Appraising the Role of Fine Needle Aspiration Cytology in Non-Thyroidal Head and Neck Masses: A Single Referral Institute Experience.
Received: 03-Jun-2017 / Accepted Date: 19-Jun-2017 / Published Date: 26-Jun-2017 DOI: 10.4172/2161-119X.1000310
Abstract
Background: Fine needle aspiration biopsy (FNAB) is a widely recognized and sensitive technique, in which a fine needle is introduced into a mass, cellular material is aspirated and a cytological diagnosis is made. It provides initial diagnosis for masses in the head and neck region, enables appropriate management plans for individual patients to be made and separates masses that are reactive or inflammatory in origin and do not require surgical intervention, from masses of neoplastic origin. Furthermore, FNAB can differentiate benign from malignant neoplasms. Objective: To study the value of fine needle aspiration biopsy (FNAB) in the diagnosis of palpable non-thyroidal neck masses in Dammam Medical Complex. Study design: Patients with palpable non-thyroidal neck masses, who had their FNAB during the three-year study period, were reviewed. The FNAB results were analyzed into two groups according to the tissue of origin, into lymph node and salivary gland in origins. The study groups were also classified based on the histopathology findings into; inflammatory, congenital and neoplastic. FNAB diagnoses were retrospectively correlated from patient’s file, with available histological findings or with the outcome of treatment. Accuracy, sensitivity and specificity of FNA were analyzed. Results: A total of 258 patients had FNAB during the study Period. All patients who lost follow-up, those who were referred from other hospitals so the full medical records could not be retrieved and those with inadequate FNAB specimens to make the diagnosis were excluded from our study. Out of the 178 FNABs included in our study, 159 FNAB were done in adult patients and only 19 FNAB were carried out in pediatric age group. For the masses from palpable lymph node, the most common diagnoses were reactive/nonspecific lymphadenitis in pediatric (73.7%) and in adult were reactive/nonspecific lymphadenitis and tuberculosis lymphadenitis (50.8% and 32.5%, respectively). The next most common masses were neoplasm (16.7%), of these 45% of the cases were metastatic in origin, while diagnosis of lymphoma made in 55% of the cases. FNA from major salivary glands were 12.6% of the cases, mainly parotid and submandibular gland (65% and 35%, respectively). In our experience, the overall FNA sensitivity was 96.77%, with specificity of 92.1% and accuracy of 95.68%. Conclusion: FNAB of head and neck masses is a simple and cost effective tool in reaching an initial diagnosis and road map the clinician’s management approach. It aids in separating inflammatory non-thyroidal neck masses from neoplastic lesions, enhances surgical planning for malignant diseases and allows rapid referral of lymphomas and cancer cases for a higher center for further management. FNAB carries a high sensitivity and specificity rate with high overall accuracy in both adult and pediatric patients if done by experienced physician and interpreted by experienced histopathologist. The complications of FNAB are negligible and the associated pain and discomfort is short lived and well tolerated by most patients. This advantage encourages the clinician to consider FNAB as first step in approaching non-resolving, non-vascular, non-thyroidal head and neck masses in both adult and pediatric population.
Keywords: Fine needle aspiration biopsy; Lymph node; Patients; Head and neck masses
259318Introduction
Masses in the head and neck region are a common clinical finding and the differential diagnosis of a neck lump covers a broad spectrum of diseases with differing implications for management [1]. Common causes of neck lump include reactive lymphadenopathy, Salivary gland enlargement, thyroid gland masses, congenital cysts and benign neoplasms. However, over one half of asymmetrical neck masses in adults are reported to be malignant, either primary (usually lymphoma) or secondary (usually carcinoma) [2]. Therefore, the accurate diagnosis of the nature of neck swelling is essential for further patient management. The primary diagnosis of neck masses when made by obtaining excision or incision biopsy has been strongly debated [3]. Several series of patients with metastatic carcinoma in cervical lymph nodes have been analyzed in the search for prognostic indicators, most series suggest that open biopsy of metastatic node, advanced age and nodal stage had adverse effect on survival [3]. Others have found that open biopsy is detrimental to clinical management as it makes subsequent examination of the neck more difficult, encourages fungation, increases the risk of subsequent recurrence in the neck and entails an unnecessary admission and general anesthetic for the patient [4,5]. Likewise, open biopsy of parotid gland neoplasm prior to definitive treatment has been reported to lead to an increased risk of tumor implantation of the wound and consequently, an increased rate of local recurrence [6]. For this reason, open biopsy of a neck mass of unknown etiology should not be undertaken until the possibility of carcinoma of salivary gland tumor has been excluded.
