasotracheal intubation procedure. We recommend that the nasotracheal intubation with TL should be started with the neutral position, because this position is intermediate position of the sniffing position and the extension position.
Nasotracheal intubation by TL is unsuccessful when the tube is inserted into the esophagus or when the tube is lodged in the tissue surrounding the epiglottis and cannot be advanced into the trachea. In the former case, it is often possible to insert the tube by extending the neck to raise the tube tip. When it is difficult to perform the intubation in this manner, changing the tube to the Endotrol tube is contemplated [19]. However, during oral and maxillofacial surgery, the use of the RAE™ tube with suitable flexion is encouraged because the connector of the anesthetic circuit and the tracheal tube disturbs the sight of the surgeon when it is located above the patient’s nose. Iseki et al. [20] have reported that the tip of the tracheal tube can be raised by the alteration of the TL; however, this method cannot be applied to the RAE™ tube. In clinical condition, we raised the tip of the tube by the tracheal tube cuff inflation technique [17] and had good results. This technique is reported to increase the success rate of blind nasotracheal intubation.
Management of the case wherein the tube cannot advance into the trachea is more difficult. In such cases, we try various head positions; however, most of these cases came to be “unsuccessful” cases.
In case of intubation using a lightwand, the advantage is that the precise position of an endotracheal tube tip is known by checking the light at the sternal notch [21]. Since the length up to a bent part of the RAE™ tube is provided, it is necessary to set an appropriate fixed length.
It has been accepted that intubation with a direct laryngoscopy is difficult for grades 3 and 4 of the Cormack and Lehane classification. Ainsworth et al. [22] have reported that the difficulty of oral intubation with lightwand has no relation to the grade of laryngoscopic view according to the Cormack and Lehane classification. Hung et al. [5] have reported that the Mallampati classification correlated with the intubation time by using the laryngoscope but did not correlate with the time by using TL. Manabe et al. have reported that there is no correlation between the difficulty of nasotracheal [9] intubation using TL and the Mallampati classification or the Cormack and Lehane classification.
There was no correlation between the airway parameters and the time required for intubation using the TL.
In other words, nasotracheal intubation using TL was not influenced by anatomic variability in this population.
In addition, intubation using TL is a light-guided technique without visualization of the laryngeal structures; therefore, there is a potential risk of trauma to the upper airway associated with its use, but there were no adverse outcomes in this study.
Our study has several limitations. First, all intubations were performed by one operator; therefore, the results may be biased towards the expertise of that operator. However, patients were unintentionally sampled so that the head positions could be equally dispersed through the study period, and this operator had a great deal of experience in nasotracheal intubation using TL from the beginning of this study. Second, premedication or anesthesia methods were not unified. Nevertheless, all patients had 0.1mg/kg of vecuronium bromide; therefore, we consider that the difference in anesthesia method could be ignored.
In conclusion, Trachlight™ is an effective alternative for patients who require nasotracheal intubation and there was no relationship between the ease of nasotracheal intubation using the TL and the head position. Because the neutral head position is intermediate position of sniffing and extension position so that we can change to the appropriate head position by one motion, we recommend that the nasotracheal intubation with TL should be started with neutral position and have to find the appropriate head position individually.
Conclusion
TL is an effective alternative for patients who require nasotracheal intubation. We could not find the favorable head position for nasotracheal intubation with TL, so we recommend that the nasotracheal intubation with TL should be started with neutral position and have to find the appropriate head position individually.
References
- Hung OR, Pytka S, Morris I, Murphy M, Stewart RD (1995) Lightwand intubation . Clinical trial of a new lightwand for tracheal intubation in patients with difficult airway. Can J Anaesth 42: 826-830.
- Weis FR, Hatton MN (1989) Intubation by use of the light wand: experience in 253 patients. J Oral Maxillofac Surg 47: 577-580.
- Favaro R, Tordiglione P, Di Lascio F, Colagiovanni D, Esposito G, et al. (2002) Effective nasotracheal intubation using a modified transillumination technique. Can J Anesth 49: 91-95.
- Friedman PG, Rosenberg MK, Lebenbom-Mansour M (1997) A comparison of light wand and suspension laryngoscopic intubation techniques in outpatients. Anesth Analg 85: 578-582.
- Hung OR, Pytka S, Morris I, Murphy M, Launcelott G, et al. (1995) Clinical trial of a new lightwand device (Trachlight) to intubate the trachea. Anesthesiology 83: 509-514.
- Park SH, Park HP, Jeon YT, Hwang JW, Kim JH, et al. (2010) A comparison of direct laryngoscopic view depending pillow height. J Anesth 24: 526-530.
- Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, et al. (1985) A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J 32: 429-434.
- Samsoon GLT, Young JR (1987) Difficult tracheal intubation: a retrospective study. Anaesthesia 42: 487-490.
- Manabe Y, Seto M, Iwamoto S (2011) The Success Rate of Nasotracheal Intubation Using Lightwand Does Not Depend on the Laryngoscopic View. J Anesth 25: 350-355.
- Cormack RS, Lehane J (1984) Difficult tracheal intubation in obstetrics. Anaesthesia 39: 1105-1111.
- Kim YC, Lee SH, Noh GJ, Cho SY, Yeom JH, et al. (2000) Thermosoftening treatment of the nasotracheal tube before intubation can reduce epistaxis and nasal damage. Anesth Analg 91: 698-701.
- Yamamura H, Yamamoto T, Kamiyama M (1959) Device for blind nasal intubation. Anesthesiology 20: 221.
- Inoue Y, Koga K, Shigematsu A (2002) A comparison of two tracheal intubation techniques with TrachlightTM in patients with cervical spine disorders. Anesth Analg 94: 667-671.
- Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT (2013) Practice guidelines for management of the difficult airway : an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 118: 251-270.
- Hung OR, Stewart RD (1995) Lightwand intubation I. A new lightwand device. Can J Anaesth 42: 820-825.
- Cheng KI, Chang MC, Lai T-W, Shen YC, Lu DV, et al. (2009) Modified lightwand-guided nasotracheal intubation technique for oromaxillofacial surgical patients. J Clin Anesth 21: 258-63.
- van Elstraete AC, Pennant JH, Gajraj NM, Victory RA (1993) Tracheal tube cuff inflation as an aid to blind nasotracheal intubation. Br J Anaesth 70: 691-693.
- Fox DJ, Castro T, Rastrelli AJ (1987) Comparison of intubation techniques in the awake patient: the Flexi-lum surgical light (lightwand) versus blind nasal approach. Anesthesiology 66: 69-71.
- Asai T (1996) Endotrol tube for blind nasotracheal intubation. Anaesthesia 51: 507.
- Iseki K, Murakawa M, Tase C, Otsuki M (1999) Use of a modified lightwand for nasal intubation. Anesthesiology 90: 635.
- Locker GJ, Staudinger T, Knapp S, Burgmann H, Laczika KF, et al. (1998) Assessment of the proper depth of endotracheal tube placement with the Trachlight. J Clin Anesth 10: 389-393.
- Ainsworth QP, Howells TH (1989) Transilluminated tracheal intubation. Br J Anaesth 62: 494-497.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 16349
- [From(publication date):
February-2014 - Jul 13, 2025] - Breakdown by view type
- HTML page views : 11641
- PDF downloads : 4708