Antidepressant Treatment Adherence among Homeless Population
Received: 26-Dec-2022 / Manuscript No. jart-23-88052 / Editor assigned: 28-Dec-2022 / PreQC No. jart-23-88052 (PR) / Reviewed: 11-Jan-2023 / QC No. jart-23-88052 / Revised: 18-Jan-2023 / Manuscript No. jart-23-88052 (R) / Published Date: 25-Jan-2023
Abstract
Inequality to mental health treatment among homeless populations in the U.S has become a major national concern, and non-adherence to antidepressant treatment is increasing. To address this problem, a systemic literature review was conducted to identify interventions that can improve antidepressant treatment adherence among this population in primary care settings. A literature search using CINAHL, PubMed, EMBASE, PsychINFO, and Google Scholar electronic databases yielded 6,041 studies that were reviewed according to several inclusion criteria: studies published in peer-reviewed journals between 2013 and 2017, sufficient racial ethnic representation from underserved groups, randomized control trial to improve adherence to prescribed antidepressants, participants with primary diagnosis of depression, follow up period of at least 6 months. Ten studies met inclusion criteria. Evidence revealed that improving antidepressant treatment adherence among underserved communities requires multifaceted interventions that employ the following: a) shared decision making, b) practice-based collaborative care and telemedicine collaborative care, and c) treatment retention and therapy participation. Interventions that can improve antidepressant treatment adherences in the homeless communities are multilayered. However, shareddecision making and collaborative care between patients and providers is critical in realizing positive outcomes. Because depression is chronic and recurring, continuous supportive services are needed. Some interventions have to be tailored to specific homeless patients depending on their response to therapy and treatment.
Keywords
Antidepressant adherence; Homeless; Mental health; Addiction research; Addiction therapy
Introduction
Depression is the most common mental health disease that causes instability in patients and its management and treatment require effective and prolonged care [1]. Antidepressant medications (AMs) are used as regimens of major depression disorders. Therefore, adherence to AMs is critical in ensuring improved quality of life, positive health outcomes, and cost-effectiveness. All patients with major depression disorder must seek treatment from mental health providers to achieve optimal outcome [2]. Because depression has a high public health impact, AMs are ranked as the most frequently prescribed medications in the US [3]. With an average rate of 55% adherence among patients with depression, non-adherence to AMs poses a huge challenge to the treatment of depression [1].
The first step in treating patients with major depression disorder is to ensure strict adherence to treatment plan and prescriptions. Several studies have shown that when antidepressants are prescribed, 28% of patients stop taking them after 1 month, and another 44% to 52% of patients stop taking medications after 3 months [4]. This is very common in depressed patients from the homeless communities [5-9]. Therefore, non-adherence to AMs is prevalent among the homeless communities [10-12], with several mitigating factors, including lack of insurance coverage, lack of medication storage space, lack of transportation, environment, poverty, and socioeconomic conditions. In addition, emergence of side effects, continuity of symptoms, complex prescriptions, and less satisfaction with the treatment can also increase non-adherence [13].
Homelessness is a social problem that has serious implications on the health of mentally ill individuals. Homeless patients exist in the US [5], and many parts of the world [14]. According to Paudyal et al. [15], 35, 000 people applied for accommodation with the Scottish government in 2015 because they were homeless. On the other hand, Fazel [6] reports that more than 400,000 and 600,000 individuals are homeless on any night in the European Union, and USA, respectively. On the night of January 2010, 649,917 individuals were homeless in the USA with approximately 62% staying in a shelter, and 26% of them had serious mental health illness, and 34% had chronic substance abuse problem [7]. It has been shown that majority of homeless individuals have mental illness or substance abuse problems [5]. Because this population faces serious health problems, serious efforts are needed to address their issues.