Fine-needle aspiration biopsy (FNAB) is simple, non-invasive and currently widely acceptable as initial diagnostic tool for neck masses, benign or malignant, even those of non-thyroidal origin. Using 22 to 27 gauge needles, FNAB provides sample for cytological examination, with possible cell block preparation. It requires a skilled aspirator along with the routine use of syringes, needles and stains. Moreover, FNAB is a very safe technique with negligible complications [6,7]. In most instances and specifically for palpable lesions, FNAB does not need major pre-procedure preparations and radiology guidance, so it can be performed in the clinic without reserving a place in the radiology unit or operating rooms.
FNAB has the following advantages over open biopsy; FNAB avoids the need for general anesthesia with operating room booking, it decreases open biopsy-related morbidity, as well as FNAB leads to more accurate open surgical planning if needed [2]. Despite of this, FNAB in non-thyroidal neck masses has gained growing acceptance in recent years as minimally-invasive procedure in tertiary care facilities, but still some clinicians are hesitant to proceed with FNAB due to the following reasons; the procedure is operator dependent and required expert cytopathologist. In addition to that, general anesthesia is needed to accomplish FNAB in selected cases and in case of un-experienced surgeon, thus mitigating one of the main advantages of this technique. Even in the presence of a benign cytological result, patients and their family concerns and pressure regarding persistence of a benign lymph node can still eventually prompt an open biopsy [2]. Complications of FNAB are rare and it causes minimal distortion of lymph node architecture and so interferes minimally with subsequent histological examination of excised lymph node [8].
The aim of our current study was to:
• To evaluate the value of FNAB in non-thyroidal palpable neck masses in both adults and pediatric patient. This study was carried out in a single institute, Dammam Medical Complex (DMC), Saudi Arabia, which is advance secondary referral hospital.
• To determine FNAB overall sensitivity, specificity and accuracy in non-thyroidal neck masses in our center and to compare results of our study with those in the published literature.
Materials and Methods
We conducted a retrospective, uncontrolled study in Dammam Medical Complex, which is the largest advanced secondary and referral hospital belongs to Ministry of Health, Eastern province of Saudi Arabia. The study was span over a three years’ period. The data was collected from the IT department, from the histopathology pre-registered electronic database and from the patient charts. The cases that included in this analysis were all patients referred to the histopathology department for Fine needle aspiration from all over DMC’s different departments, as well as from other hospitals within DMC territories, which referred patients to DMC, such as Dammam Maternity and Children’s Hospital. FABC cases who lost follow up, cases with inadequate histopathology specimens and those whom their medical records could not be retrieved were excluded from the study.
All our patients had an office-based FNAB. Subcutaneous injection of local anesthesia was not used as FNAB was done using small gauge needle thus avoiding additional needle prick. During the procedure, the palpable neck mass was identified and stabilized by digital palpation. The overlying skin was cleaned with an alcohol swab, then a 25 gauge needle attached to a 10 ml syringe was inserted into the mass transcutaneous. Multiple rapid, short excursions with suction applied to the syringe, were made within the mass and the needle was withdrawn from the patient after the suction being released. The aspirated material was then expelled onto glass slides and direct smears were made. Using simple descriptive statistics, the following variables were collected and they included demographic data, complications, cytopathological results, need for further open procedures and comparison between the final biopsy results with FNA results and overall clinical outcomes.
Results
Over three years-period, a total of 258 patients, who had palpable non-thyroidal neck masses and underwent FNABs in DMC. The records of 258 patients were reviewed, inadequate specimen which was encountered in about 41 cases (16%), which was mainly related to the surgeon experience, 19 patients (7.36%) were referred from other hospitals, so their medical records could not be traced and 20 patients (7.75%) lost follow-up and were also excluded from our study. After excluding those case, total of 178 FNABs were included in our study. 159 adults (89.1%) and only 19 patients (11.9%) were pediatric under the age of 18 years.
