Antimalaria and Anti-Inflammatory Activites New Chloroquine and Primaquine Hybrids Targeting the Blockade of Malaria Parasite Transmission
Received: 01-Sep-2023 / Manuscript No. wjpt-23-112292 / Editor assigned: 04-Sep-2023 / PreQC No. wjpt-23-112292(PQ) / Reviewed: 18-Sep-2023 / QC No. wjpt-23-112292 / Revised: 22-Sep-2023 / Manuscript No. wjpt-23-112292(R) / Accepted Date: 29-Sep-2023 / Published Date: 29-Sep-2023 DOI: 10.4172/wjpt.1000208
Abstract
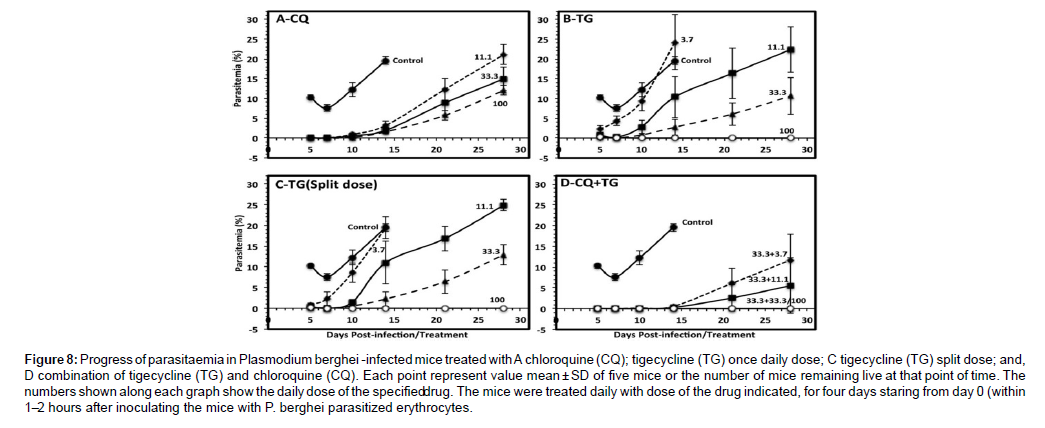
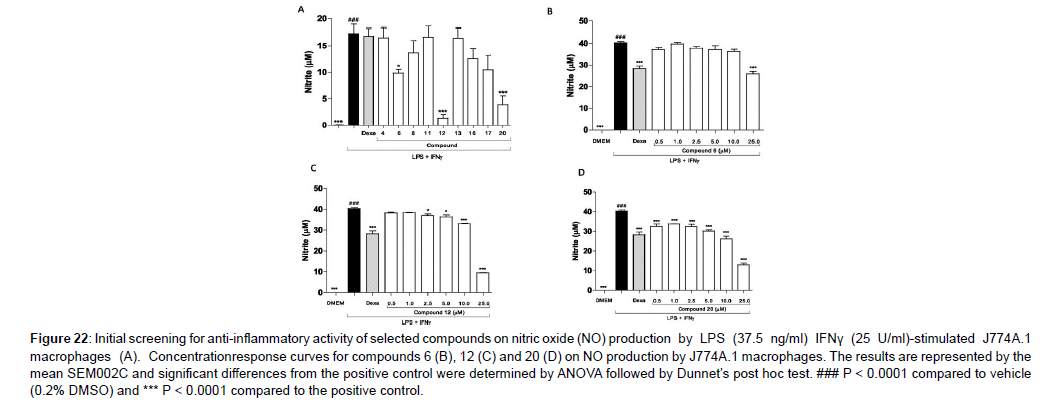
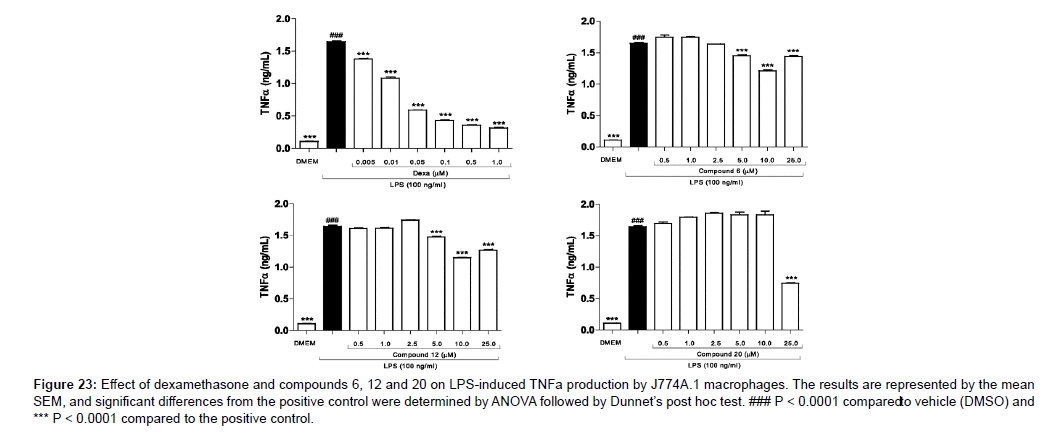
Malaria is a disease that necessitates the development of new treatments not only to combat Plasmodium but also to alleviate infection symptoms such as fever and inflammation. Chloroquine (CQ) and Primaquine (PQ) were coupled to the pharmacophoric group found in phenylacetic anti-inflammatory medicines to create a sequence of 21 hybrid molecules. These chemicals were created with a dual purpose in mind: to kill Plasmodium while also acting on the inflammatory process caused by malaria infection. Nine different biological approaches were used to test the substances. In vitro, the carbonylated CQ derivative was more effective than CQ, reduced parasitemia in P. berghei by up to 37% on day 7. PQ derivative 17 was slightly carbonylated. PQ is less powerful. In mosquitoes, the gem-difluoro PQ derivative showed a high level of transmission blocking of the malaria sporogonic cycle. Compounds 6 and 20 lowered No generation and suppressed TNF production in LPS-stimulated J774A.1 macrophages in a dose-dependent manner. Our findings suggest a plausible and intriguing strategy for developing new chemical entities that operate as transmission-blocking medications for treating malaria caused by Plasmodium falciparum and Plasmodium vivax, as well as the anti-inflammatory mechanism associated with the condition. We introduce a new family of hybrid compounds made up of the anti-plasmodial medicines primaquine and chloroquine. To yet, no treatment has been found to be effective against all phases of Plasmodium’s life cycle. We devised and synthesized a new-generation molecule including both primaquine and chloroquine components from accessible precursors, with the goal of developing medicines with bioactivity against different stages of the parasite’s life cycle. The hybrid molecule 3 has activity against asexual and sexual P. falciparum blood stages, as well as P. berghei sporozoites and liver stages, in vitro. The hybrid is active against P. berghei liver and blood stages in vivo. The concept of using one chemical to combine distinct mechanisms of action that attack different Plasmodium stages in the mammalian host was successfully validated by our findings. It is our hope that the pathogen will be outwitted by the new design of such chemicals in the spread of drug resistance. The chemical is accessible in a smooth and adaptable manner according to the streamlined synthesis process, and it is open to additional molecular modification.
Keywords
Chloroquine; Primaquine; Hybrid molecules; Plasmodium; Multistage; Anti-inflammatory
Introduction
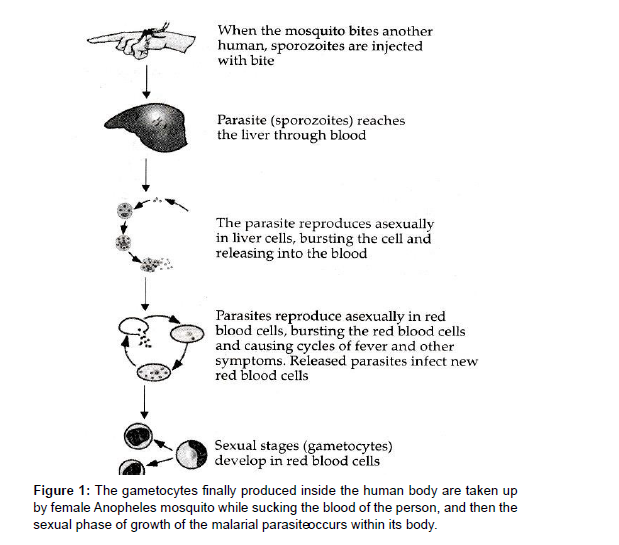
Quinolines are one of the most commonly prescribed malaria medications. Quinine was the first quinoline derivative to be used to treat malaria, followed by synthetic quinoline derivatives including Chloroquine (CQ) and Primaquine (PQ). CQ was the first choice of treatment for malaria since it is one of the safest, most inexpensive, and most effective medications against numerous forms of plasmodia. However, due to abuse, Chloroquine Resistant Strains (CQR) have emerged, rendering it useless in many regions of the world. There is widespread parasite resistance, putting the efficacy of malaria medicine treatments in jeopardy. This resistance is characterized as a delay in parasite elimination after treatment with artemisinin derivatives, which justifies the development of these drugs. Novel antimalarial drug like 8-aminoquinoline PQ and the recently approved Tafenoquine are the only medications approved to treat relapsing P. vivax malaria, and they both act as antimicrobials despite their side effects. The primary purpose of all potential antimalarial medicines is to kill the malaria parasite. The most deadly form of the disease is Cerebral Malaria (CM), which is linked to elevated levels of cytokines and chemokines as mediators of inflammation. P. vivax is the most widely distributed malaria species, accounting for malaria cases in America in 2010, with cases reported in Brazil. Since 1946, Chloroquine has been the welltolerated treatment of choice for acute vivax malaria. The drug relieves fever and parasitemia within 72 hours of the first dose and is rapidly absorbed and slowly eliminated, primarily as the parent drug and as a metabolite of approximately 3: 1 Desethychloroquine [DCQ] in a ratio of about the plasma half-life is about 50 hours and therapeutic levels against vivax malaria persist in the blood until the 21st to 35th day after treatment [1, 2 ]. Due to recurrence of parasitemia via asexual transmission, CQ-resistant P. vivax favor recurrence. After treatment with blood schizontocides, parasites in the blood stage. In an ideal world, determining drug concentrations and their most relevant active metabolites in the blood would confirm in vivo CQ Resistance [CR]. When Australians who immigrated from Papua New Guinea failed to obtain normal treatment, P.vivax CR was discovered. Evidence of the occurrence exists in South America, however there is a scarcity of data. No recurrent parasitemia was detected in certain trials conducted in different locales within 28 days [9 -11] or 30 days after the combined CQ and primaquine PQ therapy failed in P. vivax malaria acquired by Canadian visitors in GUYANA. P. vivax CR has been recorded in three cases in 177 patients in Colombia, resulting in the proper 28-day follow-up of 109 P. vivax patients who were only provided CQ [PQ prescription postponed to 28 days] in 2007. After plasmatic CQ dose to confirm 10.1 percent resistance Although PQ possesses schizonticidal activity against P. vivax, it is commonly utilized as a hypnozoiticidal medication. In vitro evidence of synergy between PQ and CQ against P. falciparum schizonts has been found. For the asexual blood stage of P. vivax, however, there is no indication of synergy between these two medicines. In patients with uncomplicated Vivax malaria, treatment efficacy after 28 days did not differ substantially between the CQ monotherapy group and the group receiving CQ plus PQ for 14 days, according to the available data [3, 4]. These facts, however, solely apply to Asian tribes and cannot be easily generalized to Latin America. The reasoning for extended parasitemia due to treatment resistance explains particularly severe anaemia; nevertheless, no individual individuals have been identified. Because CQ is no longer utilized in most of their locations, P. vivax CR who develop anaemia are well described [5, 6 ]. We measured in vivo CQ resistance in patients with uncomplicated P. vivax from western BRAZIL using CQ [standard dose of 25 mg/kg over the first 3 days estimated first 7 days] and PQ [0.5 mg/kg / Day over the first 3 days estimated first 7 days], as well as the dynamics of haemoglobin levels over the follow-up period in both resistant and sensitive groups. Malaria is a leading source of morbidity and mortality, with antimicrobials in use [ 7 ] and novel antimicrobials being discovered all over the world. The malarial parasite, Plasmodium, requires two hosts to complete its life cycle. In humans, the asexual phase of growth occurs, which can be represented as follows (Figure 1, 2, 3)
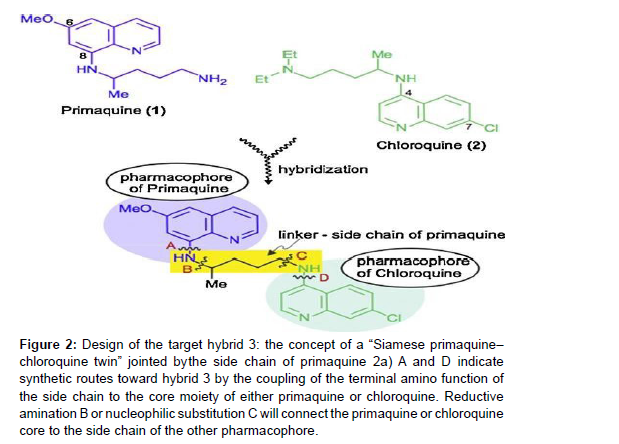
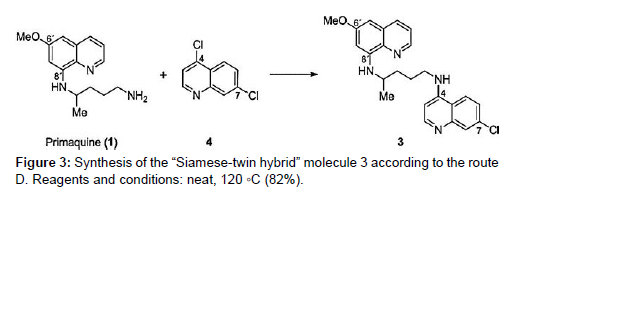
Figure 2:Design of the target hybrid 3: the concept of a “Siamese primaquine–
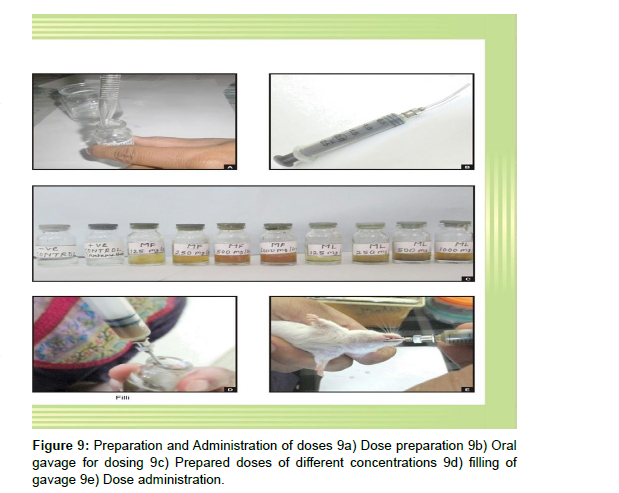
chloroquine twin” jointed by the side chain of primaquine 2a) A and D indicate
synthetic routes toward hybrid 3 by the coupling of the terminal amino function of
the side chain to the core moiety of either primaquine or chloroquine. Reductive
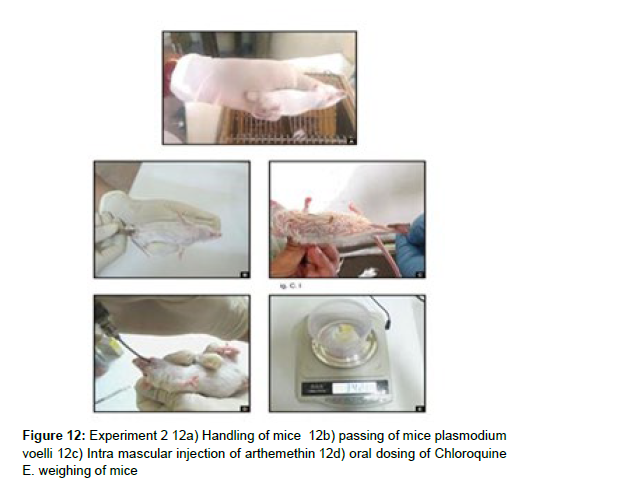
amination B or nucleophilic substitution C will connect the primaquine or chloroquine
core to the side chain of the other pharmacophore.
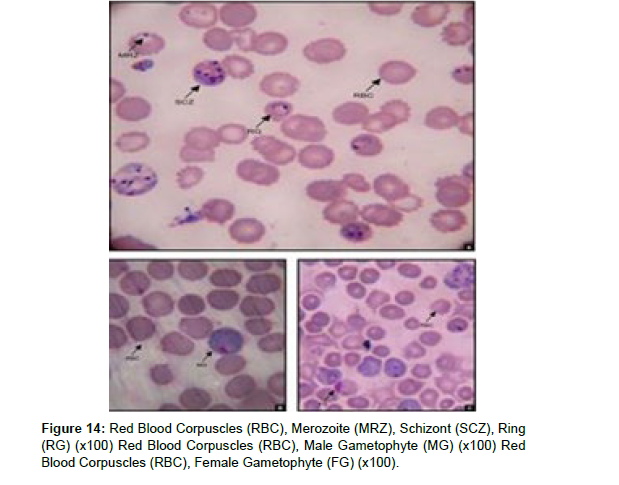
It is a well-tolerated 4-aminoquinoline antimalarial drug that is active against blood schizonts and has been used as a standard therapy for decades. Because of widespread resistance, the effectiveness of Chloroquine has been gradually declining since the early 1990s. At the same time, the official malaria treatment policy was altered to a two-drug combination therapy. There is some evidence, however, that the removal of Chloroquine from the market led in a fall of Chloroquine resistant Plasmodium species due to their reduced fitness relative to wild-type parasites. These findings point to the possibility of reintroducing Chloroquine (2) into malarial combination medication therapy [8 ].
