Editorial Open Access
Apical Periodontitis Treatment: Surgical-Non surgical?
Juan Gaston Robledo*
Department of Operative and Prosthodontics, School of Dentistry, University of Buenos Aires, Argentina
- *Corresponding Author:
- Juan Gaston Robledo
Endodontist, Department of
Operative and Prosthodontics
School of Dentistry
University of Buenos Aires, Argentina
Tel: (54) 11 4244 3418
Fax: 951032051
E-mail: jgrobledo@gmail.com
Received Date: October 28, 2013; Accepted Date: November 26, 2013; Published Date: November 28, 2013
Citation: Robledo JG (2013) Apical Periodontitis Treatment: Surgical - Non surgical? J Oral Hyg Health 1:e104. doi: 10.4172/2332-0702.1000e104
Copyright: © 2013 Robledo JG. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Introduction
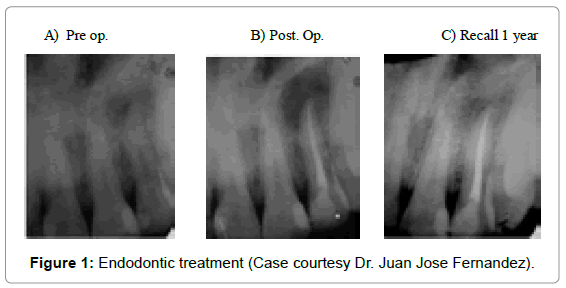
Clinical Endodontics is defined as the prevention and/or elimination of apical periodontitis [1-3]. Epidemiological studies have also shown that post treatment diseases is very common. The high rate of apical injuries is probably caused by deficient root canal treatments. Among these problems we can include: residual infection in inaccessible areas in the apex [4,5]; intraradicular infection [6]; extrusion of dentin remains with prescense of bacteria in dentinal tubules [7]; poor endodontic practices with or without altering the morphology of the root [8-10] canal and root vertical fractures [11-13]. Insufficient treatment of the root canal can be treated without surgery, while other problems may require surgery. Apical surgery offers immediate access to the root apex. The pathology is removed by curettage and section of the apex with frequent infections contained in the ramifications of the canals [5,14]. A full healing of the apical area is possible after the endodontic treatment. However, it has been observed that in some cases the swelling persists (Figure 1).
It is known that when carrying out the cleaning and disinfection of the canal, some biofilms can remain; these have been classified as different types of organized microorganisms included in a matrix [5]. These biofilms were the most common cause of persistence of the swelling and apical periodontitis [15]. They were also mentioned as inducers of chronic canal disease [5]. It is probable that tose bacteria are prsent in dentinal walls [5,16].
Procedures to carry out the root canal treatment, including root access, instrumentation, irrigation, intracanal medication and sealing of the canal are are carried out in an attempt to eradicate the infection from the canal system and eliminate spaces to avoid reinfection.
In infected root canals, the interior dentinal layer, next to the pulp, contains a great number of microorganisms [17,18].
Likewise, in some cases the bacteria have penetrated deeply into dentinal tubules, so much that they cannot be removed mechanically [19-21]. Clearly, there is no technique available capable of removing the entire infected internal dentin layer in a root canal; therefore, the bacteria remain in dentinal tubules after the instrumentation [21].
Since current procedures cannot remove the bacteria, the sealing of the canal can provide two types of solutions:
1- Prevent a new coronary infection
2- Bury remaining bacteria
Most ink penetration tests, have found colorant at least 1 mm from the foramen [22] indicating that there are spaces between the apical filling and the dentinal wall.
It has been proven that these empty spaces allow the movement of bacteria along the sealing of the canal [23-25].
When the root is poorly sealed, inflammatory cells can be found in the residual pulp tissue. If there is extrusion of sealing material outside the limits of the rood apex, there will be swelling in the periapical area. This irritation of sealing material can be the factor causing the inflammatory response [26,27].
Surgical Treatment
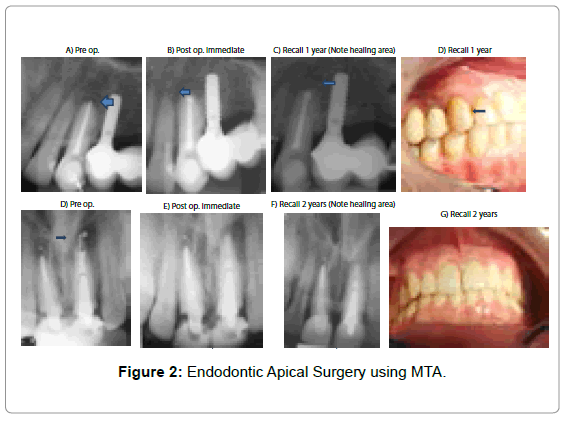
The purpose of this surgery is to clean and seal all communication of the root canal near the apex. Indications for apical surgery usually include cases in which canal obstructions do not allow the checking (retreatment) or those in which it would not be advisable to do so (Figure 2).
The conservation of the natural dental piece is still the main goal. For this, we should evaluate, among other things, the possibility of restoration and return of the function of the dental piece.