In the pediatric cases, which was only 19 FNABs, 9 patients (47.4%) were male, while 10 (52.6%) were female. The materials aspirated were from 13 enlarged lymph nodes and 3 FNABs from enlarged salivary glands. The diagnosis was benign reactive hyperplasia in 73.7% of cases (Table 1). The patients were eventually improved clinically with treatment and the lump disappeared. While in masses of salivary origin (Table 2), Sialoadenitis was the most prevalent histological diagnosis in two third of the cases, while in one third of the cases; benign neoplasms were seen in FNABs.
| Definitive Diagnosis | Number | Percentage |
|---|---|---|
| Reactive lymphadenitis | 14 | 87.5% |
| Congenital cyst | 1 | 6.25% |
| Lipoma | 1 | 6.25% |
| Total | 16 | 100% |
Table 1: Number and percentage of Paediatric FNABs from lymph nodes and definitive diagnosis.
| Definitive Diagnosis | Number | Percentage |
|---|---|---|
| Silaoadenitis | 2 | 66.66% |
| Benign neoplasm | 1 | 33.33% |
| Total | 3 | 100% |
Table 2: Number and percentage of pediatric FNABs from major salivary glands and definitive diagnosis.
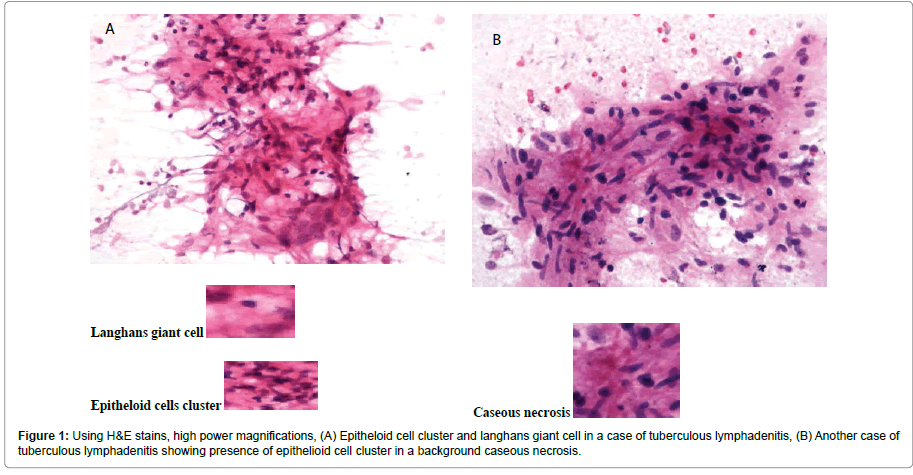
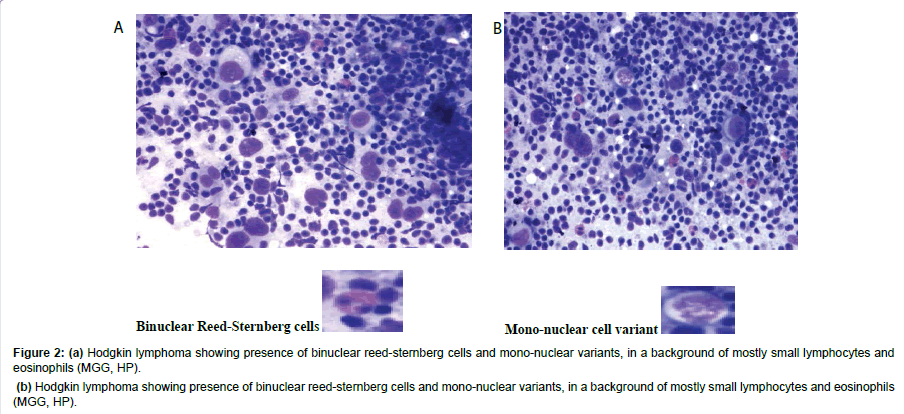
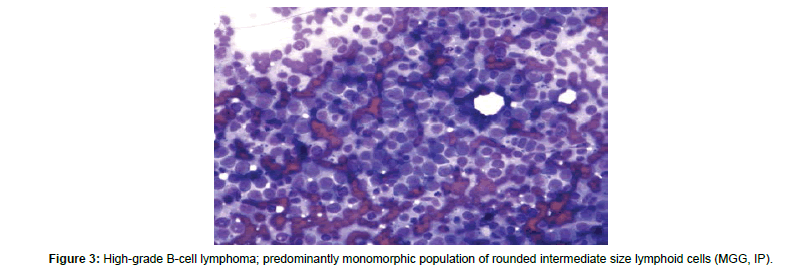
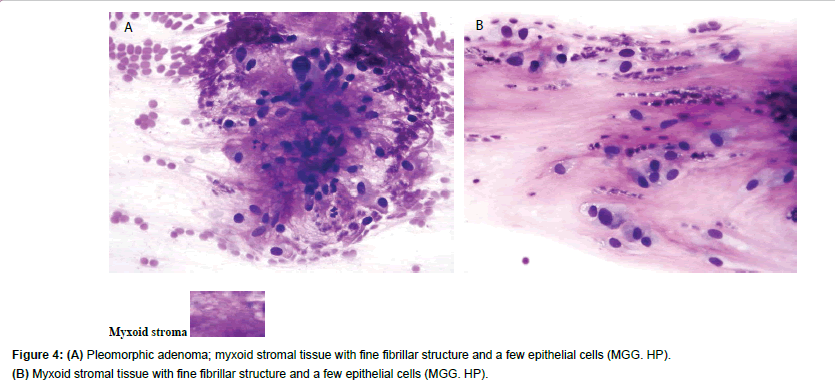
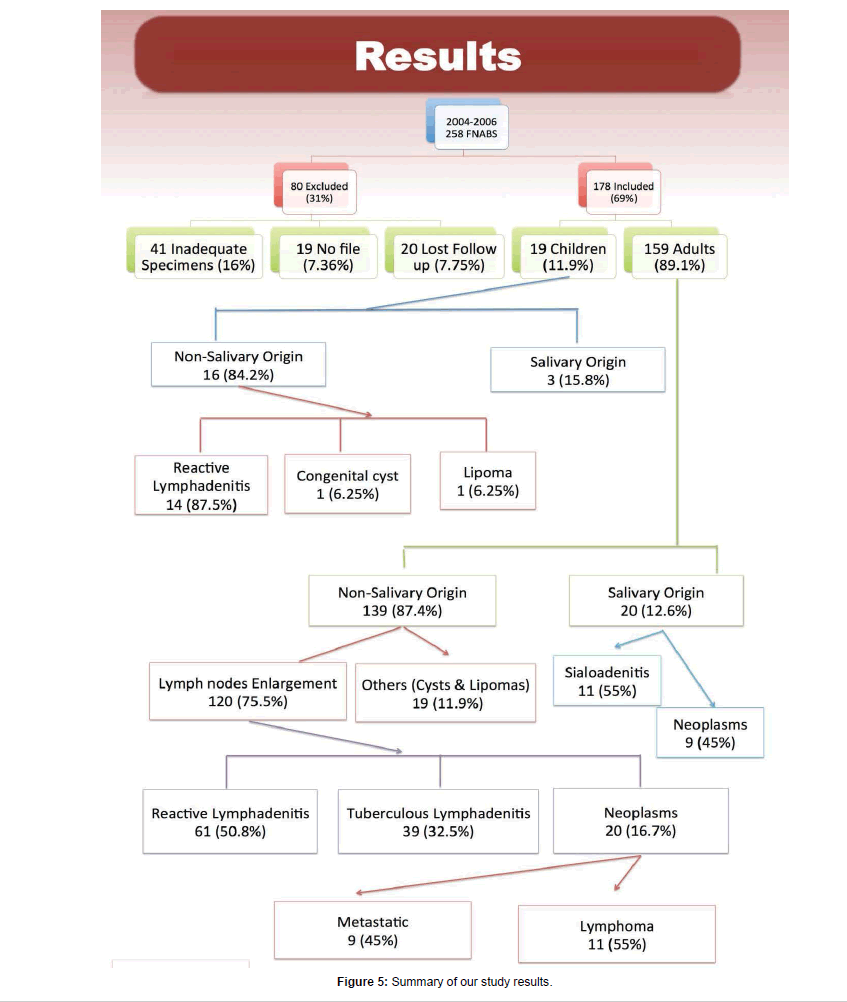
In adult case, a total of 159 FNABs were done, about 89.1%, of the total group studied. Our results showed almost equal gender with 70 (44%) of our cases were male and 89 (56%) were female. The patient’s age ranges between 19 years to 90 years, with the majority of patients were young from 19 to 30 years of age (40.9%) and patients older than 61 years of age were seen in 8.2% (Table 3). For the purpose of simplifying the analysis, the FNABs study group were divided into two major subgroups, First, FNABs from non-salivary masses origin, mainly those from lymph nodes enlargement in 120 cases (75.5%) and second is FNABs group from salivary glands enlargement and seen in 