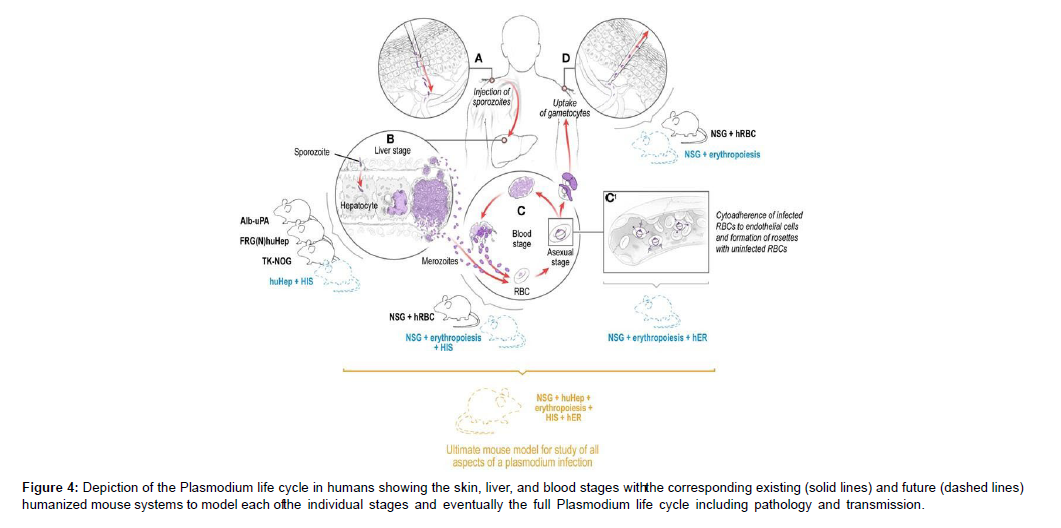
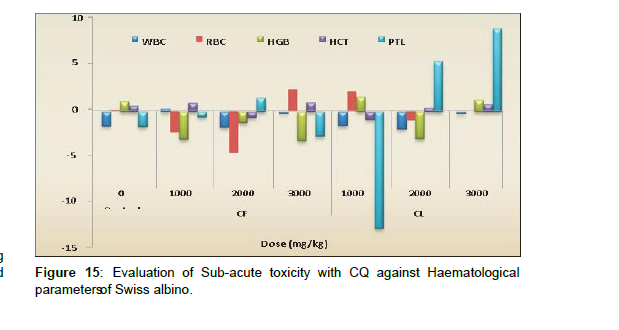
Due to their potential side effects, two additional antimalarial medicines – 8-aminoquinolines pamaquine and primaquine (1) – have been overlooked in recent years. Methemoglobinemia and haemolytic anaemia in patients with glucose-6-phosphate dehydrogenase deficiency. This is unfortunate because primaquine, an 8- aminoquinoline, is effective against liver-stage schizonts and is the only drug that kills hypnozoites. The conjugate’s increased lipophilicity relative to that of its parent chemicals was predicted to ensure appropriate membrane permeability. Furthermore, the planned hybrid structure contained nucleophilic nitrogen, which was critical for protonation and accumulation of the molecule in digesting vacuoles. Furthermore, we expected structure 3 to be a non-substrate for the P. falciparum Chloroquine-Resistant Transporter (PfCRT), which is responsible for Plasmodium’s decreased sensitivity to chloroquinelike chemicals. These considerations backed up our theory that hybrid 3 could be a promising therapeutic candidate [9 , 10 ].. The freshly synthesised hybrid 3 was put to the test. In vitro assays and in vivo tests in rats were used to determine its activity against all stages of Plasmodium in the mammalian host. Both in vitro and in vivo, the chemical displayed considerable inhibitory effects against Plasmodium liver and blood-stage parasites (Figure 4)
Figure 4: Depiction of the Plasmodium life cycle in humans showing the skin, liver, and blood stages witht he corresponding existing (solid lines) and future (dashed lines) humanized mouse systems to model each oft he individual stages and eventually the full Plasmodium life cycle including pathology and transmission.
Infection is initiated when a female Anopheles mosquito injects saliva-containing sporozoites into the skin. Sporozoites traverse dermal cells and gain access to the blood. The highly motile sporozoites transit to the liver where each sporozoite infects a single hepatocyte. One to two weeks after hepatocyte invasion, merozoites exit the liver and begin a 48-h cycle of Red Blood Cell (RBC) invasion, replication, RBC rupture, and new merozoite release. During RBC infection, the parasite expresses variant surface antigens on the surface of the infected red blood cell, which interacts with Human Endothelial Receptors (hER), thus mediating the binding of infected RBCs to the microvascular endothelium of various organs. A small number of blood-stage parasites differentiate into sexual gametocytes, which are taken up by mosquitoes in blood meals to continue the transmission to new human hosts [11 , 12 ].
Assays for parasite inhibition in vitro
10,000 isolated salivary gland sporozoites were treated with the hybrid 3 for 15 minutes at 4 C before being transferred to albumincoated eight-well slides for the gliding-motility experiment. Sporozoites were allowed to glide for 15 minutes at 37°C before being fixed for 10 minutes with 4% paraformaldehyde (AppliChem). The slides were then cleaned in PBS/1 percent FCS before being blocked in PBS/10 percent FCS for 15 minutes at 37 degrees Celsius. Monoclonal anti P. berghei CSP antibody was used to visualise sporozoites. anti-mouse (Invitrogen). The wells were mounted in PBS with 10% glycerol and embedded in nail polish. Experiments were carried out in triplicate, with each well containing 100 sporozoites. The unpaired student’s t-test was used to determine statistical significance. Sporozoite invasion experiments were carried out using a modified approach previously reported. 30,000 sporozoites, in a nutshell were pre-incubated with the hybrid compound 3 for 15 minutes at 4 degrees Celsius before being transferred to confluent human hepatoma HuH7 cells for 90 minutes at 37 degrees Celsius in the presence of the compound [13 ].
Cells were washed, fixed, and sporozoites were stained with doublestaining to distinguish extracellular from intracellular sporozoites after incubation with sporozoites. Experiments were carried out in triplicate, with each well containing 100 sporozoites. An unpaired student’s t-test was used to determine statistical significance. As previously stated, exoerythrocytic stages were developed in a typical experimental method. 8-well chamber slides (Nunc) were plated with 3 104 HuH7 cells and grown to con-fluency at 37 C one day before sporozoite infection. Purified sporozoites suspended in complete medium were placed in the chambers and allowed to invade for a period of time. 90 minutes. The medium was replenished, and 1 M-10 nM of compound 3 was added. After that, medium was replenished on a daily basis [14]. Parasites were frozen, permeabilized, and stained by immune fluorescence antibody staining using hybridoma culture supernatant anti-HSP70 antibody after 24 or 48 hours of liver stage development, as described previously. For the strains K1 and K2, activity against P. falciparum blood stages was shown. The K1 strain of P. falciparum was used to test antiplasmodial activities (resistant to chloroquine and pyrimethamine).
The assay was modified from the [3 H]-hypoxanthine incorporation assay. Infected human red blood cells were subjected to serial drug dilutions in microtiter plates in RPMI 1640 media with 5% Albumax II [15 ]. After a 48-hour incubation period at 37°C in a low-oxygen environment, 0.5 Ci [3 H]- hypoxanthine was added to each sample. After another 24 hours of incubation, the cultures were harvested onto glass-fiber filters and rinsed with distilled water. A Beta plate TM liquid scintillation counter was used to count the radioactivity. The results were represented as a percentage of the untreated controls and were recorded as Counts Per Minute (CPM) per well at each medication concentration. The IC50 values were determined using the sigmoidal inhibition curves. The averages of four data from two independent experiments carried out in duplicate are used to calculate IC50 values. Malstat reported activity against blood stages for the strains 3D7 and Dd2. Assay The assay was used to determine the viability of the parasite. P. falciparum 3D7 or Dd2 synchronized ring stages were plated at 1% parasitemia and 5% parasitemia in RPMI 1640 medium with Albumax II. (5 g/L) on microtiter plates with 96 wells. The hybrid molecule was dissolved in a final concentration of 0.5 percent DMSO and added in serial dilutions (640 pM-50 M) [16]. The plate was incubated for 72 hours at 37 degrees Celsius in a humidified, airtight incubator with 5% CO2 and 5% O2 in N2. In a 96-well microtiter plate, parasites were cultured in vitro for 72 hours, resuspended, and aliquots of 20 L were taken and added to 100 L of Malstat reagent. A 20 L mixture of NBT (Nitro Blue Tetrazolium)/Diaphorase (1:1; 1 mg/mL stock each) was added to the Malstat reaction to determine PLDH activity. Optical densities were measured in an ELISA reader at 630 nm after the plates were agitated for 30 minutes at room temperature [17 ]. The tests were carried out in threes. A negative control of 0.5 percent aqueous DMSO was employed, as well as dilution series of chloroquine (2) and primaquine (1) as further controls. The IC50 values were derived from variable-slope sigmoidal dose-response curves using the Graph Pad Prism programme version 4 after each chemical was tested 2–3 times. For each chemical, the average IC50 value was computed (Table 1).
| Assay | % | Oocyst Number (Mean | % | Compounds (Dose) | Oocyst Number (Mean | % | % |
|---|---|---|---|---|---|---|---|
| Parasitemia (Gametocythemia) | ± SD) | Mosquitoes Infection | ± SD | Inhibition Mosquitoes Infection | Oocyst Reduction | ||
| 1 | 10.3 (42%) | 256±180 | 95 | 20(50mg/kg) 20(25mg/kg) PQ(15mg/kg) | 64 ± 64 | 5 | 81.3 |
| 7.3 (49%) | 137± 100 | 90 | 142±118 | 10 | 0 | ||
| 7.0% (45%) | 117 ± 72 | 90 | 0 ± 0 | 15 | 100 |
Table 1: Oocyst number of P. gallinaceum in Ae. fluviatilis. Mosquitoes were allowed to blood feed on chickens before and after treatment with compound 20 and PQ.
Microsomes: Determination of the hybrid’s metabolic stability in rat liver
The hybrid 3’s phase I metabolism was examined using cytochrome-P450 dependent monooxygenase. Microsomes were extracted from untreated female Sprague Dawley rats and male rats treated for three days with corn oil, beta-Naphthoflavone (bNF; 100 mol/kg/days), Phenobarbital (PB; 400 mol/kg/days), or both bNF + PB. The day after the last treatment, the animals were slaughtered and microsomes were prepared: the liver was homogenised in 0.25 M sucrose with 0.1 mM EDTA (pH 7.4) and centrifuged for 20 minutes at 10,000 g followed by 1 hour at 100,000 g. All of the steps were completed on ice. Microsomes were prepared and kept at 80 degrees Celsius until needed. Incubation methods for microsomal incubations in their entirety (final volume 1000 L) As a NADPH-generating system, the hybrid 3 (100 M), rat liver microsomal protein (1 mg/mL), 0.1 M phosphate buffer (pH7.4), and -nicotinamide adenine dinucleotide phosphate (NADPH,1 mM) were added. Isocitrate (10 mM), isocitrate dehydrogenase (0.05 U), MgCl2 (4 mM), and NADP (1 mM) were used to make the NADPH-generating system, which was pre-incubated for 5 minutes at 37 C before being added to the incubation system. For 15, 30, 60, and 90 minutes, the entire incubation system was incubated. After the incubation period, 8-hydroxyquinoline was added for quantification purposes, the reaction was stopped immediately, and 500 L ethyl acetate was extracted. The residues were diluted in 50 percent methanol/water (v/v) and submitted to ion pair HPLC with UV detection after the solvent had evaporated (255 nm). Incubations in the control group were carried out under the same conditions as the experimental group. Heat-deactivated microsomes were subjected to the same circumstances. A reversed phase column (Symmetry C18, 3.9 mm 150 mm, 5 m;Waters) was used for HPLC analysis. Mobile phase A: methanol/water (1:10, v/v) with added phosphoric acid (0.01 mM) and hexanesulfonate (5 mM); B: methanol; linear gradient: 100% A to 100% B in 30 minutes at 0.65 mL/min injection volume 10 L The metabolism of the hybrid 3 was quantitatively described as relative peak areas (peak area hybrid/peak area internal standard) [18, 19].
Antimalarial medication development status and new developments
Malaria remains a severe hazard in developing countries, with more than 1 million clinical episodes and 3000 deaths per day. Malaria killed between 150 and 300 million people in the last century, accounting for 2–5% of all deaths. Approximately 40% of the world’s population currently lives in malaria-infected areas. Young children and pregnant women get the most severe symptoms of the condition. Despite the fact that malaria is native to most tropical locations, Sub-Saharan Africa accounts for 90 percent of disease-related death. Antimalarial medications are the only therapy option because an approved vaccine for malaria has yet to be developed. Despite the fact that Chloroquine was the first antimalarial drug to be synthesized, for more than 30 years, Chloroquine has been a near-magical cure, but the advent and spread of Chloroquine resistant parasites has rendered it virtually worthless in most parts of the world [20]. Artemisinin, a plant derived antimalarial, is now the only medicine available that is effective against the parasite internationally. Despite the fact that various new medications have been launched in the last 30 years, widespread or isolated examples of resistance suggest that their efficacy will be limited. As a result, novel treatments and regimens for malaria control are urgently needed. This paper provides a review of current antimalarial treatment choices as well as current efforts to create new medications based on both recent technology developments and adjustments to existing treatments, as well as combination therapies. The majorities of antimalarial medications have been discovered and developed using traditional drug discovery techniques, while drug design based on pathogen and host genomic and proteomic data is still in its early stages. The parasite food vacuole, apicoplast, and mitochondrion have been identified as the key organelles for therapeutic targeting based on their significance in parasite development and survival [21, 22]. Several components of the metabolic process are also being studied as therapeutic targets. Some of the medications already in use or in research have clear mechanisms of action; however, the exact modes of action of many pharmaceuticals have yet to be determined. It will be feasible to build target specific medications with improved safety and efficacy using genome and proteome information. Chloroquine, a four-aminoquinoline, was first synthesised chemically in 1934 as a quinine alternative. Chloroquine is deposited specifically in the parasite’s feeding vacuole, where it works as an antimalarial by blocking the polymerization of the harmful haem. The parasite produces histidine-rich protein 2, which catalyses the conversion of haem into the non-toxic and insoluble haemozoin [7, 8]. Resistance to chloroquine in P. falciparum is linked to changes in a feeding vacuole transport protein rather than a shift in haem processing [9 ]. Chloroquine-resistant parasites emerged from four unique founder events that happened in various geographic areas, according to a genome-wide microsatellite analysis. Chloroquine resistance became widespread as a result of this spread [10]. Chloroquine resistance appears to be independent of changes in this locus in P. vivax [11]. When the newly formed World Health Organization (WHO) declared war on malaria and dedicated to its universal eradication in the early 1950s, Chloroquine rose to prominence.
Primaquine, an 8-aminoquinilone, is highly effective against hypnozoites, a dormant type of P. vivax liverstage parasites. Its one-of-a-kind characteristic makes it appropriate for treating P. vivax infections alone or in conjunction with other antimalarials.
Primaquine is effective against the parasite’s sexual stages and has been used successfully to eradicate malaria from the Vanuatu archipelago in the southwest Pacific [37]. In clinical trials in Indonesia, Colombia, and Papua New Guinea, primaquine was found to be exceedingly effective. Soldiers on jungle patrol in Colombia were given primaquine every day for 17 weeks in field studies. When compared to a placebo, daily dosage of primaquine was 94 percent effective [38 ]. It is 85% efficient against P. falciparum and 85% effective against P. vivax. Methaemoglobinemia and haemolysis in Glucose6-Phosphate Dehydrogenase (G6PD)- deficient people are two serious possible side effects of primaquine treatment. Minor gastrointestinal effects, such as stomach ache, are also linked to primaquine use, however these are normally minimised when the medicine is taken with food. In a recent field experiment, 2% of participants were unable to tolerate daily primaquine usage [39].
In malaria-endemic areas, multidrug-resistant parasites have become a serious treatment issue for healthcare providers. The development of drug resistance is the expected selective response of a microorganism to lifethreatening situations, in broad evolutionary terms. As a result, parasite resistance to all currently available antimalarial drugs is almost certain to emerge. in the near future In the field of antibacterial medications, cases of Staphylococcus resistant to vancomycin, the most powerful antibiotic, have begun to show up in emergency rooms across the United States. New medications will be needed to replace those that have lost their effectiveness as long as malaria remains a worldwide health problem [23, 24 ]. The bulk of currently available antimalarial medications have their origins in herbal remedies used by traditional healers. With the entire genomic sequence of the parasite, its host (human), and vector (Anopheles), new targets could be developed utilising rational drug design and other emerging technologies in the near future. Genome and proteome data, for example, have been crucial in the discovery of new diseases. Several parasite proteins are essential for the plastid to function properly. The identification of the type II fatty acid synthesis pathway in Plasmodium, as well as other plastid-related processes that differ significantly from their human counterparts, has opened up a new set of targets. The plastid’s prokaryotic origin will also serve as a predictor of which bacterial inhibitors might be effective antimalarial. The majority of the current targets were previously targeted for other human diseases. There is already a substantial body of scientific data and libraries of chemicals that can be used to combat these targets. A structural genomics project is presently ongoing with the goal of identifying the structure of prospective therapeutic targets in a large number of protozoan species. When these elements are joined, they form a synergy [25, 26]. Two lines of investigation will provide a strong impetus for the discovery of compounds with potent antimalarial activity. However, because similar targets are encoded in the human genome, developers of these compounds must ensure that the inhibitors have a high degree of selectivity towards the parasite enzyme. This is particularly important in the case of malaria, as more than 90% of malaria deaths occur in children under the age of five, an age group in which safety is vital. Malaria also affects some of the world’s poorest countries, where healthcare services similar to those seen in the Western world do not exist. Any antimalarial medicine developed in this situation would need to have a brief curative regimen, be effective with single-daily dose, and be cost-effective. affordably priced The majority of antimalarial drugs work by reducing or eliminating asexual erythrocytic-stage parasites in the infected host; however, none of these drugs are designed to treat the pathogenesis of severe malaria and cerebral malaria, which are responsible for the majority of malaria-related deaths in African children. An antimalarial medication that selectively targets malaria pathogenesis without requiring total parasite eradication could drastically reduce fatalities in young children while also addressing the problem of antimalarial treatments losing or losing efficacy [27 , 28]. In the absence of a viable malaria vaccine, new medications that are effective against all stages of malaria parasites, including gametocytes, will be required to eradicate the disease completely a case of malaria Through effective public–private collaborations, several for-profit and non-profit organizations are spearheading efforts to alleviate the burden of this devastating disease in endemic nations by discovering, producing, and providing novel inexpensive antimalarial medications. The MMV, a public and private collaboration that is now supporting research for the development of roughly two dozen novel chemicals for malaria therapy, is leading the charge in this area. These efforts are crucial in keeping the pipeline of antimalarial drugs alive. Resistance to PQ (primaquine) and CQ (chloroquine) in P. falciparum. The research looked into more than just PQ. However, there are various equivalents. 8-amino-2- methylquinolinecompound 1’a derivatives of 8-amino-2-methylquinoline comprising the amino-alkyl side a chain of PQ [compound-2’]and carboxy-primaquine [CPQ], which is a key metabolite of PQ PQ and compound 2 had weak effect against blood stages parasites, as expected, whereas analogues with no aminoalkyl side chain [compound 1 and CPQ] had no detectable activity at all. TQ also demonstrated only sporadic activity against parasites that live inside erythrocytes. Compound 2 lowered the IC-50 of CQ in the CQ-resistant K1 parasite strain from 390Nm to 40Nm at subinhibitory concentrations, almost identical to the CQ-sensitive D10 strain. [39Nm] PQ and TQ, compound 2, were studied in depth, and it was discovered that all three compounds had a substantial synergistic interaction with CQ in the resistant K1 strain, but have no influence on the IC-50 of the CQ-sensitive D10 strain [30].
The resistance reversing effect of PQ appears to be connected to its ability to induce CQ accumulation in parasites expressing a CQresistant of the pfcrt gene. Analogues missing the amino-alkyl side chain of PQ showed no resistance reversing activity. FV [FOOD VACCULE] membrane protein Plasmodium falciparum Chloroquine Resistances Transporter [PFCRT] is encoded by this gene. The effect of PQ and CQ accumulation in Q-resistant parasites is caused by changes in pfcrt, which was used to trans infect a CQ-sensitive parasite strain with a CQ-resistant pcfrt obtained from the Dd2 strain. The presence of the mutant PFCRT Protein is the only difference between the parasites and the sensitive strain. When compared to the identical parasite strain trans-infected with its own CQ-sensitive pfcrt, these parasites accumulated about a fourth of the CQ. In C3Dd12, PQ was found to entirely restore CQ accumulation in a dose-dependent manner, but CQ accumulation was unaffected in C2GC03. PQ was found to be even more effective than the well-known CQ-resistances reverse [verapamil] at recovering CQ accumulation in C3Dd2 [31, 32].
P. falciparum parasites, for example, appeared to be responsive to quinine in vitro sites of the ICEMRS will be used to track the emergence and spread of resistance. Vivax malaria is also endemic in several ICEMRS, and EX vivo drug tests for P. vivax are available are also being carried out, but the assays are hampered by the challenges of P. vivax culture and the recognition that certain drug assays [CHLOROQUINE] necessitate a high proportion of parasites in the ring stages and a high parasitemia.