There are very few studies that have investigated the use of antidepressants and adherence in homeless populations. These studies have looked at how schizophrenia, human immunodeficiency virus (HIV), and tuberculosis (TB) treatments are associated to low adherence in the homeless [5,7]. The outcome indicated that majority of these patients go through depression and stress which leads to low adherence to their medications. Therefore it is known that homeless patients with HIV and TB poorly adhere to their medications. But little is known about homeless patients who are undergoing major depression. Optimal adherence to antidepressant medication treatment is key to continuity of care in homeless communities. It is important to note that severity of depression, occurrence of life stressors, and length of depression episode can impact the optimal response of antidepressant therapy. This is why, when antidepressant medications are taken as prescribed, severity of major depression disorder is reduced. But nonadherence to treatment plan can lead to severe consequences and hospitalization. Based on available evidence, improving antidepressant treatment adherence among homeless patients is challenging [10]. In order to identify necessary interventions, it is important to understand factors that contribute to non-adherence in homeless communities. The purpose of this literature review was to identify interventions that improve antidepressant treatment adherence among the homeless population with mental illness in primary care settings.
Methods
Search engines, key words, and initial article yield
A literature search for all published articles related to improving antidepressant treatment adherence in homeless communities was conducted using the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PubMed, EMBASE, PsychINFO, and Google Scholar electronic databases. Keywords and medical subject terms used to identify relevant studies were: “medication adherence”, “depression”, “underserved communities”, and “mental health”, “depressed minorities,” “patient compliance,” “depressive disorder,” “patient outcomes,” “antidepressants,” “interventions,” “improving antidepressant treatment”. Reference lists from all included studies and relevant reviews were searched. A web search was also performed to identify academic center on site research on underserved minority mental health patients with depression in regards to improving antidepressant treatment adherence. The initial search yielded a total of 6,041 studies: 932 articles from CINAHL, 1,462 articles from PubMed, 873 articles from EMBASE, 1,234 articles from PsychINFO, and 1,540 articles from Google Scholar. Next, articles were narrowed down using the criteria below.
Inclusion and exclusion criteria
Several inclusion criteria were used to identify studies to be included in this review: (i) English-language studies published in peer-reviewed journals between January 2013 and September 2017; (ii) sufficient racial ethnic representation from Latino Americans, African Americans, Arab Americans and other minority groups; (iii) studies with randomized control trial of at least one patient-focused intervention with the objective to improve adherence to prescribed antidepressants; (iv) the study had samples of participants with primary diagnosis of depression and who had prescriptions for antidepressants; (v) antidepressant adherence as one of the primary or secondary measures of the outcomes was considered; (vi) studies that reported any clinical outcome; and (vii) the study that had follow up period of at least 6 months. The following articles were excluded: (i) Literature review articles; (ii) articles not published in English; (iii) duplicate articles from other databases; (iv) articles more than 5 years old; and (v) articles that did not properly address methods and results related to improving antidepressant treatment adherence.
Final article yield and rationale for use
Results were examined by abstract, title, and reading the entire manuscript to determine if the study met the inclusion criteria. Out of the initial articles yielded, 5,971 were excluded because they were not within the 5 years and some were not published in English. After other exclusion criteria were applied, 10 articles remained to be used in the literature review. The ten articles represented the highest level of evidence available with 3 of them at level II, 2 at level III, and 5 at level IV evidence for improving antidepressant medication treatment adherence in the homeless communities.
Synthesis of Evidence
Homeless patients undergo several health disparities, which include lower access to healthcare, lower treatment quality, and high prevalence of mental illness [11]. This means that some of the needs of mentally ill patients are not adequately achieved even though; reducing mental health treatment inequality should be a priority in our healthcare system. Some studies have shown that the use of antidepressants among African Americans and Latinos have remained significantly low, while among non-Latino Whites it has increased [10]. Because of these findings, experts from different parts of the country have come together to discuss racial-ethnic disparities in relation to mental health [11]. One area featured in their discussion is medication adherence among underserved communities.
