Application of Skin Stretching Technique for Closure of Large Surface Skin Defects
Received: 24-Jun-2017 / Accepted Date: 09-Aug-2017 / Published Date: 16-Aug-2017 DOI: 10.4172/2161-119X.1000316
Abstract
Closure of large defects skin surface after extensive burns remains an important issue in plastic and reconstructive surgery. Deficit of intact skin dictates a careful and creative approach to surfaces of normal skin. Skin stretching technique using tissue expansion device is a promising approach to treat the little patients with large skin defects. The goal of this approach is to form a full-thickness skin flap of a desired size in cases where skin surfaces, typical for taking a graft, are limited in area or damaged. The resulting skin graft, obtained by our method, could be used on various body parts. We have treated 25 patients with large defects of skin surface using skin stretching technique. 24 patients had burn trauma and one child had a trauma related to a car accident. All patients had cicatricial deformations and various degrees of contractures, which were associated with significant limitations in their everyday life. Using skin stretching devices we were able to get full-thickness skin grafts ranging to 300 sq cm. Scar deformations and contractures were corrected in all patients. Skin stretching technique has been proven to be a useful method in treating large surface skin defects in pediatric patients with various burns, cicatricial contractures, other traumatic causes of skin defects. Skin stretching technique allows receiving a full-thickness skin graft of a desired size similar to normal skin. This method solves a problem of lack of skin graft for closure of large wound areas.
Keywords: Tissue expansion; Post-burn scars in children; Fullthickness skin graft; Burns in children; Cicatricial deformations
255468Introduction
Treatment of children with extensive defects of soft tissues is one of the most important and actual problems of traumatology, reconstructive surgery and oncology [1,2]. The closure of a wound and postoperative defect are not the only objectives pursued by surgeons, which follow modern trends in the treatment of such patients. Particular attention should be paid to the quality characteristics of the restored soft tissues, because a growing child is advisable to perform such reconstructive operations, which from the first surgery can provide the best functional result [3,4].
Full-thickness skin grafts can provide a quality long-term cosmetic and functional result. Essential disadvantages of operations involving the taking of full-thickness skin graft are limited opportunities of surfaces of healthy skin, especially in little children [5]. Practice shows, that the use of split skin for the closure of soft tissue defects leads to an improvement only for a short period of time [6]. The only advantage of a split skin graft is the reusable of donor areas of skin on the surface of the child’s body.
Since the early 1980s, the method of tissue expansion has been actively used in reconstructive and plastic surgery. Many years of experience in the use of tissue expanders led the surgeons to conclusions about the possibility of combining tissue expansion with other methods used to obtain skin grafts. For example, different relocated flaps [7], Filatov’s stem, a musculocutaneous graft on the vascular pedicle and transplantation of skin-fat flaps with the creation of vascular anastomoses [8-11]. The preliminary stretching by the expander of the skin area before taking a full-thickness skin flap is a modern technique, indispensable in the arsenal of surgeons involved in the treatment of the consequences of skin trauma.
The use of endoscopy in the implantation of the expander reduces the likelihood of complications such as bleeding in the postoperative period, and also allows to conduct tissue expansion immediately after implantation of the balloon dilator [12,13].
Materials and Methods
The treatment was carried out in the department of reconstructive surgery, as well as 3th surgical (burn injuries) department of Speransky Children’s Hospital in 2009-2017.
25 children was operated with using of a full-thickness stretched skin graft, of them one girl was operated twice. Most patients (23) received treatment for the consequences of burn injury (post-burn scars). One child we made dermal transplantation in acute period of burn injury, one–in acute period of skeletal trauma in connection with post-traumatic loss of soft tissues. In another case, we used a skin graft to reconstruct the shank stump. The distribution of children by age was as follows: from 1 to 3 years-3 children, from 3 to 7 years-7 children, from 7 to 12 years-10 children, from 12 to 18 years-5 children.
All children who received treatment for the consequences of burn injury in the acute period had a percentage of burns from 40 to 80.
Distribution by sex: boys-10, girls-15.