Hope for new antimalarial medications stems from the discovery of novel antimalarial drug targets
Malaria is a severe global danger that claims the lives of over 2 million people every year. Due to the growth of drug-resistant parasites, the lack of a viable vaccine, and the expansion of insecticide resistant vectors, treating malaria is becoming increasingly challenging. As a result, new chemotherapeutic techniques are required for malaria treatment, necessitating the search for new drug targets. Different ways to identifying novel antimalarial drug targets are discussed here. In order to generate fresh, rationally designed lead compounds, we have also paid close attention to the existing proven targets. Some of the most significant parasite proteins have been proposed as targets; however, more in vitro or in vivo structure and function investigations of these proteins are required to confirm their suitability as targets [33]. The investigation of the interactome between the apicoplast, mitochondrion, and genomic DNA will be valuable in finding key pathways or proteins that regulate critical pathways for parasite growth and survival, and could be attractive targets. Molecules involved in parasite invasion of host erythrocytes, as well as infected erythrocyte ion channels, which are required for parasite intra-erythrocyte survival and stage progression, are becoming more appealing targets. This review will go through the present state of knowledge on prospective antimalarial drug targets that could be used to build new pathways or proteins influencing critical processes for parasite development and survival, apicoplast and mitochondrion analyses could be promising targets. Molecules involved in parasite invasion of host erythrocytes, as well as infected erythrocyte ion channels, which are required for parasite intra-erythrocyte survival and stage progression, are becoming more appealing targets. This review will go through the present state of knowledge on prospective antimalarial drug targets that could be used to build new antimalarial [34, 35].
Treatment with 8-aminoquinoline
Primaquine is the most widely used drug in this class for primary (causal) and terminal (post-exposure) malaria prophylaxis, radical cure of Plasmodium vivax and Plasmodium ovale (elimination of hypnozoites, the parasites’ dormant liver forms), and as a singledose gametocytocidal agent in Plasmodium falciparum infections [118] . Tafenoquine was discovered in 1978 [119], but it has taken a long time to reach the clinic, and it is currently in phase 3 clinical studies. Although its PK properties differ from those of Primaquine, if authorised, it is expected to have similar clinical indications. In its main role in terminal prophylaxis and radical treatment, Primaquine is usually given as a 14-day course. This regimen has a number of drawbacks, including hemolysis in individuals with Glucose- 6-Phosphate Dehydrogenase (G6PD) deficiency, dose-related gastrointestinal side effects, and so on. Methemoglobinemia is a risk, and because to its complexity, it has a low compliance rate [120]. Pretreatment screening for G6PD deficiency, drug administration with food, and monitoring for cyanosis and respiratory symptoms are all measures that can be used to reduce adverse effects, all of which are more likely if G6PD-normal patients are given abbreviated highdose regimens to improve compliance [121]. PK/PD investigations of different short-course regimens should be investigated, especially when models based on known single-dose PK data show that they should be safe, because toxicity may be depending on characteristics such as age and race/ethnicity [122]. Because intermediate and poor metabolizers have more relapses, the efficacy of Primaquine against liver forms of P. vivax may be connected to the activity of the CYP2D6 enzyme [123]. Models based on known single-dose PK data show that they should be safe, because toxicity may be depending on characteristics such as age and race/ethnicity. Furthermore, Lumefantrine is a recognised 2D6 inhibitor, coadministration of the ACT artemether lumefantrine and Primaquine may reduce the Primaquine component’s efficacy. PK/PD investigations are needed to investigate these interactions in greater depth, especially since the formation of temporary active phenolic metabolites may kill hypnozoites while potentially promoting toxicity [124]. Primaquine might thus be a pro-drug that needs to be broken down in the body before it can be used. The inclusion of a 5-(3-trifluoromethyl)-phenoxy group in tafenoquine, but not Primaquine, is thought to be the explanation for Tafenoquine’s longer elimination t12 (14 days vs. 4–6 h) and reduced proclivity for methemoglobinemia [119]. A single 300 mg dose regimen, based on PK/PD and efficacy data from studies of a variety of dose regimens given in combination with CQ, appears to be the most effective. A standard 14 days course of Primaquine 15 mg/day appears to be at least as effective in avoiding P. vivax relapses as a mg Tafenoquine dosage, with a similar frequency of side effects [125,126]. There is growing evidence that, like primaquine, CYP2D enzyme system function is required for antimalarial action [127]. Concerns about Tafenoquine’s renal and ocular damage appear to be unfounded [128]. Although data from ongoing phase 3 trials could provide further information. In conclusion, 8-aminoquinoline medicines play an important role in the treatment and control of malaria. The use of PK/PD has helped with Tafenoquine dose optimization, but further research is needed to investigate the interactions between the two medicines in this class’s metabolism, efficacy, and toxicity. The protracted process of elimination because prolonged and severe hemolysis can occur in G6PD-deficient people who are accidentally treated with this medicine, t12 of Tafenoquine has implications for the necessity of effective G6PD screening. The feasibility and cost-effectiveness of using CYP2D6 metabolizer status as a predictor of parasitological response and adverse effects is unknown at this time, but it could be the topic of future research.
Novel antimalarial medications
The threat of Artemisinin resistance has heightened the urgency to discover novel antimalarial treatments that are both efficacious and well tolerated [129]. The spiroindolone class is arguably the most clinically relevant. These medications stop parasites from making proteins [130]. A potential drug resistance mutation has also been postulated as a specific molecular target for the spiroindolones in the gene encoding the P-type Cationtransporter ATPase4 (PfATP4). The medications may disrupt wild-type PfATP4, causing major rheological changes in parasitized erythrocytes, which are subsequently quickly removed by the reticulo-endothelial system [131]. The spiroindolone cipargamin has advanced from dose-finding and safety research to human malaria testing. A 3-day regimen of 30 minutes each day was developed based on volunteer data [132] and allometric scaling from animal research. A PK and early effectiveness investigation of initial parasite clearance in small groups of individuals with falciparum or vivax malaria was conducted at a dose of mg/day [133]. The parasite clearance was rapid, with a t12 of 21 hours, justifying daily dosage. Hepatic dysfunction, which occurred in 14 percent of malaria patients in the two human investigations [133], was a possible safety signal that needs to be investigated in larger-scale comparative trials. The history of antimalarial treatment over the last 60 years or so, during which the therapeutic armamentarium has been gradually depleted due to parasite drug resistance, provides compelling evidence for using quantitative pharmacology tools in the development or validation of dose regimens. Recent advancements in sample schedules, assay technology, and PK/PD modeling have resulted in more evidencebased treatments, particularly for higher risk groups including children and pregnant women. PK/PD investigations may become part of routine monitoring of efficacy in phase 4 rather than merely at earlier stages of drug development as technology becomes more cost effective. This could make early detection of treatment failure easier, limiting the potential for significant human and social harm. Malariarelated morbidity and mortality have an impact. Antimalarial therapy advancements should not, however, be used to replace other parts of malaria control, such as the use of insecticide-impregnated bed nets and vector control methods.
Expert opinions
The growing use of highly sensitive LC-MS/MS assays and more convenient sample regimens (low blood volume and sparse time points post-dose), in combination with robust population PK/PD analyses that include Using existing data, researchers have identified patient categories that may be underdosed. Young children given IV Artesunate for severe disease and oral artemether lumefantrine for uncomplicated malaria, as well as pregnant women given CQ, SP, Lumefantrine, and Piperaquine as part of ACT, are good examples. In these instances, newly recommended dosage mg/kg regimens (which can be based on simulations from PK/PD models) should ideally be evaluated further to confirm enhanced efficacy without an increase in undesirable effects [40]. Because there are signs that Artemisinin derivative doses may reach a toxicity-related ceiling without reversing the recently observed Artemisinin resistance or tolerance (delayed initial parasite clearance rather than increased late recrudescence), modelling suggests that the role of the longer-acting partner drug is critical in preventing higher-grade infections. A failure of treatment However, with the loss of the ACT components’ mutual protection, there is a frightening prospect of widespread clinically significant ACT failure in the nottoo distant future [41]. As a result, new schizonticidal medicines with a fast onset of action are required eliminate parasites quickly and could thus become a viable alternative to Artemisinin medicines when used in conjunction with a longer-acting partner treatment. More research is needed to assess their efficacy, acceptability, and safety, as well as any potential PK/PD interactions with potential partners such as Lumefantrine, Piperaquine, or Naphthoquine. In the context of HIV treatment, potential medication interactions with ACT components have been discovered, as well as with pharmaceuticals that are known to alter ventricular repolarization. These could be helpful in the event of HIV to reduce the incidence of recurrent malaria, but there’s also a chance that ART interactions will reduce ACT’s efficacy by reducing drug exposure. PK/PD studies are critical for determining the right dose while maximising the potential for benefit. Because electrocardiographic monitoring may not be possible where health care facilities are limited, it is critical to reduce the risk of adverse cardiovascular outcomes when antimalarial drugs that prolong the QTc are used, by adhering to recommended dose regimens and avoiding additional pharmacotherapy with agents that have the same effect (such as macrolide antibiotics). In this context, detailed in vitro and in vivo assessment of the potential for 4- Aminoquinolines and similar medicines to produce malignant dysrhythmias is also necessary so that relative risks may be able to be measured. Halofantrine and Lumefantrine, for example, are chemically similar but have different cardiotoxicity profiles. Primaquine is still the sole treatment for P. vivax infections that is both effective and safe. gametocytocidal agent with the highest efficacy. Tafenoquine, a chemically similar 8-amminoquinoline molecule, has taken a long time to create. Because Tafenoquine has a substantially longer (14-day) elimination t12 than Primaquine, persistent hemolysis in G6PD-deficient patients is a major problem. The new development of point of care testing for G6PD status may aid in the practical application of Tafenoquine, which may have a larger potential than Primaquine for reducing the consequences of repeated vivax relapses on the risk of anaemia and local malaria transmission. It is important to remember that improvements in antimalarial therapy are greatest when other components of control are addressed, such as the use of insecticide-impregnated bed nets and vector-reduction strategies. Because of this, the WHO’s goal of eradication has been reintroduced such a well-thought-out strategy [42, 43].
Novel antimalarial medications
The threat of Artemisinin resistance has heightened the urgency to discover novel antimalarial treatments that are both efficacious and well tolerated. The spiroindolone class is arguably the most clinically relevant. These medications stop parasites from making proteins. A potential drug resistance mutation has also been postulated as a specific molecular target for the spiroindolones in the gene encoding the P-type Cation Transporter ATPase4 (PfATP4). The medications may disrupt wild-type PfATP4, causing major rheological changes in parasitized erythrocytes, which are subsequently quickly removed by the reticuloendothelial system. The spiroindolone cipargamin has advanced from dose finding and safety research to human malaria testing. A 3-day regimen of 30 minutes each day was developed based on volunteer data. Allometric scaling from animal research. A PK and early effectiveness investigation of initial parasite clearance in small groups of individuals with falciparum or vivax malaria was conducted at a dose of mg/day. The parasite clearance was rapid, with a t12 of 21 hours, justifying daily dosage. Hepatic dysfunction, which occurred in 14 percent of malaria patients in the two human investigations , was a possible safety signal that needs to be investigated in larger-scale comparative trials.
Outcome
The history of antimalarial treatment over the last 60 years or so, during which the therapeutic armamentarium has been gradually depleted due to parasite drug resistance, provides compelling evidence for using quantitative pharmacology tools in the development or validation of dose regimens [45, 46]. Recent advancements in sample schedules, assay technology, and PK/PD modeling have resulted in more evidence based treatments, particularly for high risk groups including children and pregnant women. PK/PD investigations may become part of routine monitoring of efficacy in phase 4 rather than merely at earlier stages of drug development as technology becomes more cost-effective. This could make early detection of treatment failure easier, limiting the potential for significant human and social harm. Malaria related morbidity and mortality have an impact. Antimalarial therapy advancements should not, however, be used to replace other parts of malaria control, such as the use of insecticide-impregnated bed nets and vector control methods [47].
Expert opinions
The growing use of highly sensitive LC-MS/MS assays and more convenient sample regimens (low blood volume and sparse time points post-dose), in combination with robust population PK/PD analyses that include Using existing data, researchers have identified patient categories that may be under dosed. Young children given IV Artesunate for severe disease and oral artemether Lumefantrine for uncomplicated malaria, as well as pregnant women given CQ, SP, Lumefantrine, and Piperaquine as part of ACT, are good examples. In these instances, newly recommended dosage mg/kg regimens (which can be based on simulations from PK/PD models) should ideally be evaluated further to confirm enhanced efficacy without an increase in undesirable effects [48].
Because there are signs that Artemisinin derivative doses may reach a toxicity-related ceiling without reversing the recently observed Artemisinin resistance or tolerance (delayed initial parasite clearance rather than increased late recrudescence), modelling suggests that the role of the longer-acting partner drug is critical in preventing highergrade infections. A failure of treatment However, with the loss of the ACT components’ mutual protection, there is a frightening prospect of widespread clinically significant ACT failure in the nottoo distant future [49].
As a result, new schizonticidal medicines with a fast onset of action are required spiroindolones eliminate parasites quickly and could thus become a viable alternative to Artemisinin medicines when used in conjunction with a longer-acting partner treatment. More research is needed to assess their efficacy, acceptability, and safety, as well as any potential PK/PD interactions with potential partners such as Lumefantrine, Piperaquine, or Naphthoquine [50, 51].
In the context of HIV treatment, potential medication interactions with ACT components have been discovered, as well as with pharmaceuticals that are known to alter ventricular repolarization. These could be helpful in the event of HIV. Reducing the incidence of recurrent malaria, but there’s also a chance that ART interactions will reduce ACT’s efficacy by reducing drug exposure. PK/PD studies are critical for determining the right dose while maximising the potential for benefit [51, 52 ]. Because electrocardiographic monitoring may not be possible where health-care facilities are limited, it is critical to reduce the risk of adverse cardiovascular outcomes when antimalarial drugs that prolong the QTc are used, by adhering to recommended dose regimens and avoiding additional pharmacotherapy with agents that have the same effect (such as macrolide antibiotics). In this context, detailed in vitro and in vivo assessment of the potential for 4-aminoquinolines and similar medicines to produce malignant dysrhythmias is also necessary so that relative risks may be calculated. This can be measured. Halofantrine and lumefantrine, for example, are chemically similar but have different cardio toxicity profiles [53V].
Primaquine is still the sole treatment for P. vivax infections that is both effective and safe. Gametocytocidal agent with the highest efficacy. Tafenoquine, a chemically similar 8-amminoquinoline molecule, has taken a long time to create. Because Tafenoquine has a substantially longer (14-day) elimination t12 than Primaquine, persistent hemolysis in G6PD-deficient patients is a major problem. The new development of point-of-care testing for G6PD status may aid in the practical application of Tafenoquine, which may have a larger potential than Primaquine for reducing the consequences of repeated vivax relapses on the risk of anaemia and local malaria transmission [54].
It is important to remember that improvements in antimalarial therapy are greatest when other components of control are addressed, such as the use of insecticide-impregnated bed nets and vectorreduction strategies. Because of this, the WHO’s goal of eradication has been reintroduced such a well-thought-out strategy.
A five-year perspective
Given recent advancements in sample, assay, and population modelling technology, the possibility of more convenient, less expensive, and collaborative PK/PD investigations is real. This should lead to the creation of more sensible antimalarial treatment regimens adapted to the clinical setting, such as for the very young, pregnant women, and those with coexisting diseases like HIV [55, 56]. Although conventional Therapeutic Drug Monitoring (TDM) with immediate clinical application is problematic in resource-constrained environments, DBS sampling and a rapid turnover LC-MS/MS assay in a central facility, along with current information technology, can help. Technology has the potential to improve the everyday management of individual patients in remote locations while also providing a rich source of pharmacoepidemiological data. When frequent TDM is not practicable due to cost or logistical constraints, this technique could be utilised to see if sub therapeutic drug concentrations are to blame for clinical treatment failures that occur from time to time or when drug quality is in question. In order to maximize mutual protection against parasite resistance, researchers should evaluate the tolerance, efficacy, and toxicity of new combinations of existing medications, such as employing more than two drugs together or more frequent dosage throughout the same treatment period [57, 58]. This could apply to antimalarial medications that have been on the shelf for a while due to prior resistance but are now being used again. Parasite sensitivity has reappeared, according to in vitro and other evidence (Table 2).
| Assay | Compound | % Reduction (Mean Parasitemia ± SD)* | Survival (Mean ± SD) |
|---|---|---|---|
| 5th 7th | |||
| 4.6 ± 2 31 ± 6.4 | 13 ± 3 | ||
| Non treated CQ** | 99% (0.1 99% | ||
| 6 | ± 0) (0.4 ± | 22 ± 6 | |
| 0.4) | |||
| 1 | 0% (4.9 ± | ||
| 1.7) 11% | 16 ± 3 | ||
| (27.2 ± | |||
| 0% (5 ± 6.8 | |||
| 1.7) 2% (30 | 20 ± 7 | ||
| 8 | ± 16.2) |
Table 2: Antimalarial activity of synthetic compounds in mice infected with P. berghei treated with daily doses of 25 mg/kg body weight for three consecutive days.
Plan of Work
Antimalaria medications are used to treat and prevent malaria infection. The majority of antimalaria treatments target the erythrocytic phases of malaria infection, which is the stage of infection that causes symptoms. The fundamental goal of treatment is to remove the diseasecausing parasites from a patient’s bloodstream as quickly as possible, in order to prevent an uncomplicated case of malaria from progressing to severe disease or death. Antimalaria drugs function by destroying malaria parasites in their early stages of development in the liver and red blood cells. The life cycle of malaria parasites is the goal of this project.
• Antimalaria medications now in use
• Chloroquine-resistant and multidrug-resistant malaria
• Recent breakthroughs in antimalaria drug therapy – Analogs of existing agents, Natural products, Compounds Used in combination therapies involved in the fight against different diseases , Active compounds against newer targets (Table 3, 4, 5).
| Compound | IC50 (M) | ||
|---|---|---|---|
| 1 | |||
| 2 | |||
| Hybrid 3 | |||
| 1 and 2 | 3D7 | Dd2 | K1 |
| 3.11 ± 1.536 | 1.12 ± 0.351 | 46 ± 0.08 | |
| 0.03 ± 0.002 | 0.26 ± 0.126 | 146 ± 0.02 | |
| 0.64 ± 0.046 | 58 ± 0.185 | 0.08 ± 0.0048 | |
| 0.03 ± 0.012 | 0.19 ± 0.035 | 0.169 ± 0.055 | |
Table 3: Antiplasmodial activity of the hybrid compound 3 on the asexual blood stages of three P. falciparum strains. Infected human red blood cells were incubated with serial compound dilutions for a total exposure time of 72 h. Endpoint reading was done by Malstat (3D7 and Dd2) or by incorporation od titrated hypoxanthine (K1).
| Compound | Relative gametocytemia (%) |
|---|---|
| 1 | 0.2* ± 0.05 |
| 2 | 0.9 ± 0.07 |
| Hybrid DMSO control | 3 0.7* ± 0.04 |
| 1.0 ± 0.19 |
Table 4: Gametocytogenesis inhibition assay in P. falciparum. P. falciparum NF54 gametocytes were incubated with hybrid 3 for 48 h. After 7 days of compound-free cultivation gametocytemia (gametocytes stages IV and V) was determined on Giemsa-stained blood films. 0.5% aqueous DMSO served as negative control and a dilution series (640 pM–50 M) of chloroquine (2) and primaquine (1) as additional controls were used. The hybrid compound 3 was added in a serial dilution of 640 pM–50 M dissolved in 0.5% aqueous DMSO.
| Analyte | Experimental | Results | Application |
|---|---|---|---|
| conditions | |||
| CQ | Method A: direct spectrofluorimetric in tablets | Linearity: 1–10 lg/mL in 0.05 | Tablets |
| in 0.05 M H2SO4 and method B involves prior extraction of CQ base in chloroform | M H2SO4 with a LOD: | ||
| 0.77 lg/mL | |||
| CQ and | Ion-pair formation with | Linearity for CQ and pyrimethamine: 2.0– | Drug |
| pyrimethamine | molybdenum and thiocyanate followed by its | 42 | |
| extraction with methylene chloride | and 2.0–43.0 lg/mL, respectively. The Sandell | ||
| sensitivity for CQ and | |||
| pyrimethamine: | |||
| 0.027 and | |||
| 0.042 lg/cm | |||
| Amodiaquine (AQ) and CQ (CQ) | Spectrophotometric methods | Beer’s law: 0.2–4.0 and | Pure and dosage forms. |
| based on their oxidation | 0.5–5.0 lg cm3 | ||
| with potassium iodate and | , LOD: 0.04 | ||
| potassium bromate, respectively. The initial rates | and 0.06 lg cm3 for AQ | ||
| of oxidation of AQ and CQ | and CQ. | ||
| were monitored at 342 and | |||
| 343 nm, the wavelengths of maximum absorptions of | |||
| the two drugs.. | |||
| Primaquine and CQ | spectrophotometry | Linearity: 2–10 | Liposome dosage |
Table 5A: Conditions of spectrophotometric methods used for the determination of CQ inp harmaceutical formulations and biological fluids.