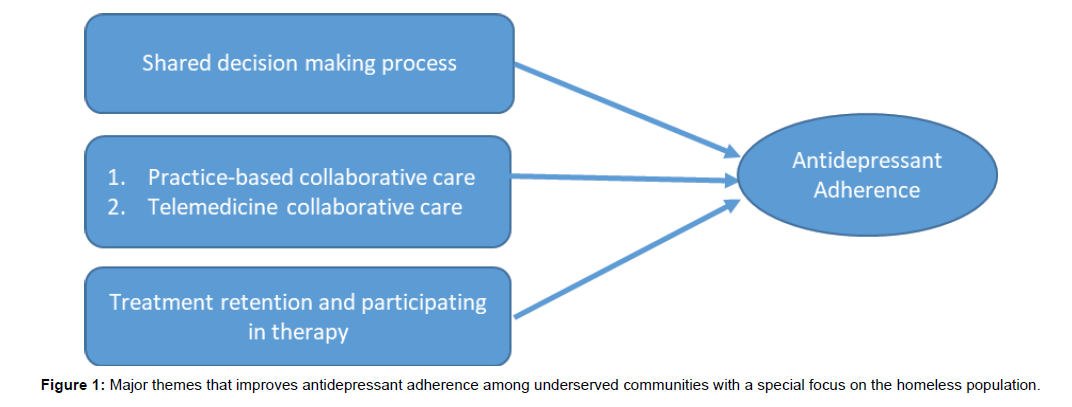
Medication adherence refers to the maintenance of adequate medical dosage and continuity of care. Therefore, managing patients with major depression disorder calls for strict adherence to antidepressant treatment. It is important to note that in homeless populations, low adherence to antidepressant medication has been widely reported [4,5,7,8]. Low adherence to antidepressants can lead to many problems such as, relapse, recurrence of disease, increase in cost of treatment, and interference with daily duties as well as hospitalization [15]. This is why low adherence to antidepressants among homeless communities is a critical issue that can contribute to unequal outcome in depression care. Managing depressed homeless patients is challenging because they are among the vulnerable and difficult to reach [8]. Health care providers who work with homeless individuals are encouraged to promote and establish a positive relationship with them. The kind of relationship should be based on mutual respect for the patients, upholding their dignity, building mutual trust, and being kind. This has been demonstrated in 208 federally funded healthcare programs, where treatment and care of homeless patients are tailored to meet their needs [6]. Some of these treatments interventions include outreach, integrated case management, collaboration with the community organizations, and guidance from the community advisory board [7]. Therefore, in order to achieve maximum outcome among these patients, it is important to think beyond access and affordability of antidepressant medications. Three major themes have emerged from the review of literature on antidepressant adherence among underserved communities with a special focus on the homeless population: 1) Shared decision making process, 2) Practice-based collaborative care and telemedicine collaborative care, and 3) Treatment retention and participating in therapy (Figure 1).
Shared decision making process
Adherence to antidepressant is a huge concern in a clinical setting [8]. Low adherence to antidepressant medications in underserved communities is associated to poor response to treatment [4]. This can sometimes be improved by patient-provider communication patterns, thus leading to shared decision-making between the provider and the patient. According to Bauer et al. [8], share-decision making between the patient and a provider plays a huge role in antidepressant medication adherence. De las Cuevas, also examined 160 psychiatric patients attending two community health centers in underserved communities, and their results indicated that adherence to antidepressant treatment was associated with attitudes towards shared decision making with their health care providers. This means that providers have to adapt their practice to meet the unique needs of homeless patients.
