Ankle Fractures: Did Quigley know Something We do not?
Received: 01-Jan-2024 / Manuscript No. crfa-24-125555 / Editor assigned: 04-Jan-2024 / PreQC No. crfa-24-125555(PQ) / Reviewed: 23-Jan-2024 / QC No. crfa-24-125555 / Revised: 24-Jan-2024 / Manuscript No. crfa-24-125555(R) / Accepted Date: 30-Jan-2024 / Published Date: 30-Jan-2024
Abstract
Background: Ankle fractures, particularly Weber B and C types, present challenges requiring surgical intervention due to their instability. Early and Swift reduction is pivotal, minimizing pain, swelling, and neurovascular issues and facilitating better soft tissue healing. Our orthopedic department employs various closed reduction techniques, and post-reduction, two methods are applied: casting with a plaster U-splint which allows the patient to be more mobile until surgery, and stockinette suspension, which potentially allows for early intervention. However, a comparative analysis of these techniques needs to be improved. Hence, we compare the two methods to assess their effects on soft tissue healing, surgery timing, pain control, and rehabilitation.
Methods: This observational, retrospective study, spanning 2019 to 2021, examines 54 patient files with Weber B or C ankle fractures. Inclusion criteria involve patients aged 18 to 65 with no significant prior ankle injuries or medical conditions affecting lower limb healing. The dependent variable is the time from fracture to surgery, while independent variables include pre-surgical treatment technique, background diseases, pre-fracture functional status, and inflammation indices. Statistical analyses include descriptive measures, Pearson correlation tests, and SPSS-28 software for significance. The Bnai-Zion Medical Center's Helsinki committee approved the study ethically.
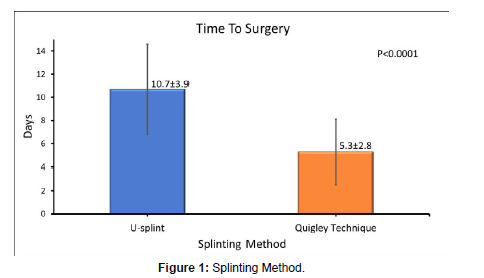
Results: 54 patients met the inclusion criteria and were divided into two groups according to the pre-surgical treatment method, i.e., casting with plaster U-splint vs. stockinette suspension (Quigley's technique). The time between the fracture and the definitive surgery was shorter in the stockinette suspension group compared to the casting group.
Conclusions: Our data suggests that Quigley's technique surpasses casting with U-splint plaster in reducing the time between an ankle fracture and definitive surgery. This finding emphasizes the potential advantages of adopting Quigley's technique in managing Weber B and C ankle fractures, promoting swifter interventions, and potentially enhancing overall patient outcomes.
Keywords
Ankle fractures; Weber B/C; Quigley’s technique
Introduction
Most orthopedic surgeons in Emergency Departments (ED) treat ankle fractures daily [1-9]. Lateral malleolus fracture, or Weber A (Lauge-Hansen SA), is the most common and is generally regarded as stable and treated conservatively by closed reduction and splinting. Bi/tri malleolar fractures with syndesmotic and ligamental damage or Weber B and C fractures (Lauge-Hansen SER or PER) are regarded as unstable, and the definitive treatment of most of these fractures will be surgical. An early closed reduction is critical because it reduces pain, swelling, and neurovascular compromise, allowing for better soft tissue healing [4-6]. Orthopedic surgeons implement a variety of techniques for closed reduction. One of which is the Quigley technique described in his article from 1959, where the patient's lower limb is suspended in a stockinette, leading to external rotation and abduction for the fracture together with avulsion of the ligaments, essentially reversing the mechanism of injury [5].
Following successful reduction, we apply two methods for maintaining it. Casting using a U-splint or a full-leg cast is the most prevalent. An alternative is keeping the lower limb in the stockinette suspension. This technique is advantageous since maintaining reduction while the patient's leg is constantly elevated allows faster edema absorption with fewer blisters and may lead to earlier surgical treatment. However, this is not a stable splinting technique, and patient hospitalization is required until definitive surgical treatment. Casting can rigidly hold the foot and ankle in position after a successful reduction, allowing for patient mobilization (either with crutches or wheelchairs) and discharge for outpatient follow-up until definitive surgical treatment. However, casting may be a double-edged sword since the patient's leg is not always elevated, leading to later surgical treatment due to slower soft tissue healing and a higher rate of edema and blisters [6-6]. Our main aim in this research is to examine which post-reduction pre-surgical treatment method leads to faster soft tissue healing and fewer blisters, effectively allowing for earlier definitive surgical treatment.