Targets |
Actions | Organism |
|---|---|---|
| AFe(II)-protoporphyrin IX | Antagonist other/unknown Inhibitor | Plasmodium falciparum Humans |
| Humans | ||
| UKeratin, type II cytoskeletal 7 | ||
| URibosyldihydronicotinamide dehydrogenase [quinone] | ||
Table 5B: Mechanism of action.
Drug Profile
1. Synonyms: Chloraquine, Chlorochin, Chloroquina, Chloroquine, Chloroquinium Chloroquinum, Cloroquina
2. Summary: Chloroquine is an antimalarial drug used to treat susceptible infections with P. vivax, P. malariae, P. ovale, and P. falciparum. It is also used for second line treatment for rheumatoid arthritis.
3. Generic Name- Chloroquine
4. Drug Bank Accession Number-DB00608
5. Background: Chloroquine is an aminoquinoline derivative first developed in the 1940s for the treatment of malaria.
The drug of choice to treat malaria until the development of newer antimalarials such as Pyrimethamine, Artemisinin, and Mefloquine. Chloroquine and its derivative hydroxychloroquine have since been repurposed for the treatment of a number of other conditions including HIV, systemic lupus erythematosus, and rheumatoid arthritis. The FDA emergency use authorization for hydroxychloroquine and chloroquine in the treatment of COVID-19 was revoked on 15 June 2020.21 Chloroquine was granted FDA Approval on 31 October 1949.20
6. Type-Small Molecule
7. Groups-Approved, Investigational, Vet approved 8. Weight Average: 319.872 8. Monoisotopic: 319.181525554 9. Chemical Formula:C18H26ClN3 [59, 60].
Pharmacology
Indication:
Chloroquine is indicated to treat infections of P. vivax, P. malariae, P. ovale, and susceptible strains of P. falciparum.19 It is also used to treat extraintestinal amebiasis.19 Chloroquine is also used off label for the treatment of rheumatic diseases,4 as well as treatment and prophylaxis of Zika virus.1,2 Chloroquine is currently undergoing clinical trials for the treatment of COVID-19.3
Associated Conditions:
Discoid Lupus Erythematosus (DLE)
Extraintestinal Amebiasis
Plasmodium Infections
Polymorphic Light Eruption (PLE)
Porphyria Cutanea Tarda
Rheumatoid Arthritis
Sarcoidosis
Acute, uncomplicated Malaria
Contraindications & Blackbox Warnings:
Avoid life-threatening adverse drug events Improve clinical decision support with information on contraindications & black box warnings, population restrictions, harmful risks, & more.
Pharmacodynamics:
Chloroquine inhibits the action of heme polymerase, which causes the buildup of toxic heme in Plasmodium species [11 ]. It has a long duration of action as the half life is 20-60 days.10 Patients should be counselled regarding the risk of retinopathy with long term usage or high dosage, muscle weakness, and toxicity in children [19].
Mechanism of action:
Chloroquine inhibits the action of heme polymerase in malarial trophozoites, preventing the conversion of heme to hemazoin [11, 15 , 16]. Plasmodium species continue to accumulate toxic heme, killing the parasite [11]. Chloroquine passively diffuses through cell membranes and into endosomes, lysosomes, and Golgi vesicles; where it becomes protonated, trapping the Chloroquine in the organelle and raising the surrounding pH [10, 13]. The raised pH in endosomes, prevent virus particles from utilizing their activity for fusion and entry into the cell [14]. Chloroquine does not affect the level of ACE2 expression on cell surfaces, but inhibits terminal glycosylation of ACE2, the receptor that SARS-CoV and SARS-CoV-2 target for cell entry [13, 14] . ACE2 that is not in the glycosylated state may less efficiently interact with the SARSCoV- 2 spike protein, further inhibiting viral entry [14].
Absorption:
Chloroquine oral solution has a bioavailability of 52-102% and oral tablets have a bioavailability of 67-114%.10 Intravenous chloroquine reaches a Cmax of 650-1300μg/L and oral Chloroquine reaches a Cmax of 65-128μg/L with a Tmax of 0.5h.10
Volume of distribution:
The volume of distribution of Chloroquine is 200-800L/kg.10
Protein binding:
Chloroquine is 46-74% bound to plasma proteins.9 (-)-chloroquine binds more strongly to alpha-1-acid glycoprotein and (+)-chloroquine binds more strongly to serum albumin.8
Metabolism:
Chloroquine is N-dealkylated primarily by CYP2C8 and CYP3A4 to Ndesethylchloroquine.5,6,7,10 It is N-dealkylated to a lesser extent by CYP3A5, CYP2D6, and to an ever lesser extent by CYP1A1.5,6,7,10 N-desethylchloroquine can be further N-dealkylated to Nbidesethylchloroquine, which is further N-dealkylated to 7-chloro- 4-aminoquinoline.10
How over products below to view reaction partners
1. Chloroquine:
(R)-chloroquine, N-desethyl
N-bidesethylchloroquine
7-chloro-4-aminoquinoline
Route of elimination:
Chloroquine is predominantly eliminated in the urine [10V] 50% of a dose is recovered in the urine as unchanged Chloroquine, with 10% of the dose recovered in the urine as desethylchloroquine [10].
Half-life: The half life of chloroquine is 20-60 days [10]
Clearance:
Chloroquine has a total plasma clearance of 0.35-1L/h/kg [10]
Adverse Effects:
Improve decision support & research outcomes with structured adverse effects data, including: black box warnings, adverse reactions, warning & precautions, & incidence rates.
Toxicity:
Patients experiencing an overdose may present with headache, drowsiness, visual disturbances, nausea, vomiting, cardiovascular collapse, shock, convulsions, respiratory arrest, cardiac arrest, and hypokalemia.19 Overdose should be managed with symptomatic and supportive treatment which may include prompt emesis, gastric lavage, and activated charcoal [19]
Drug Interactions:
This information should not be interpreted without the help of a healthcare provider. If you believe you are experiencing an interaction, contact a healthcare provider immediately. The absence of an interaction does not necessarily mean no interactions exist.
Food Interactions:
Take with food. Food reduces irritation and increases bioavailability.
Products:
Drug product information from 10+ global regions our datasets provide approved product information including: dosage, form, labeller, route of administration, and marketing period.
2. Primaquine
Synonyms: Primachin, Primachina, Primachinum, Primaquin, Primaquina, Primaquine, Primaquinum
Summary: Primaquine is an antimalarial indicated to prevent relapse of vivax malaria.
Generic Name: Primaquine
DrugBank Accession Number: DB01087
Background: An aminoquinoline that is given by mouth to produce a radical cure and prevent relapse of vivax and ovale malarias following treatment with a blood schizontocide. It has also been used to prevent transmission of falciparum malaria by those returning to areas where there is a potential for re-introduction of malaria. Adverse effects include anemias and GI disturbances. (From Martindale, The Extra Pharmacopeia, 30th ed, p404 [61]
Type: Small Molecule
Groups: Approved
Weight Average: 259.3467
Monoisotopic: 259.168462309
Chemical Formula: C15H21N3O
Pharmacology:
Indication: For the treatment of malaria. Reduce drug development failure rates Build, train, & validate machine-learning models with evidence-based and structured datasets [62].
Associated Conditions:
Malaria caused by Plasmodium ovale
Malaria caused by Plasmodium vivax
Plasmodium Infections
Contraindications & Blackbox Warnings:
Avoid life-threatening adverse drug events Improve clinical decision support with information on contraindications & black box warnings, population restrictions, harmful risks, & more.
Pharmacodynamics:
Primaquine is an antimalarial agent and is the essential codrug with chloroquine in treating all cases of malaria. In the blood, malaria parasites break down a part of the red blood cells known as haemoglobin. When this happens haemoglobin is divided into two parts; haem and globin. Haem is toxic to the malaria parasite. To prevent it from being damaged, the malaria parasite produces an chemical which converts the toxic haem into a non-toxic product. Primaquine acts by interfering with a part of the parasite (mitochondria) that is responsible for supplying it with energy. Without energy the parasite dies. This stops the infection from continuing and allows the person to recover. Primaquine kills the intrahepatic form of Plasmodium vivax and Plasmodium ovale, and thereby prevents the development of the erythrocytic forms that are responsible for relapses (it also kills gametocytes). Primaquine is not used in the prevention of malaria, only in the treatment. It has insignificant activity against the asexual blood forms of the parasite and therefore it is always used in conjunction with a blood schizonticide and never as a single agent. Primaquine has gametocytocidal activity against all plasmodia, including P. falciparum [63, 64].
Mechanism of action
Primaquine’s mechanism of action is not well understood. It may be acting by generating reactive oxygen species or by interfering with the electron transport in the parasite. Also, although its mechanism of action is unclear, primaquine may bind to and alter the properties of protozoal DNA (Table 6).
| mm) | with 0.005 M | ||||||
| reversed-phase column | sodium | ||||||
| heptanesul fonate. | |||||||
| CQ | Plasma and urine | Diethyl ether, LLE | Waters silica- based | 0.2 M sodium dihydroge n phosphate, MeOH, and | HPLC- UV (254 | LODs: | 1 |
| and DCQ | reversed-phase column (Bondapak; | ACN at a ratio of 65:30:5, | nm) | 1 and | |||
| 10 lm, 3.9 300 | with 1 mL of perchloric acid/100 mL of solution | 0.5 | |||||
| mm). | ng/mL for CQ and DCQ. LOQs. 3 | ||||||
| ng/mL for CQ | |||||||
| Quinin e, HCQ, CQ, | Serum, Whole Blood, and Filter PaperAd sorbed Dry Blood | LLE | A stainless steel tube | 705 g | HPLC- UV (215 | LOQ: 0.005– | 1.5 |
| and DCQ | (150 mm 5 mm i.d.) | Ammoniu m perchlorat e to 500 mL of MeOH- | nm) | 0.01 | |||
| packed with Spherisorb S5SCX | water (98.5:1.5). | mg/L for CQ and hydrox yCQ and 0.05 | |||||
| sulfophenylprop ylmodified silica (average particle size, 5 mm; | The pH was adjusted to | mg/L for quinin e. | |||||
| Hichrom, Woodley, U.K.) | pH 8.0 by adding 110 mL MeOH NaOH (50 | ||||||
| mM) | |||||||
| CQ | Human | Protein | 5 mm | MeOH | HPLC- | LOQ: | 1 |
Table 6: Conditions of HPLC-UV, HPLC-DAD, HPLC-FLD, and HPLC-MS methods used for the determination of CQ in pharmaceutical formulations and biological fluids.
Half-life:
3.7-7.4 hours
Adverse Effects:
Improve decision support & research outcomes with structured adverse effects data, including: black box warnings, adverse reactions, warning & precautions, & incidence rates. Drug Interactions: This information should not be interpreted without the help of a healthcare provider. If you believe you are experiencing an interaction, contact a healthcare provider immediately. The absence of an interaction does not necessarily mean no interactions exist [65].
Food Interactions:
Take with food. Food decreases irritation. PRODUCTS:
rug product information from 10+ global regions our datasets provide approved product information including: dosage, form, labeller, route of administration, and marketing period (Table 6).
Material & Method
Malaria parasites in rodents in the laboratory:
In this paper, we present a set of techniques for the cyclic transmission of rodent malaria parasites in the laboratory. Both in vivo and in vitro, this is now doable. We concentrate on the approaches that are the least “resource expensive” and generic, and that we have shown to be applicable to any parasite–host combination. Nonetheless, we understand that the ability to create transgenic “reporter” parasites/ hosts now allows for the employment of sophisticated analytical and imaging techniques in vitro, ex vivo, and in vivo in specific situations. The methods described here are those that are commonly employed to keep P. berghei alive; where applicable, we mention significant differences when transmitting other parasite species Plasmodium berghei, P. yoelii, and P. chabaudi, among other rodent malaria parasites, have proved extremely valuable in the development of our understanding of the core molecular and cellular biology of malaria. this parasitic genus Whereas one might expect the utility to be high, it isn’t. Nothing caused the prevalence of these parasites to decline as knowledge grew [66, 67 ].
Could not be further from the truth; today, more than ever before, improvements in parasite-specific genetic technologies, and parasitespecific genetic technologies Mice as laboratory hosts and vectors (e.g., Anopheles stephensi) These species, and possibly P. berghei in particular, have the potential to be extremely powerful. systems for making in-depth investigations of the molecular foundation of disease the parasite–vector and host–parasite connections While we have discovered that passing P. berghei in a sequential manner is conceivable, throughout its entire life cycle using techniques in culture [68].
Anesthetic:
Combine 1 volume Rompun (2-(2,6-xylidino)-5,6-dihydro-4 H-1,3-thiazine hydrochloride, Bayer) with 2 volumes Ketaset/Vetalar (100 mg/ml ketamine, Fort Dodge) and 3 volumes sterile phosphate buffered saline (PBS). Working stock can be held at room temperature for up to 2 weeks if stored at 4°C (RT). To perform cardiac puncture, dilute the mixture to 2–5 l/g body weight for limited anaesthesia and 15 l/g body weight for deep/terminal anaesthesia.
Phenylhydrazine stock:
PBS solution containing 6 mg/ml phenylhydrazinium chloride Filter-sterilize, aliquot, and store for no more than 2 months at 20°C. Due to the quick oxidation of phenylhydrazine, the solution should not be reused once defrosted. Inoculate mice intraperitoneally (i.p.) at a rate of 10 l/g body weight to produce reticulocytosis. Three doses of inoculation are recommended. days before the host is infected through the transmission of contaminated blood Prepare the cryopreservation medium by combining 9 volumes of Alsever’s solution with 1 volume glycerol. Sterilize by filtering, then aliquot and store at 20°C or room temperature [69 ].
Heparin stock:
Dissolve 300 units/ml preservative-free heparin in PBS, filtersterilize, aliquot, and store at 20°C. Use in such a way that the final blood concentration is 30 units/ml. Fructose/PABA mosquito feed: 8 percent fructose in demineralized water, 0.05 percent P-Aminobenzoic Acid (PABA). Place in an autoclave and keep at 4°C. The distributed feed can be supplemented with a vitamin A, D, and iron cocktail. Plasmodipur filters or CF11 cellulose powder (Whatman) for leucocyte elimination. Erythrocyte lysis. RBC lysis buffer A. 10 stock solution: 1.5 M NH 4 Cl, 100 mM KHCO 3, 10 mM EDTAH 2 O, pH 7.4 Keep the stock solution at room temperature. The lysis buffer should be maintained in the refrigerator at working strength. Gey’s solutions (b). 1,000 mL (NH 4 Cl 35.0 g, KCl 1.85 g, Na 2 HPO 4 12H2O 1.5 g, KH 2 PO 4 0.12 g, glucose 5.0 g, phenol red 50.0 mg) Gey’s stock solution A 100 mL (MgCl2 6H2O 0.42 g, MgSO4 7H2O 0.14 g, CaCl2 0.34 g) Gey’s stock solution B 100 mL (NaHCO 3 2.25 g) Gey’s stock solution C Gey’s working solution is as follows: Stock A has 20 pieces; Stock B has 20 parts. Distilled H2O, 70 parts; Stock C, 5 parts; ycodenz stock solution (definited as 100%): In 200 ml Nycodenz buffer (0.03 percent w/v Tris– HCl, 0.0061 percent w/v CaNa 2 EDTAH 2 O, 0.011 percent w/v KCl, pH 7.5), dissolve 55.2 g Nycodenz (Axis-Shield, 1002424). Autoclave and keep at room temperature. In density gradient centrifugation, Nycodenz significantly improves parasite survival when compared to Percoll [70].
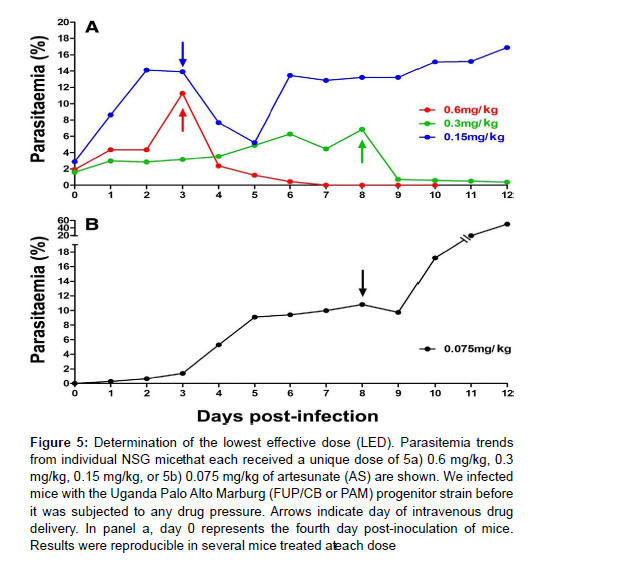
Coelenterazine Loading Buffer (CLB): pH 7.24–7.31, 20 mM HEPES, 20 mM glucose, 4 mM sodium bicarbonate, 1 mM EDTA, and 0.1 percent BSA in PBS Membrane feeders are number ten. Discovery Workshops, 516A Burnley Road, Accrington, Lancashire, BB5 6JZ, UK, sells Hemotek membrane feeders with integrated electrical warmers and reservoirs of 1 ml or 3 ml. Feeders made entirely of glass (requires rotating water bath) in a variety of sizes based on Wade’s design are available from a variety of suppliers. We frequently utilise Wade-style Perspex feeders (100, 250, 500, or 1,000 l) that we produce in-house. Membranes. Two-way stretch para film) is enough in the vast majority of cases. We employed Baudruche membrane, which was previously available from, for the fastidious mosquito (Figure 5).