20 cases (12.6%). Few isolated cases such as congenital cysts which were seen in 0.0126% of the cases and lipoma cases which were diagnosed based on mature adipose tissues and seen in 0.063% of cases. In the lymph nodes group (Table 4), half of the cases (50.8%) found to be of acute reactive inflammatory in origin, while in almost one third of the cases (32.5%), tuberculosis lymphadenitis. The FNABs features of tuberculosis lymphadenitis include epitheloid cell cluster and Langerhans giant cell (Figure 1A) and presence of epitheloid cell cluster in background caseous necrosis (Figure 1B). Neoplastic lesions were seen in 20 cases (16.7%). 9 cases had FNABs showed neoplasm of metastatic origin (45%), commonest of which was of unknown origin. 11 cases of the studied FNABs (55%) were diagnosed as lymphoma, with majority of the cases (7 cases, 63.3%) were of Hodgkin’s lymphoma. Hodgkin’s lymphoma FNABs features include presence of binuclear Reed-Sternberg cells and mononuclear cells, in a background of mostly small lymphocytes and eosinophils (Figures 2A and 2B). 5 cases (71.4%) were of nodular sclerosis type of lymphomas with predominantly monomorphic population of rounded intermediate size lymphoid cells (Figure 3). 20 FNABs were from masses originated from major salivary gland origin (Table 5), of which 13 were from the parotid gland (65%) and 7 were from the submandibular gland (35%), the diagnosis of sialoadenitis were established in 53.8% in patients with parotid masses and 57.1% in patients with submandibular masses, while benign neoplasms were seen in 9 FNABs (45%), with almost equal percentage in both parotid and submandibular glands, 46.2% and 42.9%, respectively. The most common in the parotid gland masses was pleomorphic adenoma with histopathological features of myxoid stromal tissue and fine fibrillar structure and few epitheloid cells (Figures 4A and 4B). Overall results of our study in DMC experience with FNABs showed sensitivity of 96.8% and specificity of 92.1%, with overall FNABs accuracy of 95.7% (Table 6). Figure 5 summarized our study results, highlighting the results in both pediatric and adult patients group and in every group, the studied group were further divided into salivary and non-salivary masses groups.