Practice-based collaborative care and telemedicine collaborative care
In many randomized effectiveness trials, practice-based collaborative care has been shown to improve antidepressant adherence in underserved communities. But this works well when primary care providers, mental health specialists, and nurse managers are located on-site within a primary care setting [5]. It is important to note that telemedicine-based collaborative care has been is effective in small satellite primary care clinics. In this setting, technology is used with an off-site team of mental health specialists collaborating with onsite primary care providers. This can be done in a central location by use of telephone, videoconference, and electronic health records, thus reaching far out to underserved communities where the numbers of providers are limited. In another randomized pragmatic comparative effectiveness trial, Fortney et al. [5] compared the outcomes of patients assigned to practice-based and telemedicine-based collaborative care in federally qualified health centers that served underserved populations in Arkansas’s Mississipi delta and Ozark highlands. Patients were screened for depression and 364 of them who were positive for depression were further enrolled for an 18month follow up. Patients were divided into two groups; one group was assigned to practicebased collaborative care (PBCC) and the other group was assigned to telemedicine-based collaborative care (TBCC). The PBCC group had an on-site primary care provider and a nurse manager who used evidencebased care. The TBCC group received evidenced based care from an on-site provider, and an off-site team comprised of a nurse manager as well as a pharmacist by phone. The TBCC group also received services from a psychologist and a psychiatrist via video conferencing. The primary clinical outcome measures were focused on changes in the severity of depression, remission, and treatment response. Results indicated that overtime; there was a significant reduction in severity for TBCC patients. Therefore, they concluded that an off-site telemedicinebased collaborative care team can give a better outcome as compared to locally available practice-based collaborative care in underserved communities.
Treatment retention and participation in therapy
In mental health, optimal treatment is determined by continuity of care in psychotherapy, and out-patient follow up, which is prescribed as treatment retention and therapy. In another study carried out by Bible et al. [2], it was determined that patient engagement in personal medicine plays a huge role in medication adherence. They did a crosssectional study, where they assessed medication adherence, engagement in self-care activities, perception of healthcare, and mental health control. Their results indicated that 98.3 of participants recognized selfcare as important to improving and maintaining mental health.
Knowledge gap
While researchers have found that seeking treatment when there is need, continuing care, and participating in therapy are important components of ensuring medication adherence among underserved communities, none of them has suggested methods to keep homeless patients engaged in the process. Homeless patients face a lot of challenges because they live in temporary shelters, therefore storing their medications, keeping up with scheduling, and transportation to therapy treatment can be very difficult. More research is needed to understand and improve antidepressant adherence in mentally ill homeless patients.
Discussion
Findings of this literature review revealed that improving antidepressant treatment adherence among underserved communities, and especially homeless populations, requires multifaceted interventions. Shared decision making, practice-based collaborative care and telemedicine collaborative care, as well as treatment retention and therapy participation are the main interventions. While these interventions can apply to the underserved, they fall short in addressing the problems faced by mentally ill homeless patients who sleep in rough conditions and live in derelict buildings, as well as temporary shelters. Major barriers contributing to medication non-adherence among the homeless are lack of prescription insurance coverage, instability in finance, lack of a place to store medication, and lack of reliable transport to pick up prescriptions.
Homelessness impedes one’s ability and well-being and is associated with high morbidity and mortality rate [5]. This is a unique population that needs more care and attention. Kardas, Lewek, & Matyjaszczyk [2] have established that homeless patients show poorer therapy outcomes due to their socio-economic status. In another study, Paudyal et al. [9] explored behavioral determinants of homeless patient’s adherence to prescribed medication using the theoretical domains framework (TDF). This UK study identified 13 out of 14 TDF domains that explained non-adherence to prescribed medications among the homeless. Interventions to improve antidepressant medication treatment adherences (AMTA) among the homeless should be based on three strategies: 1) overcoming transportation barriers, 2) team collaboration, and 3) telehealth.