Figure 5: Determination of the lowest effective dose (LED). Parasitemia trends from individual NSG mice that each received a unique dose of 5a) 0.6 mg/kg, 0.3 mg/kg, 0.15 mg/kg, or 5b) 0.075 mg/kg of artesunate (AS) are shown. We infected mice with the Uganda Palo Alto Marburg (FUP/CB or PAM) progenitor strain before it was subjected to any drug pressure. Arrows indicate day of intravenous drug delivery. In panel a, day 0 represents the fourth day post-inoculation of mice. Results were reproducible in several mice treated ate ach dose
Parasites host and host cell lines:
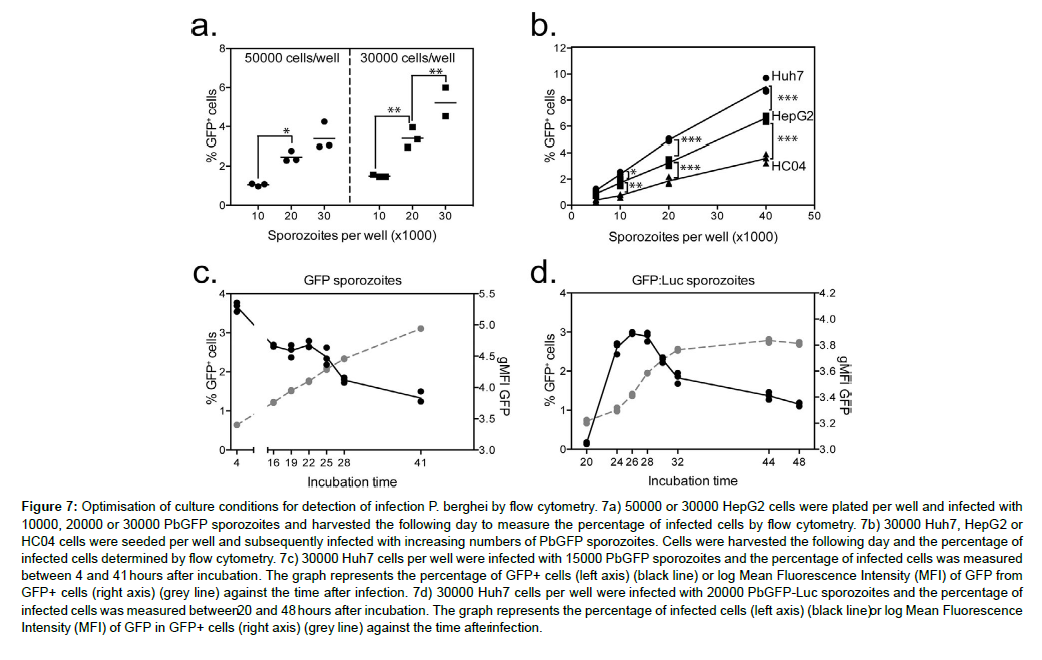
Plasmodium berghei is the first parasite has the frequently used wild-type strains NK65 and ANKA, as well as the green fluorescent strain and other transgenic strains. The P. berghei ANKA wild-type clone 2.34, as well as the gametocyte nonproducer 2.34, are often used strains. Parasites, Hosts, and Host Cell Lines 54 The GFP-expressing line 507 clone1, which stably expresses GFP but does not include the TgDHFR-TS drug resistance gene as a selection marker, was developed by provides a comprehensive database of available. HepG2 cells are available from a variety of sources, including ATCC and the Health Resources and Services Administration. H.P.A. Microbiology Services, Porton Down, Salisbury, Wiltshire, SP4 OJ6, UK. Protection Agency Culture Collections (H.P.A. Microbiology Services, Porton Down, Salisbury, Wiltshire, SP4 OJ6, UK). We discovered no changes in susceptibility between HepG2 A16 and other HepG2 cell lines, despite some authors suggesting that sub clone HepG2 A16 is a better option. Commercially available Drosophila Schneider’s-2 (S2) cells are available from a variety of sources (e.g., life technologies, 1600 Faraday Ave., Carlsbad, CA 92008, USA). Tuck-Ordinary (TO) or CD-1 mice, >5 weeks old, for normal maintenance and mosquito infections C57BL/6 mice for bite back infections; C57BL/6 mice are extremely vulnerable to sporozoite infections [9, 10]. Mosquitoes are number five. Anopheles gambiae, e.g., G3, L3-5, Yaoundé, N’Gousso; Anopheles stephensi, e.g., sda500 (very susceptible); Anopheles gambiae, e.g., G3, L3-5, Yaoundé, N’Gousso. Anopheles gambiae susceptibility in our lab is a factor of ten. that of A. stephensi [78].
Culture media
Essential Minimal Medium (MEM, Invitrogen). 10 percent heat-inactivated foetal calf serum (FCS, life technologies), 50 units/ ml penicillin, 100 g/ml streptomycin, 50 g/ml neomycin, 1 mM L-glutamine, and nonessential amino acids are added to the culture medium for HepG2 cells and exoerythrocytic stage cultures (Flow mixture). Filter-sterilize and store at 4 degrees Celsius. Culture media for Schizont (bloodstage) (modified from 11). To 500 ml of RPMI1640 (life technologies) containing 25 mM HEPES, 2 percent w/v NaHCO 3 and L-glutamine, add 25 units/ml and 25 g/ml streptomycin (2.5 ml 100 penicillin and streptomycin, life technologies). Add 20% heat-inactivated FCS to make a complete medium (life technologies). Culture medium for ookinetes. In 1 L, combine 16.4 g RPMI, HEPES, and L-glutamine (Sigma-Aldrich), 2 percent w/v NaHCO 3, and 0.05 percent w/v hypoxanthine (Sigma-Aldrich) (Sigma-Aldrich), 100 M xanthurenic acid (XA, Sigma-Aldrich) (see Note 1), 50 units/ml penicillin, 50 g/ml streptomycin (life technologies, 100 penicillin and streptomycin), pH 7 [79 , 80].
Filter-sterilize and keep for up to 6 months at 4°C. Just before usage, the complete medium is supplemented with heat-inactivated FCS (life technologies) to a final concentration of 20%. S2 culture medium [12] is a type of medium that is used to grow bacteria. Schneider’s insect media (appropriate for insect cells, Sigma-Aldrich), 50 units/ ml penicillin (Sigma-Aldrich), Schneider’s insect medium (suited for insect cells, Sigma-Aldrich), Schneider’s insect medium (suitable for insect cells, Sigma-A 5. Maintenance of Rodent Malaria Parasites in the Laboratory 55 Aldrich) and 50 g/ml Streptomycin. Filter and store at 4°C after sterilisation. Before using, add a ten percent heat-inactivated FCS supplement [81].
Culture medium for oocytes. 0.06 percent Para Amino Benzoic Acid (PABA), 0.05 percent w/v hypoxanthine, 0.2 percent w/v sodium bicarbonate, and 2 percent v/v lipoprotein-cholesterol solution (Sigma-Aldrich) 50 units/ml penicillin, 50 g/ml streptomycin, 200 g/ ml gentamycin (Sigma-Aldrich) (pH7). Filter-sterilize and store at 4 degrees Celsius. To obtain a complete medium, add 15 percent heat in activated FCS [82].
Methods Maintenance in Vivo-In Vitro:
Production of P. berghei Blood Stages in Mice
Load a 1-ml syringe with a 30G needle with a cryovial containing frozen P. berghei parasites (from a sporozoite-infected mouse = passage zero). Inject up to 200 l i.p. into the mouse and care for it according to national animal care guidelines. Take a tail smear 2 to 3 days after inoculation to check infection progress. The mouse can get cerebral malaria and/or die if the parasitemia is high or the infection period is protracted. On a daily basis, visually evaluate mice for inactivity, separation from cage mates, and ruffled fur. These mice must be employed right away or euthanized. With increased passage numbers, however, the parasite “senescence” (e.g., telomere degradation) occurs. We don’t go beyond mechanical blood passage 8 as a rule of thumb to keep gametocyte production unaffected. The rodent malaria parasites can be frozen and preserved if used only seldom (Figure 6).
Figure 6: Inhibition of the in vitro development of blood stages of Plasmodium berghei by chloroquine, artesunate and pyrimethamine. Inhibition of development was determined by measuring the rate of DNA synthesis using flow cytometry (FC assay) and by measuring inhibition of luciferase expression in parasites during development from ring forms into mature schizonts in culture. 6a) Comparison of the in vitro drug luminescence (ITDL) assay and FC for two transgenic lines: 875m1cl2 (selectable marker free line)a nd 354cl4 (contains the pyrimethamine resistant tgdhfr/ts selectable marker). In each graph the EC 50 values of both assays are shown. 6b) Comparison of the ITDL assay, performed in 24-well or in 96-well culture plates (parasites of line 875m1cl2). In each graph the EC 50 values of both assays are shown. 6c) Comparison of the ITDL assay in 96-well plates with and without storage of the culture plates at À20 °C. Plates were stored at À20 °C for either 24 h (a,b; line 354cl4) or 1 week (c,d; line 875m1cl2).
Production of P. berghei
Gametocytes in Mice:
Infect mice with P. berghei that has not been passed through a mosquito more than eight times.When asexual parasitemia reaches >1%, collect infected blood via cardiac puncture and inject 200 l (10 6– 10 8 infected RBC) into a donor mouse that has been given phenylhydrazine i.p. for 3 days to induce reticulocytosis (P. yoelii, P. vinckei, and P. chabaudi) infect mature RBC, so induced reticulocytosis is not An asexual parasitemia of less than 10% (1–1.0%) at day 3 postinoculation is appropriate for mosquito infections with P. berghei (both direct and membrane feeds). To create highly enriched gametocytes, treat animals with sulfadiazine (10 mg/l) in drinking water for two days prior to bleeding. Take a tail smear and Giemsa stain it 3-8 days after infection. Examine the gametocytes for mature male and female gametocytes. Around 8 days following infection, maximum gametocyte densities are reached [8]. Ex flagellation testing can be used to confirm the functional maturity of male gametocytes (Figure 7) [83].
Figure 7: Optimisation of culture conditions for detection of infection P. berghei by flow cytometry. 7a) 50000 or 30000 HepG2 cells were plated per well and infected with 10000, 20000 or 30000 PbGFP sporozoites and harvested the following day to measure the percentage of infected cells by flow cytometry. 7b) 30000 Huh7, HepG2 or HC04 cells were seeded per well and subsequently infected with increasing numbers of PbGFP sporozoites. Cells were harvested the following day and the percentage of infected cells determined by flow cytometry. 7c) 30000 Huh7 cells per well were infected with 15000 PbGFP sporozoites and the percentage of infected cells was measured between 4 and 41 hours after incubation. The graph represents the percentage of GFP+ cells (left axis) (black line) or log Mean Fluorescence Intensity (MFI) of GFP from GFP+ cells (right axis) (grey line) against the time after infection. 7d) 30000 Huh7 cells per well were infected with 20000 PbGFP-Luc sporozoites and the percentage of infected cells was measured between2 0 and 48 hours after incubation. The graph represents the percentage of infected cells (left axis) (black line)o r log Mean Fluorescence Intensity (MFI) of GFP in GFP+ cells (right axis) (grey line) against the time afteri nfection.
Infection of mice with sporozoites infection by mosquito feeding (Bite-Back):
Depending on the species, age, and treatment, starve mosquitos for a few hours or overnight. However, drink plenty of water to stay hydrated. The next day, do a direct feed on a naive C57BL/6 mouse that has been anaesthetized. Feed 5 P. bergheiinfected mosquitoes to each mouse for 10–20 minutes (this ratio implies 200 sporozoites per bite and 1,000 sporozoites provide a 94% chance of a blood-stage infection [13]. In P. yoelii (10 i.v. route) and P. chabaudi (400 i.p. route), lower sporozoite counts allegedly achieve equivalent transmission efficacy [14]. After feeding, place mouse under a warm heat lamp or on a heat pad to recover, and keep an eye on it until it has recovered. Begin taking blood samples from mice on day 3 after feeding to look for asexual behaviour. Blood infection, or as the parasite line allows (for example, in vivo luminescence [15]. Pass blood from this mouse (P0) or freeze it Mice are susceptible to cerebral malaria after bite-back infections.
Tail vein injection of sporozoites:
Dissect mosquitos (“Mosquito Dissection to Isolate Mosquito Salivary Glands”) and store sporozoites on ice until ready to use. Preheat mouse to 37°C for 10 minutes. Restrain the mouse, sanitize the tail with 70% ethanol, and use a 30G needle to inject at least 1,000 sporozoites (P. berghei) into the vein around the middle of the tail. Use the smallest amount of suspension possible and inject it slowly (rapid injection provokes profound vasoconstriction).
Maintenance of P. berghei in Mosquitoes
Maintenance of Anopheles stephensi:
There are other laboratory colonies; we use one that has been around for a long time. Feldman’s sda500 chosen line has given rise to a colony. Ponnudurai [16] is another name for Ponnudurai. A simple description of how to maintain a colony is available. The colony is kept at 28°C and 80% Relative Humidity (RH) on a 12/12 day/night cycle, with a 45-minute ramp up/down in light intensity at twilight and dawn. Remove the egg dish from the mosquito cage and wash the eggs and L1 larvae from the filter paper in new Reverse Osmosis (RO) water (if using chlorinated tap water, leave out to air for at least 24 hours before using to allow the chlorine to evaporate). Remove any dead adults from the surface and feed with two drops of Interpret Liquifry No1. Feed larvae a locally accessible substance from day 3 onward; we use pelleted fish meal suitable for outdoor ponds—these foods rarely cause bacterial overgrowth, simplifying feeding regimens; many others use powdered fish food. The dosage is calculated by ensuring that the larvae “nearly finish” the food in a 24/48-hour period. Healthy larvae respond to movement, and the water is clear but contains bacteria, protists, and rotifers from your local ecology. The bacterial flora that results in the mosquito’s gut can have an impact on the malaria parasite’s development in the vector. When the larvae have reached the L2 stage, dilute to 1/ml density and feed as previously 5. Pupae appear on day 8 and must be removed on a daily basis (within 48 h they will emerge as adults). These can be gathered using a variety of methods, which are mostly governed by the amount of biomass produced. As a result, we collect individual pupae using simple vacuum collection into a 5 L Erlenmeyer/ Buchner fl ask at a rate of 2,000 per day. When the pupae are full, gather them in a sieve, transfer them to clean dishes, and place them in a mosquito breeding cage (25–40 cm 3). During blood feeding and egg collection, remove or cover any pupal bowls. Take care of the adults as directed. Feed an appropriate blood source once a week; we utilize sedated rats for 1–3,000 adults. To collect (and remove) discharged blood from mosquitoes and urine from rats, cover the cage’s base with absorbent paper. Keep the cage clear of dead mosquitoes and blood (which attracts fungus, mites, and ants, all of which can jeopardize the colony’s survival) [16].
The day after you’ve eaten, make a 3 cm of clean RO water in a clean egg bowl (7 cm diameter) in the cage. Cut the point off a cone-shaped piece of paper. Insert into the bowl such that when open, the cone fills the bowl’s surface and the cone’s core meets the water. Allow for the eggs to be placed on the moist paper/water surface for 2–3 days.
Clean all containers on a regular basis, avoiding detergents if feasible. Staff should avoid wearing fragrant cosmetics and (obviously) coming into touch with household insecticides.
Direct feeding on malaria infected mice
Treat a mouse with phenylhydrazine i.p. six days before feeding the mosquitoes. Infect mice i.p. with parasitized RBC three days before feeding while the highest gametocyte densities are found on day 8 after vaccination, day 3 has been found to be the best period to obtain high oocyst yields. Place a warm container on one side of a mosquito cage (4–7 days after emergence) one day before feeding. Female mosquitoes are drawn to heat sources and can be identified by sucking them into a “pooter.” Place the insects in a suitable container and line it with filter paper to absorb the blood the mosquitoes produce while feeding. Mosquitoes love paper soup containers as mosquito cages are content with densities ranging from 0.5 to 1/ml. In the 12–24 hours before the blood feed, do not feed mosquitoes sugar, but keep them hydrated with water. Reduce the time the mosquitos are starved if they are vulnerable owing to age or treatment, or if certain strains are present. On the day of the meal, you may want to use a Giemsa-stained blood film to record the mouse’s parasitemia and/or gametocytemia (see Subheading “Giemsa Staining of Thin Blood Smears”). Testing for exflagellation as a potential sign of the parasite’s infectiousness is also useful. Anesthetize mouse: make sure that the mouse is deeply anesthetized and place it on the netting of the mosquito cage, taking care not to restrict its breathing. Keep the mouse warm with cotton wool (or a heater blanket) if it is small. Maintain the feeding mosquitoes at 19–21°C, in a draft-free, darkened environment for a minimum of 15 min (or until the appropriate number of mosquitoes have fed). A dark red light can be used if it is necessary to observe and record the feeding process. After feeding, there may be a pool of sticky blood on the bottom of the mosquito pot. Lay the pot on its side and gently tap to detach any stuck mosquitoes and maintain like this at 19–21°C and 70–80% RH overnight. After this time the blood has dried, the pots may then be returned to the vertical without fear of loss of blood-fed mosquitoes [83 ].
Engorged females are very delicate; therefore, avoid handling them if at all possible for 24 h. The day after feeding you may wish to remove unfed or partially fed (less than ¾ engorged) mosquitoes. Two methods may be used. A. stephensi previously starved for 24 h can be further starved for 48 h (but keep hydrated). Mosquitoes that have not taken a blood meal will usually die. This simple method will however not guarantee that all the unfed mosquitoes are removed. Alternatively anesthetize the mosquitoes with CO2; while asleep, transfer to a Petri dish on ice and remove unfed females (whilst not disturbing fed mosquitoes). Transfer remaining fed mosquitoes back into pot. Some losses must be expected. Feed mosquitoes with fructose/ PABA (replaced every 2–3 days) and maintain at 19–21°C (P. berghei), 25–30°C (P. chabaudi), and 24°C (P. yoelii; P. vinckei), 70–80% RH for the desired period (24 h for ookinete studies; 8-12 days for oocyst counting; 18-21 days for counting of salivary gland sporozoites and infection of mice). The variable temperature tolerances of mosquito infections of P. berghei as they mature have been recorded. A very significant boost in sporozoite numbers can be achieved by feeding the infected mosquitoes on a naïve mouse on/ around day 7 post infections [84].
Membrane feeding:
Instead of feeding directly on an infected mouse, there are numerous reasons why one would need to feed on direct replicates of artificial mixtures of infected blood and added reagents. To do this, a series of membrane feeders is ideal. Membrane feeds are the only method by which to initiate infections. Whilst this procedure is easily described we find the success achieved is highly operatordependent significant variation in success between laboratories is therefore not unexpected, and is commonly observed. Prepare mice and mosquitoes as described in Subheading “Direct Feeding on Malaria-Infected Mice”. Warm up membrane feeders to 37–39°C and maintain at this temperature throughout. If using Para film, no more than 5 min before adding the blood, stretch the membrane (Baudruche membrane or 2-way stretch Para film—the latter stretched to the point of breaking in both directions) over the feeder and secure well. Para film membranes rapidly become fragile. Baudruche membranes can be applied at any convenient time. Para film membranes rapidly become fragile. Baudruche membranes can be applied at any convenient time. Anesthetize the rodent deeply and collect blood as rapidly as possible. Keep blood at 37°C (for short periods) or rapidly cool to 0°C (for greater periods, e.g., >30 min of manipulation). Introduce gametocyte-infected blood, or ookinete culture at 30–50% hematocrit into the feeder. Put feeder in contact with the mosquito pot netting. Breathe gently on the pot to stimulate mosquitoes and allow feeding to continue for a minimum of 15 min. There is no effective time limit on the feeding of ookinete cultures, but beware as these infections can yield high parasite load. Significant mosquito mortality over the succeeding 48 h may be induced. After feeding, treat mosquitoes as described in Subheading “Direct Feeding on Malaria-Infected Mice” [85].
Maintenance in-vitro
P. berghei is the only malaria species for which every stage of the life cycle has been grown to maturity in vitro. The chronology of these achievements is as follows (naming ex vivo progenitor–in vitro product): gametocyte–ookinete [18], sporozoite merozoite [19 , 20], trophozoite–gametocyte [11], sporozoite–gametocyte [1], gametocyte– sporozoite [2]. To date, the profound inefficiencies of sporogonic culture have prevented the routine linkage of the methods of Suhrbier and Al Olayan.