Indications for implantation of expanders for taking free fullthickness stretched skin graft were based on the following criteria:
1. Extensive defects of the skin (deficit of donor sites)
2. The necessity to address multiple reconstructive tasks simultaneously (for example, eliminating of multiple cicatricial contractures),
3. Remoteness of the scar area from the area of normal skin
4. Need of taking free full-thickness skin a large size (up to 300 sq cm).
The most convenient localizations for implantation of tissue expanders were anterior and posterior region of the thorax
Out of 25 children operated with our method, 13 patients had complaints about cosmetic problems at admission, 12 patients had mostly functional complaints.
In 7 patients, the obtained full-thickness graft was used to solve problems of several localizations (for example, a graft taken from the thorax was used to eliminate extensor contractures of the brushes of both hands. We used latex expanders only, with an internal port of introduction, an oval shape, varying in volume. The introduction was carried out 2 times a week. A supervising doctor himself perfomed a fluid infusion into the expander in all patients, including those receiving treatment on an outpatient basis, were. Lasting of expansion process did not exceed 79 days. The minimum period was 22 days.
In a number of cases an active drainage was installed under the expander in the postoperative period. It is a thin silicone tube with a syringe attached to it on the opposite end of the wound, which creates a negative pressure.
In all cases, excision of the skin over the expander was using the “Surgitron” radio knife performed, which allows dissecting soft tissues without the risk of damage to the latex tissue expander.
The complications of operations were into two groups divided: related to implantation of the expander and associated with surviving of the graft. In each group, were strategically significant and insignificant problems identified. The significant complications were in two cases. These were suppuration of the expander and necrosis of the graft. Insignificant complications we saw in 10 cases, these were marginal necrosis of grafts.
Results and Discussion
Conducting reconstructive operations using a free full-thickness stretched cutaneous graft has direct indications for children with a deficit of normal skin and extensive soft tissue defects. In the treatment of patients with a scar surface area more than 70% of the entire skin, the use of these operations is the only way to perform reconstructive interventions. This method is also irreplaceable for the elimination of extensive areas of the scar surfaces in patients who do not have areas near the scars that are suitable for implantation of the expander.
The most convenient anatomical area for implantation of the expander is the thoracic region, including its posterior surface (back region). In cases, when we cannot implant expanders into "convenient" areas for expansion in a patients with consequences of extensive burns, other areas may be used for performing tissue expansion, including abdominal skin.
Tissue expansion for obtaining a free skin graft is possible to eliminate extensive wound surfaces in the period of acute trauma (including burn injury), provided that the wound is prepared for transplantation (granulations are present). This surgical intervention allows a qualitative compensation of the skin in such anatomical areas that are vital for the child in a functional and cosmetic sense. Carrying out operations using high-quality full-layer material allows avoiding multi-stage reconstructive interventions in the rehabilitation period, which undoubtedly affects the socialization and quality of life of the child.
The properties of soft tissues of young children (up to 3 years) do not allow for the removal of large-sized skin grafts. Using expanders allows to receive a full-thickness skin grafts up to 250 sq cm in size even in small children, being an important method for such a contingent of patients.
With the complications of the operations performed by our method, which affect the final result of the treatment, we encounter not more often than when carrying out balloon tissue expansion in the classical version and free skin transplantation.
Clinical example 1: a 7 year old girl, was admitted to a routine surgical treatment with the diagnosis: Consequences of burn injury, right shoulder contracture, right elbow joint flexion contracture, contractures and finger syndactyles of both hands, multiple cicatricial deformities of the trunk skin, upper and lower extremities. It is known from the anamnesis, that the child was burned by a flame at the age of 5 years. In the acute period of the injury received treatment at the place of residence.
Due to the presence of numerous scar deformities and deficiency of normal skin, it was decided to implant 3 expanders into the ulnar fossa on the left, back and thorax. The expansion was carried for 79 days out. The volume of expanders was 70, 240 and 220 ml, respectively. During the final operation, 1 expander (in the area of the ulnar fossa on the left) was used to create an excess of skin for a local plastic operation. The stretched skin of 2 other expanders was excised to obtain free grafts that were used to removing the contracture of the right shoulder joint, Right elbow joint, as well as extensor contractures of the brushes of both hands. Postoperative period occurred without clinically significant complications.
As a result, cosmetic and functional problems were eliminated simultaneously in several anatomical areas in a child with extensive scars of the skin.