| Age Group | # and % of patients | Male | Female |
|---|---|---|---|
| 19-30 years | 65 (40.9%) | 25 (35.7%) | 40 (45%) |
| 31-40 years | 40 (25.2%) | 19 (27.1%) | 21 (23.6%) |
| 41-50 years | 28 (17.5%) | 11 (15.7%) | 17 (19.1%) |
| 51-60 years | 13 (8.2%) | 7 (10%) | 6 (6.7%) |
| >61 years | 13 (8.2%) | 8 (11.5%) | 5 (5.6%) |
| Total | 159 (100%) | 70 (44%) | 89 (56%) |
Table 3: Number and percentage of patients, their age group distribution and gender.
| Definitive diagnosis | # and % of FNABs |
|---|---|
| Acute reactive lymphadenitis | 61 (50.8%) |
| Tuberculosis | 39 (32.5%) |
| Neoplasm | 20 (16.7%) |
| Metastatic | 9 (45%) |
| Lymphoma | 11 (55%) |
| Total | 120 (75.5%) |
Table 4: Adult FNABs Definitive diagnosis, in masses originating from lymph nodes.
Figure 2: (a) Hodgkin lymphoma showing presence of binuclear reed-sternberg cells and mono-nuclear variants, in a background of mostly small lymphocytes and eosinophils (MGG, HP).
(b) Hodgkin lymphoma showing presence of binuclear reed-sternberg cells and mono-nuclear variants, in a background of mostly small lymphocytes and eosinophils (MGG, HP).
| Definitive Diagnosis | From Parotid Gland | From Submandibular Gland | Total |
|---|---|---|---|
| Silaoadenitis | 7 (53.8%) | 4 (57.1%) | 11 (55%) |
| Benign Neoplasm | 6 (46.2%) | 3 (42.9%) | 9 (45%) |
| Total | 13 (65%) | 7 (35%) | 20 (100%) |
Table 5: Adult FNABs from masses originating from salivary glands.
| Disease | No Disease | ||
|---|---|---|---|
| Positive Test | 120 | 3 | PPV=97.6% |
| Negative Test | 4 | 35 | NPV=89.7% |
| Sensitivity 96.8% |
Specificity 92.1% |
Accuracy: 95.7% |
Table 6: 2 X 2 tables summarizing the overall results of FNABs.