Cultures of Exoerythrocytic Stages:
Exoerythrocytic stages of P. berghei can be cultured in the human cell line HepG2, and in other human cell lines [21, 22]. These are more convenient host cells than the primary hepatocytes from the mouse or rat [23], or the taxonomically “correct” Thamnomys [24].
Culture HepG2 cells in MEM freshly supplemented with 10% FCS, penicillin 50 μg/ml, streptomycin 100 μg/ml, neomycin 50 μg/ml, and media supplements (L-glutamine, 1 mmol/l; 2. nonessential amino acids (Flow mixture); glucose 3 mg/ml) in 25-cm 2 flasks at 37°C in air containing 5% CO2. Split the cells into appropriate vessels when they are semicon fl uent. Remove the media and rinse the cells with 0.05% trypsin/EDTA. Following addition of 0.25% trypsin/0.02% EDTA let the fl ask sit for a few min at 37°C until the cells are detached. Remove supernatant (containing detached cells) and wash in complete medium. Split 1:4–1:6. Seed in 24-well plates at 1–2 × 10 5 cells per well and culture for 48–72 h until confluence. Irradiate the cells with 3,000– 3,500 rads from a Cobalt 60 source to reduce growth rate Replenish medium following irradiation. Very briefly immerse mosquitoes (21– 35 days postinfection) in 70% ethanol and allow to dry (on ice) in a sterile atmosphere. Dissect out salivary glands in supplemented MEM ( see Subheading “Mosquito Dissection to Isolate Mosquito Salivary Glands”); for each well of a Costar 24-well plate, use two infected A. stephensi mosquitoes.
Transfer salivary glands into homogenizer and release sporozoites (“Observation of Salivary Gland Sporozoites”). Estimate sporozoite numbers using a hemocytometer. If necessary, dilute sporozoites. Remove medium from HepG2 cultures completely and in the case of Costar 24-well plates, add 1–4 × 10 4 sporozoites/well (150–200 μl of suspension) to each well. Incubate for 2 h at RT. Add fresh medium and transfer to a 37°C incubator gassed with 5% CO 2 in air. Fully mature schizonts can be seen 45–48 h after sporozoite inoculation and by 60 h, the majority of Exo-Erythrocytic (EE) stages should be mature schizonts [23]. Rupturing hepatocytes can often be seen lying above the plane of the attached cells. Change medium twice a day. Examine EE parasites as required by the experimental protocol, e.g., confocal laser scanning microscopy. For classical morphological studies, use monolayers that are fixed in Bouin’s fixative and subsequently staine
Culture of blood stages:
Cultures of asexual blood stages of P. berghei can be initiated from infected mouse blood or from cell cultures containing mature EE schizonts. For the latter, exchange HepG2 culture medium for RPMI 1640 supplemented with 20% inactivated FCS, 5.94 g/l HEPES, 2 g/l sodium bicarbonate (pH 7.2) [ 26] and change the gas to 4% CO 2, 4% O 2 , 92% N 2. Prepare reticulocytes from a Wistar rat injected with 120 mg/ kg body weight phenylhydrazine 4–5 days prior to harvest. Harvest reticulocyte-enriched blood by cardiac puncture and remove the white blood cells (see Subheading “Removal of Leukocytes from Whole Blood”). Wash twice in RPMI 1640, recover RBC at 500 × g for 10 min. For a 10-ml culture of EE schizonts, add 25 μl of a packed reticulocyte suspension to the infected HepG2 cells. Using a magnetic stirrer, stir the culture at 400 rpm at 37°C (to induce release of merozoites). After 12 h, centrifuge mixed cell suspension at 500 × g and add the RBC pellet to a fresh flask containing pre-equilibrated and supplemented RPMI 1640. Gently and continuously stir RBC to maintain cells in suspension (50 rpm). Replace medium every 12 h and gas the culture. Add fresh reticulocytes 22 h after transfer. Stir at 400 rpm for 5 min to initiate a new round of schizogony. Repeat step 8every 25 h. Mature gametocytes can be seen in cultures >24 h after setup [Figure 8].
Figure 8: Progress of parasitaemia in Plasmodium berghei -infected mice treated with A chloroquine (CQ); tigecycline (TG) once daily dose; C tigecycline (TG) split dose; and, D combination of tigecycline (TG) and chloroquine (CQ). Each point represent value mean ± SD of five mice or the number of mice remaining live at that point of time. The numbers shown along each graph show the daily dose of the specifiedd rug. The mice were treated daily with dose of the drug indicated, for four days staring from day 0 (within 1–2 hours after inoculating the mice with P. berghei parasitized erythrocytes.
Culture of erythrocytic schizonts (modified from):
Gas 50–100 ml complete schizont culture medium with 5% CO 2, 3% O 2. Bleed mouse with a maximum of 3–5% parasitemia and add blood to medium. Gas-culture again and culture schizonts at 37°C while being shaken gently at 50 rpm for 20 h. Pellet culture at 500 × g. Discard all of supernatant except 1 ml. Resuspend the pellet in the remaining liquid and layer on top of a 55% Nycodenz/PBS cushion. Centrifuge at 300 × g for 25 min at RT using the lowest acceleration possible; the spin has to end without using any brake. Isolate parasites at the interface. Wash parasites with schizont culture medium and spin 10 min at 500 × g. Merozoites can be released by stirring the schizontinfected RBC with a magnetic stirrer [86F].
Ookinete culture:
Passage 200 μl heavily infected blood into mice treated 3 days. Previously with phenyl hydrazine. On day 3–8 post infection, check for gametocyte abundance and maturity by exflagellation. Bleed mice by cardiac puncture into complete ookinete medium so that blood is diluted 1:20–1:40 and place in vented tissue culture flasks. Optional: mouse white blood cells can be removed by passing culture immediately through a CF11 (Whatman) cellulose at 4°C or Plasmodipur filters (Euro-Diagnostica). Delays of 15–60 min can totally prevent ookinete formation, because the motile male gametes are released in the column and are retained. Store culture at 19–21°C in air for 22–24 h. If required, recover culture pellet following centrifugation at 500 × g for 5 min. Resuspend pellet and dilute 1:4 in an appropriate medium and count ookinetes in a hemocytometer at 400× (40× objective, 10× ocular) magnification [ 87].
Oocyst and sporozoite culture:
S2 cells are cultured at 19 ± 1°C in complete Schneider’s insect medium. Prepare ookinete cultures as described in Subheading 3.2.4 and purify using a Nycodenz cushion — all under strict sterile conditions. Maintaining sterility, pipette 90 μl of cold Matrigel into each well of a Lab-Tek 8-well chamber slide. Allow Matrigel to settle at 37°C for 30 min. Mix ookinetes and S2 cells in a 1:10 ratio using 10 4 ookinetes/ chamber in complete oocyst culture medium. Pipet mixed cell suspension onto solid Matrigel. Incubate plates at 19 ± 1°C in air. Replenish S2 cells every 48–72 h. Within 1–2 days, young oocysts can be observed on the surface or within the matrigel. By day 20, the fi rst sporozoites are released. Sporozoites can be collected from the supernatant and are infectious to mice [88 ].
Sundry Methods:
Cardiac puncture of mice:
Inject 15 μl/g body weight of Rompun/Ketamine anesthetic intramuscularly (i.m.) into the thigh(s) of the mouse using a 30G needle; there may be local bleeding. The animal may become briefly hyperactive, but thereafter anesthesia is deep and thus suitable for cardiac bleeds or for exposure to mosquitoes. Anesthesia can persist for up to 45 min. Wait until the pain reflexes of the mouse cease and lay the mouse on its back. Prepare a 1-ml syringe attached to a 26G needle containing 100 μl heparin (300 units/ml). Spray the skin with 70% alcohol; locate the heart (beat) with your fingers and then insert the needle about 5 mm into the mouse usually just to the right of the sternum between the second and third ribs. It may be necessary to use a quick stabbing action to ensure the tip of the needle penetrates the heart (and does not simply push it aside). Gently retract the plunger to con fi rm that the needle is in the bloodstream and then inject the heparin into the heart. Wait ~15 s and then gently withdraw the blood. The more gently this is done the more blood is finally harvested [89 ].
Blood smears:
Restrain mouse in an approved manner. We carefully abrade the skin on the tip of the mouse tail and with a gentle squeeze, transfer a small drop of blood (approximately 1 μ l) onto a glass slide. Quickly rest the edge of another glass slide just ahead of the drop of blood. Gently draw back the top glass slide and then allow the drop to disperse fully along its edge. Immediately, and firmly sweep the slide forward, drawing the blood along and forming a thin layer. Air-dry slide (an electric hair dryer, or fan heater is very useful to obtain rapid drying and hence optimal morphological preservation) [90].
Fixation and staining methods
Giemsa staining of thin blood smears:
Dilute concentrated Giemsa stain (modified solution, Fluka) to 10% (EE stages) or 20% (all other stages) in Giemsa buffer (0.7% w/v anhydrous KH 2 PO 4, 1% w/v anhydrous Na 2 HPO 4). Fix blood film in methanol for ~20 s and tip off excess methanol (it is better not to let the methanol evaporate fully). Either place individual slides face down on the surface of the stain, or if handling a batch of slides stain vertically in a Coplin jar—this is to avoid precipitated stain spoiling the final preparation. Stain exoerythrocytic stages for at least 45 min up to overnight and all other stages 10–20 min. Rinse slides very briefly in tap water (or Giemsa buffer if the tap water is acidic) and air-dry. Old 40 slides can be re fixed and stained, but the end result never surpasses the original [91].
Bouin’s fixation of exoerythrocytic stages:
Rinse cultures in multi well slides or on coverslips brie fly in PBS. Fix for 10–30 min in Bouin’s fluid (5% acetic acid, 9% formaldehyde, 0.9% picric acid, Sigma-Aldrich). Stain in 10% Giemsa stain overnight. Wash briefly in Giemsa buffer, and then treat with 60% acetone in water to enhance differentiation Wash/rinse further for 20 s each in 100% acetone, Histo-Clear (National Diagnostics), and Euparal essence (Australian Entomological Supplies). Mount preparations in Euparal Vert (Australian Entomological Supplies) [92].
Red blood cell lysis:
Method A:
Resuspend pellets of asexual parasites or ookinetes in cold 1x RBC lysis buffer. Incubate on ice for 20 min.Spin cells for 5–10 min at 500 × g at 4°C and discard supernatant. Wash the cells if necessary twice using PBS or culture medium.
Method B:
Resuspend pellet of RBC in 10 volumes of Gey’s working solution and hold on ice for 1–3 min, shaking occasionally. Stop lysis by adding Iscove’s Modified Dulbecco’s Media(IMDM, life technologies) containing 5% FCS. Wash again with IMDM [93F].
Observation of Mosquito Stage Parasites Dissection to Isolate Mosquito Midguts
Anesthetize mosquitoes with CO 2 and keep immobile on ice. Place one mosquito onto microscope slide beside a drop of PBS. Hold the thorax with a 26G needle or a pair of fi ne forceps, pull on the penultimate abdominal segment gently using another 26G needle or fi ne forceps to gently withdraw the midgut, and ensure that the gut makes contact with the PBS drop. If necessary, cut off the Malpighian tubules and terminal segment, and the foregut (if it has not already snapped clear of the body) [94].
Observation of Ookinetes from Mosquitoes:
24 h after blood feeding, knock out mosquitoes with CO2 and transfer to a Petri dish on ice. Dissect out blood- filled midgut (which is very delicate if fully engorged!) into a very small drop of ookinete medium (instead of PBS). With a very sharp blade make an incision in the midgut lying in the drop of ookinete medium. Gently tease the blood clear of the mosquito tissue and stir gently to produce a homogeneous suspension. If required, now make a blood smear and Giemsa stain. Alternatively, make a dilute suspension and observe directly by phase/ interference contrast microscopy, or other methodology. If observation of the (fixed) mid gut epithelium is required, it is easy to remove the blood meal after fixation in 4% formaldehyde for 45 s; the blood bolus is more cohesive which facilitates its removal [95].
Observation of Oocysts on Mosquito Midguts
On days 8–12 after feeding, dissect mosquito midguts in either PBS or 1% mercurochrome in PBS Observe by light, phase, or interference microscopy or, if using fluorescent reporter lines or tagged parasites, by fluorescence microscopy. Midguts can be fixed 30 min in 4% formaldehyde/PBS. Fixed midguts can be mounted in VECTASHIELD (Vector Labs) or in other mounting media. If a GFP-expressing parasite strain is used, mosquitoes can already be dissected on day 7 and GFPexpressing oocysts observed immediately by fluorescence microscopy. Alternatively midguts can be fixed as above and observed at convenience [96, 97]. To count fluorescent oocysts, we refer the reader to the method. The algorithm for the semiautomated counting of microscopic images is available free of charge from the authors. Observation of Midgut Sporozoites [98]. Using the rearing protocol described above, on day 15–21 after feeding, dissect mosquito midguts as described in Subheading “Dissection to Isolate Mosquito Midguts” into PBS or RPMI. Transfer ~10 guts into a 1-ml glass homogenizer in 200 μl PBS or RPMI and homogenize with a few strokes [99 ]. The pestle should be a loose fi t, and the strokes gentle, to ensure that the sporozoites themselves are not homogenized. Take homogenate and count sporozoites as required, e.g., in a hemocytometer (after allowing them to settle for 15 min), or if appropriate by flow cytometry. Preparation & administration of doses (Figures 9 and 10).
Following parameters were analysed in Complete Blood Count (CBC):
White Blood Cells (WBC) count: WBC count signifies the number of white blood cells in the blood in cells per microliter (μl) [100, 101]. The cells in the WBC differential count are typically listed separately. Red Blood Corpuscles (RBC) count: RBC count measures the number of Red Blood Corpuscles in a volume of blood and it is usually million cells per microliter (μl). Haemoglobin (HGB) Concentration: HGB Measures the amount of haemoglobin molecule in a volume of blood in grams per deciliter (g/dL) (one-hundredth of a liter) [102, 103]. Hematocrit (HCT) value: HCT value signifies the percentage of the whole blood occupied by Red Blood Corpuscles. Platelets (PTL) Count: It measures the number of platelets in a volume of blood in per microliter (μl). A low platelet count (thrombocytopenia) may also be detected in the complete blood count [105]. Mean Corpuscles Volume (MCV): MCV is the measurement of the average size or volume of a typical red blood cell in a blood sample in femtoliters (fL) (a fraction of one-millionth of a liter) [106, 107]. Mean Corpuscular Haemoglobin (MCH): MCH measures the amount of haemoglobin in an average red blood cell in pictograms (pg) (a small fraction of a gram) [108, 109]. Mean Corpuscular Haemoglobin Concentration (MCHC): MCHC measures the average haemoglobin concentration in a volume of blood gram per decilitre (g/dL) [110, 111].
Observations
Percent parasitaemia:
Percent parasitaemia was calculated by recording the number of parasites in nearly 10-50. Percent parasitaemia was recorded from day 7 to day 25 (Since the mice in positive control survived average approximately 25 days) or till death of mice after each 48hr.
Percent suppression:
The suppression in parasitaemia with respect to control group was determined after recording the parasite counts for different dose groups. The relative percent suppression with respect to the control group was used. Weight of mice: Weight of each mice before infection (day 0) and day 7 to day 25 or till death of mice after each 48hr. Mean Survival Time (MST): Mean Survival Time is the arithmetic mean of the survival time of different mice used in a particular experimental group. The day of death of mice was recorded once a day between 9- 10 A.M
Experimental A.
Handling of mice B. passing of mice plasmodium voelli C. Intra mascular injection of arthemethin D oral dosing of Chloroquine E. weighing of mice (Figure 12)
Staining of blood sample (Figure 13)
Different stages of Plasmodium yoelii in blood smear (Figure 14)
Experimental findings laboratory rearing of Anopheles stephensi malaria mosquitoes and swiss albino mice (mus musculus)
Since work is related with malaria, so it was important to know the detail life cycle Anopheles stephensi (L.) in the laboratory as a part of experimental protocol.
Rearing of Anopheles stephensi:
The laboratory culture of Anopheles stephensi (L.) was done under optimum environmental conditions. The larvae were collected from river pockets from nearby village of Bedla and different other locations of Udaipur district and cultured in the laboratory to establish pure line culture.
Eggs:
In the laboratory total numbers of eggs laid by five females were 247, 325 and 164 after 24, 48 and 72 hours respectively, with an average of 147.2 eggs per female after 72 hours. The incubation period ranged from 2-3 days, with an average of 2.30 days.
Larvae:
There were four larval instars in the life cycle of Anopheles stephensi (L.), with an average of 14-16 days, as reported earlier by many workers under optimum abiotic conditions. In the present study larvalperiod ranged from 10-13 days with an average of 11.60 days at an average of 27.92°C temperature and 70.54 per cent relative humidity.
Pupae:
Pupal stage is the last aquatic stage of mosquito life cycle. It is a non-feeding stage, but marks the beginning of adult life and end of larval life. Biology of mosquitoes in the laboratory revealed an average of 2.40 days of pupal period at 28.06 degree temperature, and 69.29 percent of relative humidity.
Adult:
Adult is the reproductive stage of mosquito life cycle that lasts for 3- 6 days. Male and female depended on fruit juices for their development, but females need blood for the growth of eggs. The average adult life span noted was 4.60 days in the laboratory. The study in laboratory showed that the mean of total life cycle was completed in 20.90 days, with a temperature of 28°C and 70.08 percent relative humidity [112].
Rearing of Swiss albino mice:
Swiss albino mice were properly reread in the laboratory by providing following facilities and environmental conditions: The light cycle of 12:12 or 10:14 hrs (light: dark) was required for normal physiological and behaviour parameters of mice like regulating growth, metabolic, endocrine, and immunological parameters. light intensity for albino mice was best below 25lux for their normal behaviour, as well as progression of eye pathology and reproductive parameters. Comfort room temperature range for mice housing was between 20 and 26°C, this range is required for proper metabolism, cardiovascular function, motor activity, growth and development, consumption of food and water, haematology and serological parameters, susceptibility to toxins, sleep depth and behaviour. A relative ambient humidity for mice rearing was 55±15 percent for proper thermoregulation as well as for transmission of pathogens. Colorless, tinted transparent cages or white opaque cages are preferred for housing of mice and this cage design permits, mice in climbing which is a regular component of locomotor activity of mice. Pellet diet supplemented with soaked grains was found to be preferable and nutritive for mice. Mice are social animals and should, wherever possible, be maintained in stable, harmonious social groups. Proper housing allows mice the opportunity for social interaction, the opportunity to carry out normal behaviours and the opportunity to rest and withdraw from each other. Normal behaviours of mice include eating, drinking, urinating, defecating, foraging, exploring, gnawing, hiding, climbing, playing, nesting, digging and engaging in a range of social activities (Figure 15, 16, 17, 18, 19, 20) [113].
Result and Discussion
The metabolic stability of the primaquine–chloroquine hybrid positions was designed, synthesized, and investigated. Furthermore, because the electron-withdrawing effect of the para-quinoline amine reduces the nucleophilicity of the 4-amino-7-chloro-quinoline portion, it was shown to be unreactive in both reductive amination and nucleophilic substitution processes (route C). The next step was to look at methods A and D, which entail coupling of the side chain’s terminal amino group to the primaquine or chloroquine’s aminoquinoline core. Unfortunately, the nucleophilic substitution starting material necessary for route A was not readily available, making this method impractical.