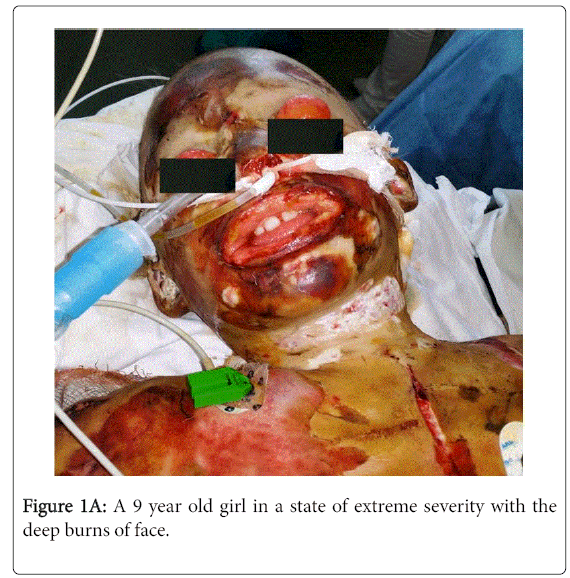
Clinical example 2: A 9 year old girl (Figures 1A-1D) entered the intensive care department in a state of extreme severity with a diagnosis: burns by flame 2-3 degrees of the face, scalp, neck, both upper limbs, hips, stops at S 60%.
In the process of treatment, the child underwent multi-stage surgical interventions. The wounds in face, head and neck remained open.
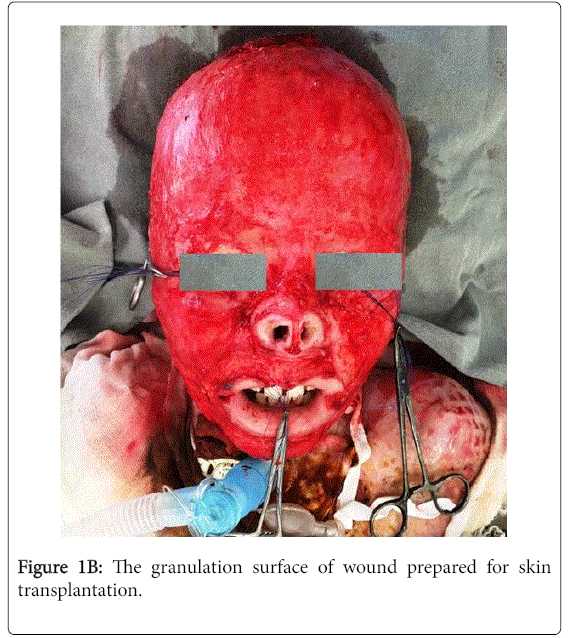
On the right thigh was implanted expander to create a free stretched graft to close wounds in the face and head. During the expander stretching period, preparation of granulation wounds in the face area for skin transplantation was completed.
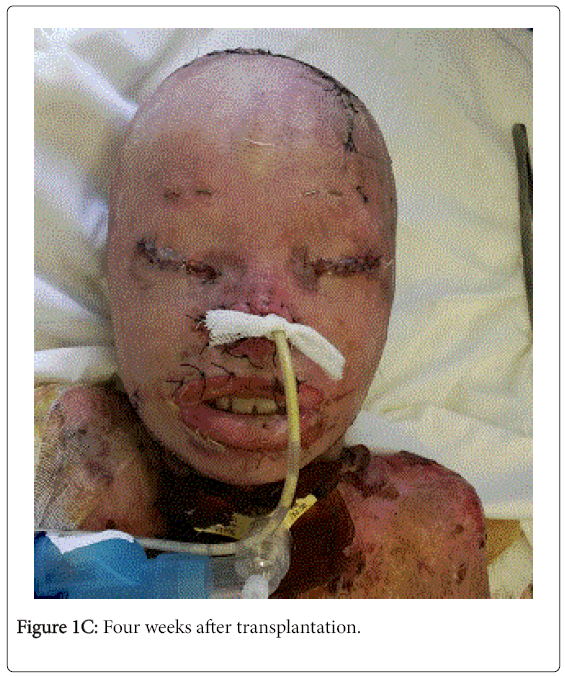
On the 34th day after the implantation of the tissue expander, we made a transplantation of the stretched skin into the face, scalp, and neck area. In the region of the right thigh above the expander, a fullthickness graft measuring 35 × 20 cm was taken and transferred to the wound surfaces of the face, the scalp, and the neck. We have cut out holes for the eyes, nose, ear shells, mouth. The graft was in various areas is partially fixed by an atraumatic suture material. The graft was fixed to the child's head with a self-locking bandage after the application of atraumatic coatings.