Discussion
The use of needle aspiration for purposes of diagnosis can be traced back to 1847, when Kun described a “new instrument for the diagnosis of tumours” [9]. This was followed by occasional sporadic reports of this technique towards the end of 19th century. In 1883, Leydon used needle aspiration to obtain cells to isolate pneumatic microorganisms. Three years later, Menetrier used the technique to diagnose pulmonary carcinoma. One of the first reported needle aspirations has been traced to the mid-1880s [10]. In the United Kingdom, in 1927, Dudgeon and Patrick proposed needle aspiration of tumors as a means of rapid microscopic diagnosis [11]. This idea was taken on with full avidity in the early 1930s, by Hayes E Martin, a head and neck surgeon and Edward B Ellis, a chief histotechnologist at New York’s Memorial Hospital for Cancer and Allied Diseases (the present Memorial Sloan- Kettering Cancer Center) [10]. Much of the credit for their success deservedly goes to Stewart, the surgical pathologist responsible for interpreting the smears. In 1933, Stewart described the experience of the Memorial Hospital comprising 2500 tumors analyzed by the aspiration method [11]. Since then, the role of diagnostic cytology has expanded tremendously. The availability of a variety of rapid, safe and cost-effective techniques and stains often places cytopathology in the forefront of diagnostic evaluations for masses all over the body and moreover, in the head and neck region.
Fine needle aspiration biopsy (FNAB) is the study of cells aspirated from a mass using a small gauge needle. Its main advantages are that it is minimally invasive, has virtually no contraindications and does not violate the neck, so allowing the early diagnosis of a neck mass without risking seeding of malignant cells [12,13]. Fine needle aspiration and biopsy are typically indicated when no cause for persistent neck mass is found on the initial evaluation. It is recommended as a first line of investigation in palpable head and neck masses. Accuracy of FNAB is dependent on obtaining an adequate specimen for examination by the cytopathologist. In our study 16% of all aspirates were considered inadequate, as compared to the literature, it can reach nearly one fifth of aspirates [1]. The presence of cytopathologist at the time that the procedure is being performed is considered to enhance the likelihood of obtaining an adequate specimen [12]. When the sample obtained by FNAB is reported as being inadequate, then a repeated aspiration should be performed.
In adults, the use of FNAB is considered the gold standard of care in the diagnosis of masses in head and neck and other body sites. The diagnostic accuracy of FNAB in differentiating malignant and benign lesions, as we found a Sensitivity of 96.8% and a Specificity of 92.1%, with overall accuracy of 95.7%. Similar studies reported Sensitivity between 82.14% and 95% and a Specificity of 62.7% to 100%, with FNAB overall accuracy ranges from 80 to 97% [14-22], thus our results were in line with those found in the published English literatures. The accuracy is dependent on operator experience as in one study can reach 100% when performed by a consultant and 91% when performed by junior staff, thus the greater experience of the operator appears to improve the accuracy rate [23]. However, in our current study, we did not address the effect of performer experience or level on the accuracy of FNAB.
American physicians have been reluctant to adopt its use for children; however, even though it is generally accepted approach for approaching an atypical course of what otherwise appears to be a common childhood condition ‒ especially a persistent, unexplained or growing mass ‒ should receive prompt evaluation. Many physicians believe that a highly suspicious mass may require surgical excision despite FNAB and that therefore FNAB is redundant and unwarranted, as shown by many studies [24]. FNAB was able to obviate surgical intervention and to allow treatment to be initiated immediately in many patients. Even in those in whom operation was still required, preoperative FNAB eliminate the anxiety before and during the operation because the clinician could inform the patient and family of the probable diagnosis before the operation and discuss treatment options fully, Thus the surgeon could plan definitive surgical approach and avoid a frozen section or two-stage procedure.