Meanwhile, both of the route D precursors, 4,7-dichloroquinoline and primaquine (1), are commercially available. As a result, route D appeared to be the best option. Due to primaquine’s redox-active characteristics, limited yields of isolated product were obtained. Our efforts to improve the process revealed that nucleophilic substitution worked well at 120°C without the need of a catalyst. This new technique was less expensive and better suited to scaling up. Due to the reduced amount of reagents and side products, the product was also easier to purify. In rat liver microsomes, the hybrid 3’s metabolic stability was studied [114, 115]. A series of microsomal incubations with four different rat liver microsomes were used to determine the enzymatic stability. The various activity of the cytochrome P450 monooxygenases (CYP) and CYP isozymes characterise the microsomes used in the studies. The metabolization of the hybrid 3 was temporal and microsome dependent. The metabolic rate of the hybrid compound ranged from 20% (microsomes from female rats) to 80% after 90 minutes of incubation (microsomes from PB and bNF induced male rats). When ion pair chromatograms from microsomal incubations were compared to chromatograms from control samples, the number of extra peaks seen ranged from 9 (female rats) to 15 (microsomes from PB + bNF induced male rats) [116]. Two of the additional peaks were ascribed to the aminoquinoline moieties of primaquine and chloroquine, namely 6-methyl- 8-aminoquinoline and 4-amino-7-chloroquinoline, by cochromatography with the reference compounds. Because only two reference substances were available at the time, it’s unclear to what extent other additional peaks are hybrid 3 metabolites. Identifying the remaining peaks and assigning a value In a follow-up study, the metabolites will be studied. Pharmacokinetic investigations in vivo can be carried out once the principal metabolites and their conjugates have been identified [117, 118].
To test our hypothesis of integrating the activities of the two pharmacophores of primaquine and chloroquine into a single hybrid molecule 3, we looked at its effects on different Plasmodium stages in vitro and in vivo on several platforms. As a result, the hybrid 3’s effects on sporozoite gliding motility, liver-stage development within hepatocytes, asexual blood stages, and gametocytes were investigated. We also tested the drug in an in vivo P. berghei animal model to see if it has preventive (pre-blood infection) and curative (blood infection) efficacy against the liver and blood stages, respectively [119].
The hybrid compound 3 isn’t one of them. In vitro, it has a large influence on sporozoite motility but has little effect on hepatocyte invasion. In vitro, sporozoites exhibit gliding motility, which is a type of locomotive movement. By staining for the track of produced CSP, the GPI-anchored surface protein completely covering the sporozoite surface, we investigated the in vitro motility behaviour of the sporozoites under the influence of the hybrid. There was a significant or dose-dependent effect, according to the results. In addition, we tested the hybrid’s effect on parasite invasion in vitro, but the results were inconclusive and ineffective (Figure 21).
In vitro, the hybrid molecule has a strong inhibitory effect on liver-stage development.
In vitro, the hybrid compound exhibits strong inhibitory effect against liver-stage development. When a sporozoite invades a hepatocyte, it forms a sporozoite. The vacuole of a parasite changes into a round-shaped liver stage. We were able to test for action against the established hepatic stages pos invasion in human hepatoma cells by adding 3 to the media after sporozoite invasion. In comparison to untreated controls, we used immunofluorescence microscopy to examine the inhibitory effect of the hybrid on the morphology (size and shape) and developmental stage of liver stages. Under confocal microscope analysis, the diameter of the fluorescent signal produced by the liver-stage parasite was measured, and the number of parasites in each well was counted. When compared to the untreated control, the hybrid molecule 3 induced an overall decrease in the number of liver stages per well at 48 hours, implying that a therapeutic effect could be achieved. IFA was able to detect just a small percentage of parasites because they were completely destroyed or otherwise harmed. When parasite size was compared to the control, parasite size was found to be less [120, 121].
24 hours after invasion, the size of the uninhibited liver stage in the untreated control was reduced to 80% of its original size at 1 M, where 100% would reflect the mean size of the uninhibited liver stage in the untreated control. At later time periods, this mild suppression of liver-stage development became more significant, with a size of 46 percent recorded at a concentration of 1M, 48 hours after invasion, which is comparable to the inhibition seen with Primaquine at 10 M. (standard in vitro inhibitory concentration), The hybrid compound 3 displayed intermediate inhibition at 100 nM, with a size of about 60%. When seen as a whole, these findings show that the new hybrid molecule 3 has potential effects in vitro against the parasite’s liver stages, or pre-pathological stages [122].
Asexual blood stages, including Chloroquine-resistant strains, are active against the hybrid compound. Using the Malstat assay and the hypoxanthine incorporation assay, we examined the activity of the hybrid molecule 3 against the blood stages of three different Plasmodium falciparum strains: K1, Dd2, and 3D7. The former two are Chloroquine-resistant, whilst the latter is Chloroquine-sensitive. With an IC50 of 0.64 0.046 M, the hybrid 3 is active against 3D7. There were no extra or synergistic effects when Primaquine and chloroquine were used together at the same concentration (IC50 = 0.03 0.012 M).
Primaquine (IC50 = 3.11 1.536 M) has no synergistic effects when combined with other drugs. 3D7 is a 3D7 strain. As a result, the activity of 3 for 3D7 is lower than that of Chloroquine, falling somewhere between Primaquine and Chloroquine, implying that it is a less potent schizonticidal against 3D7. Surprisingly, 3 has an inhibitory impact against the chloroquine-resistant strain Dd2 (IC50 = 0.58 0.185 M), which is equivalent to its action against 3D7. The hybrid molecule is somewhat more effective than the combination of and (IC50 = 0.19 0.035 M). Surprisingly, the findings suggest that primaquine’s previously documented resistance-reversing action may also occur in the K1 strain. In comparison to 3D7 or Dd2 471 (IC50 = 0.08 0.0048 M), the hybrid 3 has extremely good and much better activity against this strain. It’s around six times as large more effective than primaquine (1, IC50 = 0.46 0.08 M) and chloroquine (2, IC50 = 0.146 0.02 M). The pharmacophore combination of Chlotoquine and Primaquine was likewise more effective than 3D7 and Dd2, but not as successful as the hybrid molecule (data not shown). The equimolar combination of both i.e. combined administration at similar concentrations (IC50 = 0.169 M), provided a modest extra impact, but was less potent than the hybrid compound 3. This is just another example of Primaquine’s resistancereversing ability (1). As a result, the hybrid 3 is the most active in the most resistant strain K1, outperforming the equimolar combination of mother medicines, Primaquine as well as Chloroquine [123, 124].
We share our findings in this thesis. The concept of a unique hybrid consisting of the pharmacophores Primaquine and Chloroquine coupled together in an authentic form without the introduction of new functional groups has been proposed for the first time. We provide evidence for varying activities against all stages of Plasmodium in the mammalian host in vitro (against liver-stage development, asexual and sexual blood-stage development), as well as demonstrate its prophylactic and therapeutic potential in vivo, in contrast to most previous publications. Since Primaquine is thought to be a pro-drug, its hydroxylated metabolites, such as quinone, are thought to be responsible for its mechanism of action which means the translational potential of our in vitro data to in vivo activity must be approached with care. Our hybrid shows varying but interesting activities against P. falciparum in vitro: it It shows a small intermediate activity against Dd2 and 3D7, but a strong activity against Chloroquine-resistant strain K1, indicating a resistance-reversion impact. Furthermore, our novel hybrid 3 has a high inhibitory effect against P. berghei asexual blood stages in vivo and an inhibitory effect against P. berghei liver stages in vitro, with a preventive effect seen in rodent experiments. This prophylactic impact did not result in complete eradication of intrahepatic parasites, but it did result in a prophylactic delay in clinical malaria onset. We choose the subcutaneous and intraperitoneal routes of administration because they are best defined in the Plasmodium rodent infection model, even though Chloroquine and Primaquine are commonly given orally in the field, and a human translational strategy would be more appropriate. This administration approach will involve field trials. The hybrid 3 was capable of completely preventing blood-stage patency in 66 percent of rats at the maximum dose supplied up to day 30 post-infection. This could be the case either to parasite eradication at the liver stage, or a reduction in liver load sufficient to diminish the amount of merosomes egressing from the liver to be destroyed by the immune system, or by the hybrid molecule itself Given that a single injection is enough to produce infection, the other scenario may be more likely. Indeed, the hybrid proved effective against chloroquine-resistant P. falciparum blood forms, with a significantly lower IC50 than strain K1, which is commonly utilised. P. falciparum strains that are resistant to chloroquine and pyrimethamine have been identified by research groups as the standard Chloroquine and pyrimethamineresistant P.
falciparum strain. This is noteworthy because the hybrid’s blood-stage action is conferred by the pharmacophore of Chloroquine. It is possible to speculate on the nature of this activity against chloroquineresistant strains. Due to an interaction with the PfCRT, the Primaquine pharmacophore component attaching more readily to its machinery than chloroquine due to its higher lipophilicity. Primaquine has previously been shown to be a chloroquine resistance reverser in P. falciparum. Primaquine is more effective in this regard than the first described’resistance-reversing agent,’ verapamil, in terms of preventing Chloroquine ejection and inhibiting -hematin crystallisation. Within the authorised therapeutic dosage of Primaquine treatment, it has been suggested that combining Primaquine and Chloroquine therapy could be a cheap and easy way to revive and extend the life of chloroquine in the field. Our hybrid proposes a new way to accomplish the same therapeutic goal using a single chemical with a single pharmacokinetic profile and half life.
As a result, the therapeutic potential of a primaquine–chloroquine hybrid 3 is significant. Effective parasite suppression in the liver targets the parasite at a developing bridge head, the rallying point before the erythrocyte attack. Targeting the parasite at this phase acts as a preventative measure to avoid clinical signs from developing. It has been established that Primaquine is a safe and efficient prophylactic drug.
Non-pregnant women and tourists with a normal glucose-6- phosphate-dehydrogenase level are protected from malaria. It may also give a solution to hypnozoite-forming Plasmodium infections, such as P. vivax, where recrudescence due to reactivation of dormant liverstage forms can occur months or years after infection. Aside from the obvious therapeutic potential of the action against pathology-inducing parasite blood stages, the hybrid’s small but apparent activity against gametocytes is intriguing and clinically relevant. Eradication of these forms would not only be curative, but it would also halt the vicious cycle of mosquito re-infection and prevent the spread of drug-resistant parasite genotypes. This synthesis’ activity is proof of concept. That inhibition is achievable, which opens the door for future synthetic improvements. The capacity of the primaquine–chloroquine hybrid 3 to inhibit the liver and blood stages of mammalian Plasmodium infection in vitro and in vivo is described for the first time in this paper.
Compounds (I and II) were employed as bio isosteres of antiinflammatory medications such as ibuprofen and diclofenac as dual-activity antimalarial treatments capable of killing the parasite in the human blood and blocking transmission, i.e., those that can target both asexual parasites and Plan our hybrids. They include the 2-(2-acetamidophenyl)-2,2-gem-difluoroacetamide (I) or 2-(2-acetamidophenyl)-2-oxoacetamide (II) moieties, which have previously been shown to have anti-inflammatory activity.26 To make scaffolds, the quinolinic pharmacophoric group of CQ was connected to linker groups containing 2–4 (CH2) units, yielding compounds 1–13. Compounds 14–21 were also made by directly binding the acetamide skeletons to PQ. The goal of this research is to find chemicals that can kill Plasmodium while also acting on the inflammatory process generated by malaria infection. Novel PQ-derived compounds could have a broad spectrum of activity against all types of Plasmodium involved in the biological cycle of malaria in the human host, and could offer new therapy options for P. vivax malaria. These PQ compounds can help prevent the spread of malaria.
Additionally, PQ is a parasite-prevention medicine that works against gametocytes, which are the sexual form of the parasite. The parasite’s gametocytes, which are responsible for its development, should be valued and required. The process of molecular hybridization entails joining two pharmacophoric groups from different chemicals to form a single molecule. This new molecule, which is now known as a hybrid, may have the same or better activity as the precursor compound. It can function through the same mechanism as the precursor drug or in distinct ways, allowing resistance mechanisms to be avoided. These traits are critical when it comes to getting medications for the treatment of endemic diseases in underserved communities, such as malaria sufferers. We’ve used the hybridization method extensively to create a variety of hybrids that are resistant to P. falciparum. A prototype was created after 22 CQ and sulfadoxine hybrids were designed. That was more effective than both of the precursor medications combined. 23 We discovered new compounds among the nonquinoline derivatives, namely inhibitors of the P. falciparum dihydroorotate dehydrogenase (PfDHODH) enzyme. These triazolo pyrimidine and pyrazolopyrimidine derivatives are prototypes for novel molecules to be synthesised. In vitro, both asexual and sexual P. falciparum blood stages, as well as P. berghei sporozoites and liver stages, are active against the hybrid molecules 3. The hybrid is active against P.berghei liver and blood stages in vivo. Our plan work has effectively validated the concept of combining distinct mechanisms of action to attack different plasmodium stages in the mammalian host with a single chemical. Our goal is that the innovative design of such a chemical will outsmart the pathogen in medication distribution resistances (Figure 22, 23).
Figure 22: Initial screening for anti-inflammatory activity of selected compounds on nitric oxide (NO) production by LPS (37.5 ng/ml) IFNγ (25 U/ml)-stimulated J774A.1 macrophages (A). Concentrationresponse curves for compounds 6 (B), 12 (C) and 20 (D) on NO production by J774A.1 macrophages. The results are represented by the mean SEM002C and significant differences from the positive control were determined by ANOVA followed by Dunnet’s post hoc test. ### P < 0.0001 compared to vehicle (0.2% DMSO) and *** P < 0.0001 compared to the positive control.
Figure 23: Effect of dexamethasone and compounds 6, 12 and 20 on LPS-induced TNFa production by J774A.1 macrophages. The results are represented by the mean SEM, and significant differences from the positive control were determined by ANOVA followed by Dunnet’s post hoc test. ### P < 0.0001 comparedt o vehicle (DMSO) and *** P < 0.0001 compared to the positive control.
Conclusion
The findings suggest a practical and fascinating strategy to developing new chemical entities for the treatment of malaria caused by Plasmodium falciparum and Plasmodium vivax, as well as the antiinflammatory mechanism associated with the condition. Twenty-one novel CQ and PQ compounds (1–21) were synthesised and evaluated in vitro against the CQR clone of P. falciparum (W2). With IC50 values ranging from 0.12 to 3.18 M, the carbonylated CQ derivatives 1–10 showed action. The most effective of the compounds in this series was compound 6 (n = 3; R = Cl). Compound 8 (n =4; R =H), on the other hand, was also powerful and had the best selectivity. When compared to carbonylated analogues, gem-difluorinated CQ derivatives (10– 13) showed no significant changes. When evaluating them as linkers based on carbon numbers, it was It’s impossible to argue that one series was much superior to the other. Carbonylated 14–17 PQ derivatives and gem-difluorinated 18–19 PQ derivatives were the least powerful CQ derivatives. The best of this series were compound 17 (R = Br) and its gem-difluorinated counterpart 21, which had IC50 values of 2.50 and 3.50 M, respectively. When employed at a high dose (50 mg/ kg), compound 20 (R = Cl) showed strong transmission inhibition of the malaria sporogonic cycle in mosquitoes, compared to PQ, which completely inhibited the cycle when administered at a level of 15 mg/ kg. In mice infected with P. berghei, compound 8 (n = 4; R =H) reduced parasitemia by up to 37% (25 mg/kg) on day 7 following inoculation.
References
- Li C, Zhu X, Ji X, Quanquin N, Deng YQ, et al. (2017) Chloroquine, a FDA-approved Drug, Prevents Zika Virus Infection and its Associated Congenital Microcephaly in Mice. E Bio Medicine 24: 189-194.
- Shiryaev SA, Mesci P, Pinto A, Fernandes I, Sheets N, et al. (2017) Repurposing of the anti-malaria drug chloroquine for Zika Virus treatment and prophylaxis. Sci Rep 7: 15771.
- Gao J, Tian Z, Yang X (2020) Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Biosci Trends.
- Kim KA, Park JY, Lee JS, Lim S (2003) Cytochrome P450 2C8 and CYP3A4/5 are involved in chloroquine metabolism in human liver microsomes. Arch Pharm Res 26: 6317.
- Kaewkhao K, Chotivanich K, Winterberg M, Day NP, Tarning J, et al. (2019) High sensitivity methods to quantify chloroquine and its metabolite in human blood samples using LC-MS/MS. Bioanalysis 11: 333-347.
- Projean D, Baune B, Farinotti R, Flinois JP, Beaune P, et al. (2003) In vitro metabolism of chloroquine: identification of CYP2C8, CYP3A4, and CYP2D6 as the main isoforms catalyzing Ndesethylchloroquine formation. Drug Metab Dispos 31: 748-754.
- Ofori-Adjei D, Ericsson O, Lindstrom B, Sjoqvist F (1986) Protein binding of chloroquine enantiomers and desethylchloroquine. Br J Clin Pharmacol 22: 356-358.
- Walker O, Birkett DJ, Alvan G, Gustafsson LL, Sjoqvist F (1983) Characterization of chloroquine plasma protein binding in man. Br J Clin Pharmacol 15: 375-377.
- Ducharme J, Farinotti R (1996) Clinical pharmacokinetics and metabolism of chloroquine. Focus on recent advancements. Clin Pharmacokinet 31: 257-274.
- Coronado LM, Nadovich CT, Spadafora C (2014) Malarial hemozoin: from target to tool. Biochim Biophys Acta 1840: 2032-2041.
- Colson P, Rolain JM, Raoult D (2020) Chloroquine for the 2019 novel coronavirus SARS-CoV-2. Int J Antimicrob Agents.
- Wang M, Cao R, Zhang L, Yang X, Liu J, et al. (2020) Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res 30: 269-271.
- Vincent MJ, Bergeron E, Benjannet S, Erickson BR, Rollin PE, et al (2005) Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol J 2: 69.
- Chou AC, Fitch CD (1992) Heme polymerase: modulation by chloroquine treatment of a rodent malaria. Life Sci 51: 2073- 2078.
- Slater AF, Cerami A (1992) Inhibition by chloroquine of a novel haem polymerase enzyme activity in malaria trophozoites. Nature 355: 167-169.
- Vandekerckhove S, D'hooghe M (2015) Quinoline-based antimalarial hybrid compounds. Bioorg Med Chem 23: 5098-5119.
- Plantone D, Koudriavtseva T (2018) Current and Future Use of Chloroquine and Hydroxychloroquine in Infectious, Immune, Neoplastic, and Neurological Diseases: A Mini-Review. Clin Drug Investig 38: 653-671.
- FDA Approved Drug Products: Chloroquine Phosphate Oral Tablets.
- FDA Approved Drug Products: Aralen Chloroquine Oral Tablets.
- FDA: Emergency use Authorization for Hydroxychloroquine and Chloroquine Revoked.
- Mihaly GW, Ward SA, Edwards G, Nicholl DD, Orme ML, et al. (1985) Pharmacokinetics of primaquine in man. I. Studies of the absolute bioavailability and effects of dose size. Br J Clin Pharmacol 19: 745- 750.
- Alving AS, Arnold J, Hockwald RS, Clayman CB, Dern RJ, et al. (1955) Potentiation of the curative action of primaquine in vivax malaria by quinine and chloroquine. J Lab Clin Med 46: 301-306.
- Hill DR, Baird JK, Parise ME, Lewis LS, Ryan ET, et al. (2006) Primaquine: report from CDC expert meeting on malaria chemoprophylaxis I. Am J Trop Med Hyg 75: 402- 415.
- Cohen RJ, Sachs JR, Wicker DJ, Conrad ME (1968) Methemoglobinemia provoked by malarial chemoprophylaxis in Vietnam. N Engl J Med 279: 1127- 1131.