Overcoming transportation barriers
Homeless individuals with mental health illness face several psychosocial and socioeconomic problems with decreased access to routine medical care. One of these problems is transportation to a medical facility. Continued update of patients’ contact information is important because transportation barrier can be addressed by arranging transportation, and having appointment reminders. Calling them ahead of time can ensure they come in as scheduled. Depression can affect memory, so some patients need to be reminded of their appointments. In some cases, it might be difficult to reach them the day before the appointment; therefore, calling at different times is advisable. Study carried out by Wells, Palinkas, Williams, & Ell [2] recommended that using a public van to transport patients can motivate them to come for treatment therapy when they know that someone is picking them up at a certain time and then taking them back home.
Team collaboration
Providers and healthcare teams must strive to build rapport with homeless patients by enhancing communication skills through shared-decision making and team collaboration [2]. Patient-provider communication patterns have been associated with adherence to both cardio metabolic and antidepressant medication adherence. Thus, flexibility and accommodation among providers and persons doing scheduling is critical when dealing with mental health patients who are homeless. This calls for collaboration that ensures that most of these patients are retained. Collaborative care is considered an evidencebased intervention for mental health [10,11]. It is aimed at improving access and continuity of mental health treatment in primary care setting. Two different research groups showed that incorporating principles of collaborative care in their intervention resulted in improved depression treatment adherence in homeless and low-income communities. They focused on using patient preferences to choose primary care treatment, and they had a depression care manager who monitored medication adherence and symptoms whenever there was a follow up visit. The depression manger had the responsibility of consulting both the psychiatrist and primary care physician. Grote et al. [3] also evaluated whether “MOMCare”, which is a culturally relevant collaborative care intervention was associated with improved quality of care and antidepressant treatment adherence among socioeconomically disadvantaged women. They conducted a randomized controlled multisite trial with blinded outcome. Their results indicated the majority of patients had post-traumatic stress disorder (PTSD) and patients on “MOMcare” were more likely to stay in their treatment visits and had greater chance to adhere to antidepressants. Therefore, the use of collaborative care is gaining support among research groups that study homeless patient populations [8, 16]. This study builds on previous findings to emphasize that collaborative care can improve antidepressant treatment adherence among the homeless patients.
Telehealth
Telehealth refers to the use of videoconferencing, telephone, mobile applications, Internet-based applications, store and forward imaging to provide long distance clinical services. Its advantage is that it decreases the cost of travel and transportation, while increases the ability of the providers to provide services to large geographic area. Telehealth technology may reduce the effect of treatment barriers and improve participation in antidepressant treatment adherence for homeless veterans with mental health. This technology has been used to study homeless veterans with posttraumatic stress disorder (PTSD). The Department of Veterans Affairs set up a goal in 2009, to end homelessness among veterans by 2015. They used a VA supportive housing program called Department of Housing and Urban Development-VA Supportive Housing (HUD-VASH) program to reduce the number of homeless veterans from the streets. Since the start of this program, there has been a 36% reduction in homelessness among veterans. However, veterans who live in HUD-VASH are still challenged with limited transportation and social support. Therefore, the use of health information technology (HIT) offers in-home health education, and disease promotion. Gabrielian et al. [4] investigated the use of HIT care management program and Care Coordination Home Telehealth (CCHT) to homeless veterans in HUD-VASH. Their results show that most veterans who lived in HUD-VASH were satisfied with CCHT. While more studies are still needed, it is becoming increasingly clear that in an integrated model involving primary care and mental health specialists telehealth maybe useful in improving antidepressant treatment adherence among the homeless veterans.
Implications
Because depression is chronic and recurring, continuous supportive services may be needed. Some interventions might also need to be tailored to specific homeless patients depending on their response to therapy and treatment. It is important to note that mental health patients have more unmet needs that can only be resolved if they receive proper psychiatric attention.
Conclusion
Adherence to antidepressant treatment remains a major challenge in the homeless community. While shared decision making and collaborative care between patients and providers is critical in realizing positive outcomes, the high rate of nonadherence to medication treatment in patients with depression warrant concern. As much as provision of transportation, enhancing collaboration, and integrating telehealth can help to improve adherence, there are still many barriers to be addressed with proactive care management and with addition of more resources. More scientific investigations are needed to identify modifiable factors to improve adherence among the homeless.