Clinicians may be reluctant to use FNAB in cases in which the clinical suspicion of malignancy is low, fearing that the procedure is too traumatic and usually prefer to observe the patient clinically [25]. As this study was carried out in hospital mainly dealing with adult cases and there is a separate children hospital in the same area in our study, the number of pediatric cases was too small. Only 11.9%, in comparison to the total number of FNAB. Therefore, no definitive results can be obtained, but based on our limited experience, FNAB procedure in children was safe with no complications such as tumor spread along the needle tract or infectious complications were almost non-existent [24].
The lesions arising from the lymph node is found in patients across different ages, ranging from early to advanced age [26]. In our study, youngest patient encountered was 3 year old and the eldest was 90 years of age. In one of the largest studies in literatures, a study of 864 and 1.103 patients showed that inflammatory lymphadenopathy which is typically self-limited and resolves spontaneously over weeks. Cervical adenitis is probably the most common cause of an inflammatory mass in the neck as seen in our study in about 50% of the cases. Tubercular lymphadenopathy was found in 39 cases (32.5%) and this finding was in concordance with others [26]. This observation was slightly higher than that given by Wilkinson et al. [19], who noted a percentage of 27.3% in 783 cases analyzed during his study. This discrepancy could be due to failed anti-tubercular therapy or resistant strains of mycobacterium. However, few authors have reported a higher incidence of tubercular lymphadenopathy as 77.0%, 65.3% and 62.5%, respectively [27]. Neoplasm in the lymph node found in our study in 20 cases (16.7%), of these, in 55% of the cases, malignant lymphomas diagnosed and this higher than the reported studies (20%) [16], probably due to the small number on that study (6 cases only).
Interpretation of FNAC from the salivary glands is, however, a difficult cytopathological technique with many problems and pitfalls [28]. Although some of these problems are similar to those encountered in the interpretation of other histological material18 and are due to the varied and heterogeneous nature of salivary gland neoplasia, other dilemmas are inherent to FNAC-namely, uncertainty as to the site and tissues actually aspirated, minimal material and the lack of architectural pattern in smears compared with histological sections [29].
Conclusion
Neck mass is very common presenting symptom to otolaryngologist, general surgeon and family physician. It can affect any age group starting from early childhood to elderly. Evaluation of these patients is crucial in order to reach definitive diagnosis, to avoid unnecessary surgical intervention and facilitate the patient’s referral to higher centers if needed. The proper evaluation of affected patient started with careful history taking, proper and thorough physical examination, followed by pathological diagnosis. Fine needle aspiration biopsy is an excellent first line method of investigation in any persistent neck lump, FNAB of palpable head and neck masses is a simple, cost effective and yet very effective diagnostic tool in separating inflammatory from neoplastic lesions. A high index of suspicion should be maintained in any high risk patients, on the basis of age, smoking and other clinical symptoms (hoarseness, dysphagia, otolagia, non-healing ulcers, or weight loss), In such cases, repeating FNAB reduces the likely hood of missing cancer, especially in initially inadequate FNAB samples. In our study, the accuracy of FNAB is 95.68%, with high sensitivity and specificity, appraise the role of FNAB in initial work up for any persistent non-thyroidal, non-vascular masses.
References
- Sheahan P, Fitzgibbon J, O'Leary G, Lee G (2004) Efficacy and pitfalls of fine needle aspiration in the diagnosis of neck masses. Surgeon 2: 152-156.
- Slaughter DP, Majarakis JD, Southwick HW (1956) Clinical evaluation of swellings in the neck. Surg Clin North Am 36: 3-9.
- Gleeson M, Herbert A, Richards A (2000) Management of lateral neck masses in adults. BMJ 320: 1521-1524.
- Gooder P, Palmer M (1984) Cervical lymph node biopsy--a study of its morbidity. J Laryngol Otol 98: 1031-1040.
- McGuirt WF, McCabe BF (1978) Significance of node biopsy before definitive treatment of carcinoma. Laryngoscope 88: 594-597.
- Simsir A, Rapkiewicz A, Cangiarella J (2009) Current utilization of breast FNA in a cytology practice. Diagn Cytopathol 37: 140-142.
- Manfrin E, Mariotto R, Remo A, Reghellin D, et al. (2008) Is there still a role for fine-needle aspiration cytology in breast cancer screening? Experience of the Verona mammographic breast cancer screening program with real-time integrated radiopathologic activity (1999-2004). Cancer 114: 74- 82.