- Coleman MD, Coleman NA (1996) Drug-induced methaemoglobinaemia. Treatment issues. Drug Saf 14: 394-405.
- Taavitsainen P, Juvonen R, Pelkonen O (2001) In vitro inhibition of cytochrome P450 enzymes in human liver microsomes by a potent CYP2A6 inhibitor, trans-2-phenylcyclopropylamine (tranylcypromine), and its nonamine analog, cyclopropylbenzene. Drug Metab Dispos 29: 217- 222.
- Bapiro TE, Andersson TB, Otter C, Hasler JA, Masimirembwa CM (2002) Cytochrome P450 1A1/2 induction by antiparasitic drugs: dose-dependent increase in ethoxyresorufin O-deethylase activity and mRNA caused by quinine, primaquine and albendazole in HepG2 cells. Eur J Clin Pharmacol 58: 537-542.
- Suhrbier A (1987) The complete development in vitro of the vertebrate phase of the mammalian malarial parasite Plasmodium berghei. Trans R Soc Trop Med Hyg 81: 907-909.
- Al-Olayan EM (2002) Complete development of mosquito phases of the malaria parasite in vitro. Science 295: 677-679.
- Vanderberg JP, Gwadz RW (1980) The transmission by mosquitoes of plasmodia in the laboratory. In: Kreier JP (ed) Malaria, vol 2, Pathology, vector studies, and culture. Academic, New York 154- 234.
- Sinden RE (1996) Infection of mosquitoes with rodent malaria. Mol Biol Insect Dis Vector 67- 91.
- Sinden RE (2002) Maintenance of the Plasmodium berghei life cycle. In: Doolan D (ed) Methods in molecular medicine. Humana, Totowa, NJ 25-40.
- Shute P, Maryon M (1966) Laboratory technique for the study of malaria. 2nd edn. J & A Churchill, London.
- Franke-Fayard B (2004) A Plasmodium berghei reference line that constitutively expresses GFP at a high level throughout the complete life cycle. Mol Biochem Parasitol 137: 23-33.
- Dearsly AL (1990) Sexual development in malarial parasites: gametocyte production, fertility and infectivity to the mosquito vector. Parasitology 100: 359-368.
- Jaffe RI (1990) Differences in susceptibility among mouse strains to infection with Plasmodium berghei (ANKA clone) sporozoites and its relationship to protection by gamma irradiated sporozoites. Am J Trop Med Hyg 42: 309- 313.
- Scheller LF (1994) Susceptibility of different strains of mice to hepatic infection with Plasmodium berghei. Infect Immune 62: 4844-4847.
- Mons B (1986) Intraerythrocytic differentiation of Plasmodium berghei. Acta Leiden 54:1–83 Schneider I (1972) Cell lines derived from late embryonic stages of Drosophila melanogaster. J Embryol Exp Morphol 27: 353-365.
- Vanderberg JP (1968) Protective immunity produced by the injection of x-irradiated sporozoites of Plasmodium berghei. II. Effects of radiation on sporozoites. J Parasitol 54: 175-180.
- Sinden RE (2008) Progression of Plasmodium berghei through Anopheles stephensi is densitydependent. PLoS Pathog 3: 195.
- Ploemen IH (2009) Visualisation and quantitative analysis of the rodent malaria liver stage by real time imaging. PLoS One 4: 7881.
- Feldmann AM, Ponnudurai T (1989) Selection of Anopheles stephensi for refractoriness and susceptibility to Plasmodium falciparum. Med Vet Entomol 3: 41-52.
- Sato Y (1996) Effect of temperature on Plasmodium berghei and P. yoelii on mosquito stage in Anopheles stephensi. J Parasitol 45: 98-104.
- Yoeli M, Upmanis RS (1968) Plasmodium berghei ookinete formation in vitro. Exp Parasitol. 22: 122-128.
- Strome CP (1979) The cultivation of the exoerythrocytic stages of Plasmodium berghei from sporozoites. In Vitro 15: 531-536.
- Sinden RE, Smith JE (1980) Culture of the liver stages (exoerythrocytic schizonts) of rodent malaria parasites from sporozoites in vitro. Trans R Soc Trop Med Hyg 74: 134-136.
- Calvo-Calle JM (1994) In vitro development of infectious liver stages of P. yoelii and P. berghei malaria in human cell lines. Exp Parasitol 79: 362-373.
- Sinden RE (1990) The development and routine application of high-density exoerythrocytic-stage cultures of Plasmodium berghei. Bull World Health Organ 68: 115-125.
- Beaudoin RL, Mitchell SC, Tubergen FTA (1977a) Plasmodium berghei: immunization of mice against the ANKA strain using the unaltered sporozoite as anantigen. Experimental Parasitology 42: 1-5.
- Bhattacharjee AK, Kyle DE, Vennerstrom JL, Milhous WK (2002) A 3D QSAR pharmacophore model and quantum chemical structure–activity analysis ofchloroquine(CQ)-resistance reversal. J Chem Inf Comput Sci 42: 1212-1220.
- Bowman ZS, Oatis Jr JE, Whelan JL, Jollow DJ, McMillan DC (2004) Primaquine-induced hemolytic anemia: susceptibility of normal versus glutathione-depleted rat erythrocytes to 5- hydroxyprimaquine. J Pharmacol Exp Thr 309: 79-85.
- Bray PG, Deed S, Fox E, Kalkanidis M., Mungthin M, et al. (2005) Primaquine synergises the activity of chloroquine against chloroquine-resistant P. falciparum. Biochem Pharmacol 70: 1158-1166.
- Brueckner R, Baird OC, Milhous JKWK (2001) Antimalarial Chemotherapy: Mechanisms of Action, Resistance, and New Directions in Drug Discovery. Humana Press, Totowa, NY.
- Chakravarty S, Cockburn IA, Kuk S, Overstreet MG, Sacci JB, et al. (2007) CD8+ T lymphocytes protective against malaria liver stages are primed in skin-draining lymph nodes. Nature Medicine 13: 1035-1041.
- Frisk-Holmberg M, Bergqvist Y, Termond E, Domeij Nyberg B (1984) The single dose kinetics of chloroquine and its major metabolite desethylchloroquine in healthy subjects. Euro J Clin Pharmacol 26: 521-530.
- Gupta L, Srivastava K, Singh S, Puri SK, Chauhan PM (2008) Synthesis of 2-[3-(7-Chloroquinolin-4-ylamino)-alkyl]-1-(substituted phenyl)-2,3,4,9-tetrahydro-1H-beta-carbolines as a new class of antimalarial agents. Bioorg Med Chem Lett 18: 3306-3309.
- Kumar A, Srivastava K, Raja Kumar S, Puri SK, Chauhan PM (2009) Synthesis of 9-anilinoacridine triazines as new class of hybrid antimalarial agents. Bioorg Med Chem Lett 19: 6996-6999.
- Friesen J, Matuschewski K (2011) Comparative efficacy of pre-erythrocytic whole organism vaccine strategies against the malaria parasite. Vaccine. 29: 7002-7008.
- Walsh JJ, Coughlan D, Heneghan N, GaynorC, Bell A (2007) A novel artemisinin–quinine hybrid with potent antimalarial activity. Bioorg Med Chem Lett 17: 3599-3602.
- Schramm H, Robertson LW, Oesch F (1985) Differential regulation of hepatic glutathione transferase and glutathione peroxidase activities in the rat. Biochem Pharmacol 34: 3735-3739.
- Ramjanee S, Robertson JS, Franke Fayard B, Sinha R, Waters AP, et al. (2007) The use of transgenic Plasmodium berghei expressing the Plasmodium vivax antigen P25 to determine the transmission-blocking activity of sera from malaria vaccine trials. Vaccine 25: 886-894.
- Solomon VR, Lee H (2009) Chloroquine and its analogs: a new promise of an old drug for effective and safe cancer therapies. Eur J Pharmacol 625: 220-233.
- Peters JU (2012) The binding of the circumsporozoite protein to cell surface heparan sulfate proteoglycans is required for plasmodium sporozoite attachment to target cells. J Biol Chem 276: 26784-26791.
- Kaur K, Jain M, Reddy RP, Jain R (2010) Quinolines and structurally related heterocycles as antimalarials. Eur J Med Chem 45: 3245-3264.
- Price RN, von Seidlein L, Valecha N, Nosten F, et al. (2014) Global extent of chloroquine-resistant Plasmodium vivax: a systematic review and meta-analysis. Lancet Infect Dis 14: 982-991.
- Dondorp AM, Smithuis FM, Woodrow C, Seidlein LV (2017) How to Contain Artemisinin- and Multidrug-Resistant Falciparum Malaria. Trends Parasitol 33: 353-363.
- Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM (2008) Artemisinin Resistance in Cambodia 1 (ARC1) Study Consortium. Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med 359: 2619-2620.
- Dondorp AM, Nosten F, Yi P, Das D, Phyo AP (2009) Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med 361: 455-467.
- Cheeseman IH, Miller BA, Nair S, Nkhoma S, Tan A, et al. (2012) A major genome region underlying artemisinin resistance in malaria. Science 336: 79-82.
- Teixeira C, Vale N, Pérez B, Gomes A, et al. (2014) "Recycling" classical drugs for malaria. Chem Rev 114: 11164-11220.
- https://www.mmv.org/research- development/mmv-supported projects
- Dunst J, Kamena F, Matuschewski K (2017) Cytokines and Chemokines in Cerebral Malaria Pathogenesis. Front Cell Infect Microbiol.7: 324.
- Morphy R, Rankovic Z (2005) Designed multiple ligands. An emerging drug discovery paradigm. J Med Chem 48: 6523-6543.
- Pinheiro CS, Luiz, Feitosa Lívia M, Gandi M, Silveira FF (2019) The Development of Novel Compounds Against Malaria: Quinolines, Triazolpyridines, Pyrazolopyridines and Pyrazolopyrimidines. Molecules. 22: 4095.
- Boechat N, Pinheiro LC, Silva TS, Aguiar AC, Carvalho AS, et al (2012) New trifluoromethyl triazolopyrimidines as anti-Plasmodium falciparum agents. Molecules 17: 8285-8302.
- Azeredo LFSP, Coutinho JP, Jabor VAP, Feliciano PR, Nonato MC, et al. (2017) Evaluation of 7-arylaminopyrazolo[1,5-a]pyrimidines as anti-Plasmodium falciparum, antimalarial, and Pf-dihydroorotate dehydrogenase inhibitors. Eur J Med Chem 126: 72-83.
- Carvalho LH, Brandão MG, Santos Filho D, Lopes JL, Krettli AU (1991) Antimalarial activity of crude extracts from Brazilian plants studied in vivo in Plasmodium berghei-infected mice and in vitro against Plasmodium falciparum in culture. Braz J Med Biol Res 24: 1113-23.
- Gwadz RW, Koontz LC, Miller LH, Davidson DE (1983) Jr. Plasmodium gallinaceum: avian screen for drugs with radical curative properties. Exp Parasitol 55: 188-196.
- Tasón de Camargo M, Krettli AU (1978) Aedes fluviatilis (Lutz), a new experimental host for Plasmodium gallinaceum brumpt. J Parasitol 64: 924-925.
- Carvalho LH, Ferrari WM, Krettli AU (1992) A method for screening drugs against the liver stages of malaria using Plasmodium gallinaceum and Aedes mosquitos. Braz J Med Biol Res 25: 247-255.
- Aguiar ACC, Figueiredo FJB, Neuenfeldt PD Malar J (2016) 16:110.
- World Health Organization (WHO), Global database on antimalaria drug efficacy and resistance, Geneva: https://www.who.int/malaria/areas/drug_resistance/drug_ efficacy_database/en/, 2018 (accessed 25 May 2020).
- Carmona-Fonseca J, Alvarez G, Maestre A (2009) Methemoglobinemia and adverse events in Plasmodium vivax malaria patients associated with high doses of primaquine treatment. Am J Trop Med Hyg 80: 188-193.
- Shaffer N, Grau GE, Hedberg K, Davachi F, Lyamba B , et al. (1991) Tumor necrosis factor and severe malaria. J Infect Dis 163: 96-101.
- Knight JC, Udalova I, Hill AV, Greenwood BM, Peshu N, et al. (1999) A polymorphism that affects OCT-1 binding to the TNF promoter region is associated with severe malaria. Nat Genet 22: 145-150.
- Oduola AM, Milhous WK, Weatherly NF, Bowdre JH, Desjardins RE (1988) Plasmodium falciparum: induction of resistance to mefloquine in cloned strains by continuous drug exposure in vitro. Exp Parasitol 67: 354-360.
- Trager W, Jensen JB (1976) Human malaria parasites in continuous culture. Science 193: 673-675.
- Lambros C, Vanderberg JP (1979) Synchronization of Plasmodium falciparum erythrocytic stages in culture. J Parasitol 65: 418-420.
- Vossen MG, Pferschy S, Chiba P, Noedl H (2010) The SYBR Green I malaria drug sensitivity assay: performance in low parasitemia samples. Am J Trop Med Hyg 82: 398-401
- Calvo Calle JM, Moreno A, Eling WM, Nardin EH (1994) In vitro development of infectious liver stages of P. yoelii and P. berghei malaria in human cell lines. Exp Parasitol 79: 362-373.
- Borenfreunda E, Babicha H, Martin-Alguacila N (1987). Toxicol in Vitro. 2: 1-6.
- Aguiar AC, Santos Rde M, Figueiredo FJ, Cortopassi WA, Pimentel AS, et al. (2012) Antimalarial activity and mechanisms of action of two novel 4-aminoquinolines against chloroquine-resistant parasites. PLoS One 7: e37259.
- do Céu de Madureira M, Paula Martins A, Gomes M, Paiva J, Proença da Cunha A, et al. (2002) Antimalarial activity of medicinal plants used in traditional medicine in S. Tomé and Príncipe islands. J Ethnopharmacol 81: 23-29.
- Andrade Neto VF, Brandão MG, Stehmann JR, Oliveira LA, Krettli AU (2003) Antimalarial activity of Cinchona-like plants used to treat fever and malaria in Brazil. J Ethnopharmacol 87: 253-256.
- Talisuna AO, Bloland P, D'Alessandro U (2004) History, dynamics, and public health importance of malaria parasite resistance. Clin Microbiol Rev 17: 235-254.
- Wongsrichanalai C, Sibley CH (2013) Fighting drug-resistant Plasmodium falciparum: the challenge of artemisinin resistance. Clin Microbiol Infect 19: 908-916.
- World Health Organization, WHO Global Malaria Programme. Guidelines for the treatment of malaria. Geneva: World Health Organization; 2015.
- White NJ (2013) Pharmacokinetic and pharmacodynamic considerations in antimalarial dose optimization. Antimicrob Agents Chemother 57: 5792-5807.
- Simpson JA, Zaloumis S, DeLivera AM (2014) Making the most of clinical data: reviewing the role of pharmacokinetic-pharmacodynamic models of anti-malarial drugs. Aaps J 16: 962-974.
- World Health Organization. Assessment and monitoring of antimalarial drug efficacy for the treatment of uncomplicated falciparum malaria. Geneva: World Health Organization; 2003.
- Shah VP, Midha KK, Dighe S (1991) Analytical methods validation: bioavailability, bioequivalence and pharmacokinetic studies. Conference report. Eur J Drug Metab Pharmacokinet. 16: 249-255.
- U.S. Department of Health and Human Services FaDA, Center for Drug Evaluation and Research (CDER) [Internet]. Guidance for Industry. Bioanalytical Method Validation; 2013.
- World Health Organization. Methods and techniques for assessing exposure to antimalarial drugs in clinical field studies. Geneva: World Health Organization; 2011.
- Thomas CG, Ward SA, Edwards G (1992) Selective determination, in plasma, of artemether and its major metabolite, dihydroartemisinin, by high-performance liquid chromatography with ultraviolet detection. J Chromatogr 583: 131-136.
- Batty KT, Davis TM, Thu LT (1996) Selective high-performance liquid chromatographic determination of artesunate and alpha and beta-dihydroartemisinin in patients with falciparum malaria. J Chromatogr B Biomed Appl 677: 345-350.
- Melendez V, Peggins JO, Brewer TG (1991) Determination of the antimalarial arteether and its deethylated metabolite dihydroartemisinin in plasma by high-performance liquid chromatography with reductive electrochemical detection. J Pharm Sci 80: 132-138.
- Batty KT, Salman S, Moore BR (2012) Artemisinin-naphthoquine combination therapy for uncomplicated pediatric malaria: a pharmacokinetic study. Antimicrob Agents Chemother. 56: 2472-2484.
- Birgersson S, Ericsson T, Blank A (2014) A high-throughput LC-MS/MS assay for quantification of artesunate and its metabolite dihydroartemisinin in human plasma and saliva. Bioanalysis 6: 2357-2369.
- Hilhorst MJ, Hendriks G, De Vries R (2014) A high-performance liquid chromatography-tandem mass spectrometry method for the determination of artemether and dihydroartemisinin in human plasma. J Chromatogr B Analyt Technol Biomed Life Sci 965: 45-53.
- Lindegardh N, Hanpithakpong W, Kamanikom B (2011) Quantification of dihydroartemisinin, artesunate and artemisinin in human blood: overcoming the technical challenge of protecting the peroxide bridge. Bioanalysis 3: 1613-1624.
- Debrus B, Lebrun P, Kindenge JM (2011) Innovative highperformance liquid chromatography method development for the screening of 19 antimalarial drugs based on a generic approach, using design of experiments, independent component analysis and design space. J Chromatogr A 1218: 5205-5215.
- Sheiner LB (1984) The populations approach to pharmacokinetic data analysis: rationale and standard data analysis methods. Drug Metab Rev 15: 153-171.
- Sheiner LB, Rosenberg B, Marathe VV (1977) Estimation of population characteristics of pharmacokinetic parameters from routine clinical data. J Pharmacokinet Biopharm 5: 445-479.
- Aarons L, Ogungbenro K (2010) Optimal design of pharmacokinetic studies. Basic Clin Pharmacol Toxicol 106: 250-255.
- Steimer JL, Mallet A, Golmard JL (1984) Alternative approaches to estimation of population pharmacokinetic parameters: comparison with the nonlinear mixed-effect model. Drug Metab Rev 15: 265-292.
- Beal SL (2001) Ways to fit a PK model with some data below the quantification limit. J Pharmacokinet Pharmacodyn 28: 481-504.
- Holford N (2013) A time to event tutorial for pharmacometricians. CPT Pharmacometrics Syst Pharmacol 2: 43.
- Savic RM, Jonker DM, Kerbusch T (2007) Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn 34: 711-726.
- Klayman DL (1985) Qinghaosu (artemisinin): an antimalarial drug from China. Science 228: 1049-1055.
- De Vries PJ, Dien TK (1996) Clinical pharmacology and therapeutic potential of artemisinin and its derivatives in the treatment of malaria. Drugs 52: 818-836.
- Davis TM, Karunajeewa HA, Ilett KF (2005) Artemisinin-based combination therapies for uncomplicated malaria. Med J Aust 182: 181-185.
- Dondorp A, Nosten F, Stepniewska K (2005) South East Asian Quinine Artesunate Malaria Trial g. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet. 366: 717-725.
- Dondorp AM, Fanello CI, Hendriksen IC (2010) Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet 376: 1647-1657.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Sonwani HP (2023) Antimalaria and Anti-Inflammatory Activites NewChloroquine and Primaquine Hybrids Targeting the Blockade of Malaria ParasiteTransmission. World J Pharmacol Toxicol 6: 208. DOI: 10.4172/wjpt.1000208
Copyright: © 2023 Sonwani HP. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1138
- [From(publication date): 0-2023 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 907
- PDF downloads: 231