Ankle and Toe-Brachial Pressure Index after Exercise in Patients on Maintenance Hemodialysis
Received: 05-Dec-2015 / Accepted Date: 23-Jan-2017 / Published Date: 29-Jan-2017
Abstract
In patients undergoing hemodialysis (HD), the incidence of peripheral arterial disease (PAD) is high, leading to a severe condition; therefore, examinations that facilitate early diagnosis are necessary. The diagnostic accuracy of the ankle brachial pressure index (ABI) after walking, of which the cut-off value was corrected for HD patients, is higher than that of the ABI or toe brachial pressure index (TBI) at rest. Furthermore, the TBI after walking transiently induces marked perfusion disorder of the toes. The two procedures are useful for the early diagnosis of latent PAD in HD patients.
Keywords: Peripheral arterial disease; Ankle-brachial pressure index; Toe-brachial pressure index, Exercise
5006Abbreviations
ABI: Ankle-Brachial Pressure Index; TBI: Toe- Brachial Pressure Index; HD: Hemodialysis; Ex: Exercise; r-ZETS: Resting Zero TBI Sign; e-ZETS: Exercise-Induced Zero TBI Sign; PAD: Peripheral Arterial Disease
Introduction
The incidence of symptomatic peripheral arterial disease (PAD) in patients undergoing hemodialysis (HD) ranges from 19 to 23% [1,2], being higher than in the general population[3]. In some HD patients, PAD is asymptomatic, and rapidly progresses; critical limb ischemia (CLI) is detected without intermittent claudication. Refractory CLI requires lower-limb amputation, markedly reducing activities of daily life or leading to death from sepsis. Therefore, it is important to detect latent PAD in the early stage and perform treatment.
For PAD screening, the ABI is routinely used. However, in HD patients, the sensitivity of this index is low due to marked arterial calcification, delaying the detection of PAD. As a means to overcome this limitation, there is a method to measure lower limb blood flow after exercise [4-7]. In this article, we review the usefulness of these examinations.
One-minute test
Measurement of the ABI after walking (Ex-ABI) provides much information to evaluate perfusion disorder of the lower limbs. Ex-ABI is measured as follows: ABI was measured after 15 minutes at rest, and immediately after walking using the computerized treadmill system following a protocol. Each patient's 12-lead electrocardiogram and heart rate were monitored throughout the walking protocol for one minute (2.4 km/h, 12%). However, the walking speed was reduced to 2.0 km/h when the patient was more than 70 years old or was a low left ventricular function case. Trans-Atlantic Inter-Society? (TASC?) shows walk speed with 3.2 km/h, but uses speed of 2.4 km/h in a Japanese.
Walking was discontinued when one of the followings appeared: horizontal or downsloping ST depression of 0.1 mV compared with the resting ST at 80 msec after the J point [1], abnormal blood pressure responses (systolic pressure ≥ 250 mmHg, diastolic pressure ≥ 120 mmHg) [2], dangerous or potentially dangerous arrhythmias [3], the maximum heart rate obtained using the equation “220 – age” [4], difficulty in walking due to lower limb pain [5] and symptoms of the cardiopulmonary or neurological system [6].
For Ex-ABI measurement to make a definitive diagnosis of PAD, patients are instructed to walk on a treadmill for 5 minutes (3.2 km/h, 12%) [8]. However, the walking speed and slope are stressful for HD patients with a reduced exercise tolerance. We shortened the walking time (5 minutes) to 1 minute [5,6]. Such shortening of the walking time may reduce the accuracy of examination, but the diagnostic accuracy of the Ex-ABI at 1 minute was similar to that at 5 minutes in our study [9]. In addition, 1 minute walking has a merit: heart diseasederived accidents may not occur during examination [10]. For HD patients, 1 minute Ex-ABI measurement is appropriate.
Some investigators recommended the Doppler method for ABI measurement. However, there is a strong correlation between the oscillometric and Doppler methods [11,12] and an automatic measurement device [13] using the oscillometric method is more convenient for Ex-ABI measurement or large-scale screening.