Materials and Methods
We performed a single-center observational, retrospective research based on medical files. The files collected include all patients aged 18 to 65 who suffered from Weber B or C fractures and were operated on at the orthopedic surgery department at Bnai-Zion Medical Center between 2019 and 2021. The collected data included fracture type, postreduction treatment method, and time to definitive surgical treatment.
The timing of definitive treatment was determined clinically by following soft tissue redenies. We also collected Patients' demographics, background diseases, functional status before the fracture, and inflammation indices around the day of definitive surgery. Since this is a retrospective study, there is no concern about dropouts. There is potential selection bias since only patients operated on are included in this research and only those who underwent the procedure at the Orthopedic Surgery Department at Bnai-Zion Medical Center and not in the community. Fifty-four patients were included in the study. The low number of patients may hinder the power of statistical analysis. The Helsinki committee of Bnai-Zion Medical Center approved this study.
Research variables
The dependent variable in this study is the time between the fracture and the definitive operation. The independent variables in this study are (1) pre-surgical reduction technique, (2) Background diseases, (3) Functional status before the fracture, and (4) Inflammation indices around the day of surgery.
Minimal sample size
We expect 15% differences between the Quigley technique and casting time to surgery. This is a two-sided hypothesis. α is expected to be 5% and power =80% (1-β). The minimal sample size in both groups all together is 50.
Statistical analysis
We performed descriptive statistical analyses of all main variables' percentages, averages, and standard deviations. The relationships between post-reduction pre-surgical treatment technique (plaster U-splint vs. stockinette suspension) and days to surgery were examined using Pearson correlation tests and considering inferential statistics. We also studied the effect of potential confounders, such as fracture type, age, gender, etc. P < 0.05 is regarded as statistically significant. All statistical analyses were done in SPSS-28 software (IBM, Armonk, NY, USA).
Results
Patient demographics
Our study includes 54 patients ages 18 to 65 years old who have suffered from Weber B or C fractures and were operated on at the orthopedic surgery department at Bnai-Zion Medical Center between 2019 and 2021. The patients were divided into two different groups according to the post-reduction technique that was used before definitive surgery: (1) the U-splint casting technique and (2) stockinette suspension (Quigley technique). The median age of the U-splint group was 40.1 years with a standard deviation (SD) of 14.0, while the median age for the Quigley technique group was 44.9 years with a standard deviation of 14.7 [Table 1]. Age did not differ between treatment groups, nor were there significant differences between groups on gender (p > 0.05). As for background diseases that could influence survival, we examined several common conditions that may affect the time between reduction and definitive surgery: Hypertension, Diabetes Mellitus without mention of complications, Osteoporosis, Hyperlipidemia, Hypothyroidism, Obesity, Alcohol use, and Tabaco use. 19 patients of the U-splint group had none of these conditions compared to only eight patients of the Quigley technique group. We found no statistical significance in the distribution of background diseases [Table 2].
| Number of patients | Median age | Male | Female | |
|---|---|---|---|---|
| U-splint | 35 | 40.1±14.0 | 19 (54.3%) | 16 (45.7%) |
| Quigley technique | 19 | 44.9±14.7 | 7 (36.8%) | 12 (63.2%) |
Table 1: Study population characteristics focusing on median age and gender.
| U-splint | Quigley Technique | |
|---|---|---|
| Hypertension % | 22.857 | 15.789 |
| Diabetes Mellitus % | 11.428 | 15.789 |
| Osteoporosis % | 2.857 | 10.526 |
| Hyperlipidemia % | 11.428 | 15.789 |
| Hypothyroidism % | 5.714 | 10.526 |
| Obesity % | 8.571 | 10.526 |
| Alcohol use % | 5.714 | 0 |
| Tabaco use % | 5.714 | 21.052 |
| None of the above % | 54.285 | 42.105 |
Table 2: Frequencies of background diseases.
The median CRP of the U-splint group was 9.4, with a standard deviation of 10.7, while the median CRP for the Quigley technique group was 16.0, with a standard deviation of 21.8 [Table 3]. CRP did not differ between treatment groups (p > 0.05). As for the Weber fracture type, 84.8% of the patients suffered from Weber B in the U-splint group, while only 15.2% suffered from Weber C fracture. In the Quigley technique group, 63.2% of the patients suffered from Weber B fracture, while only 36.8% suffered from Weber C fracture [Table 4]. There were no significant differences between groups on Weber category frequencies (p > 0.05).
| U-splint | Quigley Technique | |
|---|---|---|
| CRP | 9.4±10.7 | 16.0±21.8 |
Table 3: CRP Characteristics of the study population.
| U-splint | Quigley Technique | |
|---|---|---|
| Weber B % | 84.8 | 15.2 |
| Weber C % | 63.2 | 36.8 |
Table 4: Frequencies of weber fracture types.