- Patt BS, Schaefer SD, Vuitch F (1993) Role of fine-needle aspiration in the evaluation of neck masses. Med Clin North Am 77: 611-623.
- Ansari NA, Derias NW (1997) Fine needle aspiration cytology. J Clin Pathol 50: 541-543.
- Webb AJ (1974) Through a glass darkly. (The development of needle aspiration biopsy). Bristol Med Chir J 89: 59-68.
- Dudgeon LS, Patrick CV (1927) A new method for the rapid microscopical diagnosis of tumours. Br J Surg 15: 250-261.
- Amedee RG, Dhurandhar NR (2001) Fine-needle aspiration biopsy. Laryngoscope 111: 1551-1557.
- Frable WJ, Frable MA (1974) Thin-needle aspiration biopsy in the diagnosis of head and neck tumours. Laryngoscope 84: 1069-1077.
- Soni S, Pippal SK, Yashveer B, Srivastava P (2010) Efficacy of fine needle aspiration cytology in diagnosis of neck masses. World Articles in Ear, Nose and Throat 3: 1.
- Akhavan-Moghadam J, Afaaghi M, Maleki AR, Saburi A (2013) Fine needle aspiration: An atraumatic method to diagnose head and neck masses. Trauma Mon 18: 117-121.
- Palestini N, Papotti M, Sapino A (1994) Fine-needle aspiration biopsy of the thyroid: Review of a 7 year experience. Int J Surg Pathol 1: 171-175.
- Manjula K, Prasad CSBR, Gayathri BN, et al. (2011) Cytomorphological study of lateral neck swellings. J Clin Diagn Res 5: 1016-1019.
- El Hag IA, Chiedozi LC, al Reyees FA (2003) Fine needle aspiration cytology of head and neck masses. Seven years’ experience in a secondary? Care hospital. Acta Cytol 47: 387-392.
- Wilkinson AR, Mahore SD, Maimoon SA (2012) FNAC in the diagnosis of lymph node malignancies: A simple and sensitive tool. Indian J Med Paediatr Oncol 33: 21-24.
- Anne S, Teot LA, Mandell DL (2008) Fine needle aspiration biopsy: Role in diagnosis of pediatric head and neck masses. Int J Pediatr Otorhinolaryngol 72: 1547-1553.
- Addams-Williams J, Watkins D, Owen S, Williams N, Fielder C (2009) Non-thyroid neck lumps: Appraisal of the role of fine needle aspiration cytology. Eur Arch Otorhinolaryngol 266: 411-415.
- Hafez NH, Tahoun NS (2011) Reliability of fine needle aspiration cytology (FNAC) as a diagnostic tool in cases of cervical lymphadenopathy. J Egypt Natl Canc Inst 23: 105-114.
- Martin HE, Ellis EB (1930) Biopsy by needle puncture and aspiration. Ann Surg 92: 169-181.
- Stewart FW (1933) The diagnosis of tumors by aspiration. Am J Pathol 9: 801-812.
- Liu ES, Bernstein JM, Sculerati N, Wu HC (2001) Fine needle aspiration biopsy of pediatric head and neck masses. Int J Pediatr Otorhinolaryngol 60: 135-140.
- Jandu M, Webster K (1999) The role of operator experience in fine needle aspiration cytology of head and neck masses. Int J Oral Maxillofac Surg 28: 441-444.
- Steel BL, Shwartz MR, Ibrahim R (1995) Fine needle aspiration biopsy in the diagnosis of lymphadenopathy in 1.103 patients. Acta Cytol 38: 76-81.
- Young JA (1994) Diagnostic problems in fine needle aspiration cytopathology of the salivary glands. J Clin Pathol 47: 193-198.
- Eveson JW1 (1992) Troublesome tumours 2: Borderline tumours of salivary glands. J Clin Pathol 45: 369-377.
Citation: Al-Qudehy ZA, Al-Mommen A, Al-Nufaily Y, Butt S (2017) Appraising the Role of Fine Needle Aspiration Cytology in Non-Thyroidal Head and Neck Masses: A Single Referral Institute Experience. Otolaryngol (Sunnyvale) 7:310. DOI: 10.4172/2161-119X.1000310
Copyright: © 2017 Al-Qudehy ZA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4221
- [From(publication date): 0-2017 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 3410
- PDF downloads: 811