References
- Trimarchi M, Bondi S, Torre DE, Terreni MR, Bussi M (2017) Palate perforation differentiates cocaine-induced midline destructive lesions from granulomatosis with polyangiitis. Acta Otorhinolaryngol Ital 37(4): 281-285.
- Trimarchi M, Bussi M, Sinico RA, Meroni P, Specks U (2013) Cocaine-induced midline destructive lesions-An autoimmune disease?. Autoimmun Rev 12: 496-500.
- Di Cosola M, Ambrosino M, Limongelli L, Favia G, Santarelli A (2021) Cocaine-Induced Midline Destructive Lesions (CIMDL): A Real Challenge in Diagnosis. Int J Environ Res Public Health 18(15): 7831.
- Trimarchi M, Gregorini G, Facchetti F, Morassi ML, Manfredini C, et al. (2001) Cocaine-induced midline destructive lesions: clinical, radiographic, histopathologic, and serologic features and their differentiation from Wegener granulomatosis. Medicine 80: 391-404.
- Bains MK, Hosseini-Ardehali M (2005) Palatal perforations: past and present. Two case reports and a literature review. Br Dent J 199: 267-269.
- Colletti G, Allevi F, Valassina D, Bertossi D, Biglioli F (2013) Repair of cocaine-related oronasal fistula with forearm radial free flap. J Craniofac Surg 24:1734-1738.
- Berman M, Paran D, Elkayam O (2016) Cocaine-Induced Vasculitis. Rambam Maimonides Med J 7: 1-5.
- Moreno-Artero E, Querol-Cisneros E, Rodríguez-Garijo N, Tomás-Velázquez A, Antoñanzas J, et al. (2018) Mucocutaneous manifestations of cocaine abuse: A review. J Eur Acad Dermatol Venereol 32: 1420-1426.
- World Drug Report (2021) World Drug Report 2021. United Nations Office on Drugs and Crime, Austria.
- Richards JR, Jacqueline K (2022) Cocaine Toxicity. StatPearls Publishers, United States.
- Molteni M, Saibene AM, Luciano K, Maccari A (2016) Snorting the clivus away: an extreme case of cocaine-induced midline destructive lesion. BMJ Case Rep 2016: bcr2016216393.
- Trimarchi M, Bertazzoni G, Bussi M (2014) Cocaine induced midline destructive lesions. Rhinology 52(2):104-111.
- Barrientos J, Corchero G, Soler F (2021) Surgical treatment of cocaine-induced palatal perforations: Report of three cases and literature review. J Clin Exp Dent 13(2): e201-e206.
- Rampi A, Vinciguerra A, Bondi S, Policaro NS, Gastaldi G (2021) Cocaine-Induced Midline Destructive Lesions: A Real Challenge in Oral Rehabilitation. Int J Environ Res Public Health 18(6): 3219.
- Yaman H, Aydın Y, Yılmaz S, Onder E, Guclum E, et al. (2011) Recurrent and Massive Life Threatening Epistaxis due to Nasal Heroin Usage. Clin Exp Otorhinolaryngol 4(3):159-161.
- Wiesner O, Russel KA, Lee AS, Jenne DE, Trimarchi M, et al. (2004) Antineutrophil cytoplasmatic antibodies reacting with human neutrophil elastase as a diagnostic marker for cocaine-induced midline destructive lesions but not autoimmune vasculitis. Arthritis Rheum 50: 2954-2965.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Lemessa D (2023) Antidepressant Treatment Adherence among Homeless Population. J Addict Res Ther 14: 509.
Copyright: © 2023 Lemessa D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1205
- [From(publication date): 0-2023 - Jun 30, 2024]
- Breakdown by view type
- HTML page views: 1025
- PDF downloads: 180