It has been demonstrated that after an effective endodontic surgery, 97% of cases show signs of full recovery in the x-rays within 1 year. Some injuries have healed after a 7 month period [14].
Situations in which we would chose the surgical treatment:
--Canals which cannot be treated due to their anatomical complexity.
--Symptomatic tooth or evident injuries due to the lack of previous treatment.
--Failure in previous endodontic treatment atempts (revisions). Fractured instruments which block the light in the canal, making the access to the root apex impossible.
--Extrusion beyond apical limits of any sealing material.
--Long anchored bolts which would be difficult to remove to access the apical area.
Conclusion
Aplical periodontitis may not be detected by x-rays and may persist after many treatments. The firs option to eliminate this pathology is by means of pulp therapy, when this is not enough to solve the problem, endodontic surgery is chosen to solve the situation in order to eliminate the disease.
References
- Orstavik D, Pitt Ford TR (1998) Apical periodontitis: microbial infection and host responses. In: Orstavik D, Pitt Ford TR (Eds.) Essential Endodontology. Blackwell Science, Oxford.
- Friedman S (2002) Considerations and concepts of case selection in the management of post-treatment endodontic disease (treatment failure). Endodontic Topics 1: 54-78.
- Trope M (2003) The vital tooth-its importance in the studyand practice of endodontics. Endodontic Topics 5: 1-11.
- Nair PN, Sjögren U, Figdor D, Sundqvist G (1999) Persistent periapical radiolucencies of root-filled human teeth, failed endodontic treatments, and periapical scars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87: 617-627.
- Nair PN, Henry S, Cano V, Vera J (2005) Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after "one-visit" endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99: 231-252.
- Sundqvist G, Reuterving CO (1980) Isolation of Actinomyces israelii from periapical lesion. J Endod 6: 602-606.
- Yusuf H (1982) The significance of the presence of foreign material periapically as a cause of failure of root treatment. Oral Surg Oral Med Oral Pathol 54: 566-574.
- Ray HA, Trope M (1995) Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J 28: 12-18.
- Tronstad L, Asbjørnsen K, Døving L, Pedersen I, Eriksen HM (2000) Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod Dent Traumatol 16: 218-221.
- Gorni FG, Gagliani MM (2004) The outcome of endodontic retreatment: a 2-yr follow-up. J Endod 30: 1-4.
- Vire DE (1991) Failure of endodontically treated teeth: classification and evaluation. J Endod 17: 338-342.
- Testori T, Badino M, Castagnola M (1993) Vertical root fractures in endodontically treated teeth: a clinical survey of 36 cases. J Endod 19: 87-91.
- Tamse A, Fuss Z, Lustig J, Kaplavi J (1999) An evaluation of endodontically treated vertically fractured teeth. J Endod 25: 506-508.
- Rubinstein RA, Kim S (1999) Short term observation of the results of endodontic surgery with the use of a surgical operation microscope and super-EBA as root-end filling material. J Endod 25: 43-48.
- Costerton JW, Stewart PS, Greenberg EP (1999) Bacterial biofilms: a common cause of persistent infections. Science 284: 1318-1322.
- Tronstad L, Sunde PT (2003) The evolving new understanding of endodontic infections. Endodontic Topics 6, 57-77.
- Valderhaug J (1974) A histologic study of experimentally induced periapical inflammation in primary teeth in monkeys. Int J Oral Surg 3: 111-123.
- Peters LB, Wesselink PR, Buijs JF, van Winkelhoff AJ (2001) Viable bacteria in root dentinal tubules of teeth with apical periodontitis. J Endod 27: 76-81.
- Armitage GC, Ryder MI, Wilcox SE (1983) Cemental changes in teeth with heavily infected root canals. J Endod 9: 127-130.
- Ando N, Hoshino E (1990) Predominant obligate anaerobes invading the deep layers of root canal dentin. Int Endod J 23: 20-27.
- Ricucci D, Langeland K (1998) Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J 31: 394-409.
- Wu MK, Wesselink PR (1993) Endodontic leakage studies reconsidered. Part I. Methodology, application and relevance. Int Endod J 26: 37-43.
- Torabinejad M, Ung B, Kettering JD (1990) In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod 16: 566-569.
- Chailertvanitkul P, Saunders WP, Saunders EM, MacKenzie D (1997) An evaluation of microbial coronal leakage in the restored pulp chamber of root-canal treated multirooted teeth. Int Endod J 30: 318-322.
- Clark-Holke D, Drake D, Walton R, Rivera E, Guthmiller JM (2003) Bacterial penetration through canals of endodontically treated teeth in the presence or absence of the smear layer. J Dent 31: 275-281.
- Brynolf I (1967) A Histological and roentgenological study of periapical region of human incisors. Odontologisk Revy 18: 1-97.
- Bergenholtz G, Lekholm U, Milthon R, Engstrom B (1979) Influence of apical overinstrumentation and overfilling on re-treated root canals. J Endod 5: 310-314.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 24761
- [From(publication date):
December-2013 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 19966
- PDF downloads : 4795