The postoperative period proceeded without complications, the full engraftment of the graft was noted.
Conclusion
The method of transplantation of the stretched full-thickness skin graft is an indispensable way of obtaining an excess of quality skin material in children with extensive post-burn scars and large soft tissue defects.
Substitution of defects of soft tissues of the skin with a free fullthickness stretched skin graft is possible not only in children with scars process, but also in the acute period of trauma.
Preliminary stretching of the skin area makes it possible to obtain a one-piece autogram of large sizes without damage to the donor area.
The stretching of healthy skin in patients with a large area of postburn scars allows you to create an excess of material for carrying out reconstructive interventions in several problem areas.
References
- Avdeev AE (1997) Plastic of cicatricial skin lesions by the method of endoexpanding dermotension in children. Abstract of dissertation of candidate of medical Sciences, pp: 4-7.
- Khagurov RA (2011) Application of the method of balloon dermatensia in pediatric reconstructive surgery. Abstract of dissertation of candidate of medical Sciences, pp: 4-5.
- Bogdanov SB, Babichev RG (2016) Face plastic of full-thickness skin grafts in children, Ross. vestnik det. hirurgii, anest. i reanimatologii 6: 86-91.
- Bogdanov SB (2015) The relevance of the substitution of full-thickness skin graft in deep burns of the face in children, Ross. vestnik det. hirurgii, anest. i reanimatologii, App, Proceedings of the congress of pediatric surgeons of Russia, pp: 35-36.
- Congenital giant pigmented nevi in children (2014) Abstract of dissertation of candidate of medical Sciences, pp: 14-15.
- Barkhudarova NR, Burkov IV, Trusov AV, Pronin GP, Fomina MG (2008) New technologies in the treatment of children with consequences of burn injury. Detskaya Hirurgiya 3: 24-27.
- Rivera R, LoGiudice J, Gosain AK (2005) Tissue expansion in pediatric patients. Clin Plast Surg 32: 35-44, viii.
- Zan T, Li H, Gu B, Liu K, Xie F (2013) Surgical treatment of facial soft-tissue deformities in postburn patiens: A proposed classification based on a retrospective study. Plast Reconstr Surg 132: 1001e-10014e.
- Yanko-Arzi R, Gur E, Margulis A, Bickels J, Dadia S, et al. (2014) The role of free tissue transfer in posterior neck reconstruction. J Reconstr Microsurg 30: 305-312.
- Song B, Jin J, Liu Y, Zhu S (2013) Prefabricated expanded free lower abdominal skin flap for cutaneous coverage of a forearm burn wound defect. Aesthetic Plast Surg 37: 956-959.
- Li H, Zhou Y, Du Z, Gu B, Liu K, et al. (2015) Strategies for customized neck reconstruction based on the pre-expanded superficial cervical artery flap. J Plast Reconstr Aesthet Surg 68: 1064-1071.
- Perlovskaya VV (2014) The use of endovideosurgical technology in treatment of children with extensive defects of the skin expander dermotension. Detskaya Hirurgiya 6: 7-10.
- Sharobaro VI, Moroz VY, Starkov YG. Surgical treatment of sequelae of burns with the use of a balloon stretching and endoscopy. Skoraya Med Pomoshch 3: : 254-255.
Citation: Shcherbakova MA, Trusov AV, Rybchenok VV, Fomina MG, Bataev SKhM, et al. (2017) Application of Skin Stretching Technique for Closure of Large Surface Skin Defects. Otolaryngol (Sunnyvale) 7:316. DOI: 10.4172/2161-119X.1000316
Copyright: © 2017 Shcherbakova MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5014
- [From(publication date): 0-2017 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 4193
- PDF downloads: 821