However, the U-splint group had significantly more days to surgery than the Quigley technique group (t(52) = 5.3, p < 0.001). The median days to surgery for the U-splint group was 10.7 days with a SD of 3.9 days, while the median days to surgery for the Quigley technique group was 5.3 days with a SD of 2.8 days [Figure 1]. Furthermore, treatment differences remained significant also after statistically controlling for effects of age, CRP, and Weber category (F(1,46) = 23.0, p < 0.001).
Discussion
One of the most common fractures that orthopedic surgeons treat is ankle fractures [1-9]. This study compared two post reduction splinting techniques before definitive surgery for Weber B or C ankle fractures. To our knowledge, no previous study has compared these two post-reduction pre-surgical techniques to determine which is more beneficial for patients suffering from Weber B or C fractures regarding soft tissue healing, timing of surgery, pain control, and rehabilitation time following surgery.
In our study, we found that age, gender, Weber fracture type, and CRP levels did not have a significant difference between the two study groups regarding the time between the reduction of the fracture and the definitive surgery.
However, we found that the Quigley technique is significantly superior to the U-splint plaster technique regarding the time between the reduction and the definitive surgery. The U-splint plaster group had substantially more days to surgery than the Quigley group [t(52) = 5.3, p < 0.001)]. Furthermore, the treatment differences also remained significant after statistically controlling for the effects of age, CRP, and Weber fracture type [F(1,46) = 23.0, p < 0.001].
The strengths of this study include the neutralization of many diseases that are known to affect the healing of soft tissues. Thus, the reduction technique would be the only explanation for the difference in the time between the reduction and definitive surgery. Moreover, the variability of the Israeli population is reflected in the two study groups, thus increasing the likelihood that the outcome is suitable for various patients.
As for limitations, the main limitation of this study is the small sample size, which makes it difficult to determine if the outcome is a factual finding and may cause a type II error. Another possible limitation of the study is a selection bias in the Quigley group. The Quigley technique requires hospitalization, and the patients are examined daily during rounds, allowing for early identification of surgery-ready patients. However, it is very likely that the patients in the U-splint plaster group, who are followed on an outpatient basis, only elevate their braced leg for some hours of the day. Hence, soft tissue healing is delayed, and the surgery is delayed as well.
Conclusion
In conclusion, our study demonstrates that the Quigley reduction technique is superior to the plaster U-splint regarding the time between fracture and timing of the definitive surgery and is shown by a statistically significant difference (p < 0.001) in time between the reduction of ankle fractures marked as Weber B or C and the timing of the definitive surgery between the two groups. A more considerable sample size study should be performed to determine if this outcome is still valid on larger scales.
References
- Goost H, Wimmer MD, Barg A, Kabir K, Valderrabano V, et al. (2014) Fractures of the ankle joint—investigation and treatment options. Dtsch Arztebl Int. 111: 377-388.
- Juto H, Nilsson H, Morberg P (2018) Epidemiology of Adult Ankle Fractures: 1756 cases identified in Norrbotten County during 2009–2013 and classified according to AO/OTA. BMC Musculoskelet Disord. 19: 441 .
- Court Brown CM, McBirnie J, Wilson G (1998) Adult ankle fractures-an increasing problem? Acta orthopaedica Scandinavica. 69: 43-47 .
- Alton TB, Harnden E, Hagen J, Firoozabadi R (2015) Single provider reduction and splinting of displaced ankle fractures: a modification of Quigley's classic technique. J Orthop Trauma. 29: e166-e171 .
- Quigley TB (1959) A simple aid to the reduction of abduction-external rotation fractures of the ankle. Am J Surg. 97: 488- 493 .
- Dean DB (2009) Field management of displaced ankle fractures: techniques for successful reduction. Wilderness Environment Med. 20: 57-60 .
- Payne R, Kinmont JC, Moalypour SM (2004) Initial management of closed fracture-dislocations of the ankle. Annals of the Royal College of Surgeons of England. 86: 177 .
- D'Angelantonio A 3rd, Malay DS, Contento R, Winner R (2009) Instructional technique guide: closed reduction of the supination-eversion Stage IV (Weber Type B) ankle fracture. J Foot Ankle Surg. 48: 394-397.
- Brown C, Ross S, Mynark R, Guskiewicz K (2004) Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 13: 122-134 .
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Levine AD, Gidron Y, Semenisty A, Ben-Lulu O, Strul I (2024) AnkleFractures: Did Quigley know Something We do not?. Clin Res Foot Ankle, 12: 496.
Copyright: © 2024 Levine AD, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1078
- [From(publication date): 0-2024 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 885
- PDF downloads: 193