Measurement of the TBI after walking (Ex-TBI) is the same as Ex- ABI. However, small cuff for toes is used.
Ex-ABI
Ex-ABI measurement is useful in patients with symptoms suggestive of PAD and an ABI of ≥ 0.91. As there is a superior arterialcalcification- related shift of the ABI value in HD patients, the Ex-ABI is highly useful. However, few studies have performed Ex-ABI measurement involving HD patients.
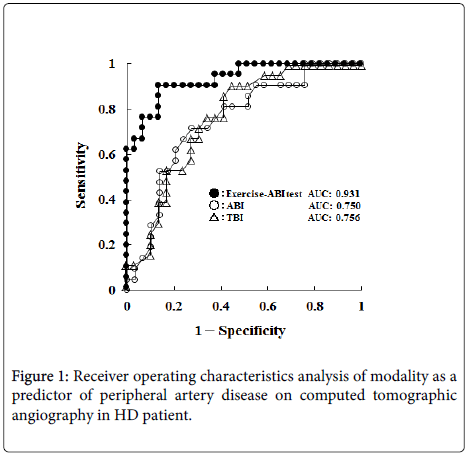
We investigated the Ex-ABI in HD patients, and compared it with computed tomographic angiography findings (above the knee) [6]. The diagnostic accuracy of the Ex-ABI was higher than that of the ABI or toe brachial pressure index (TBI), which may be available for HD patients because there is no influence of arterial calcification (Figure 1).
However, in ABI and Ex-ABI, evaluation of blood flow disorder below the knee is difficult (Table 1).
| Advantage | Disadvantage | |
|---|---|---|
| ABI | Simple | Low sensitivity |
| TBI | Simple | moderate sensitivity |
| Ex-ABI | Early detection | time-consuming |
| Ex-TBI | Early detection | time-consuming |
Table 1: Advantage and disadvantage in Ankle and toe-brachial pressure index.
According to the TASC, the cut-off value of the Ex-ABI was 15 to 20% lower than the ABI. However, when establishing the cut-off value at this range in HD patients, the sensitivity of the Ex-ABI was 100%, but its specificity was markedly low (48.3%) [6]. This suggests that the cut-off value previously used is not appropriate for HD patients. On the other hand, when re-establishing the cut-off value of the Ex-ABI as a 35.0% decrease, which was obtained on the receiver operating characteristics analysis, the sensitivity and specificity were 90.5 and 86.2%, respectively [6]. When the conventional cut-off value is used as the Ex-ABI in HD patients, there may be a false-positive increase. Therefore, in HD patients, the cut-off value of the Ex-ABI must be changed to a 35% decrease, considering the condition.
Ex-TBI
In HD patients, the big toe is often amputated due to CLI. To diagnose perfusion disorder at the toe level, the TBI using the oscillometric method is used. Matsui et al. [14] regarded a toe pressure reaching a flat as a “zero TBI sign”, and reported its usefulness as an index reflecting severe perfusion disorder of the toes. This sign refers to a state in which the toe pressure is below the measurement threshold of an automatic measurement device, 40 mmHg. If findings, such as ischemic pain at rest, ulcers, and gangrene, are present in addition to such hemodynamics, CLI may occur. Therefore, the “zero TBI sign” is important for CLI diagnosis.
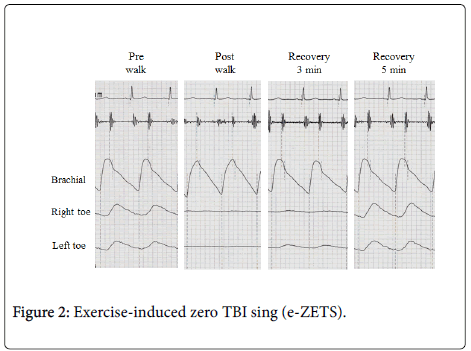
Recently, we found that the “zero TBI sign” was observed after 1 minute walking, and termed this phenomenon the “exercise-induced zero TBI sign (e-ZETS)” [7]. Patients meeting the following conditions were regarded as showing an e-ZETS: measurement with an automatic measurement device using the oscillometric method [1], resting TBI measurement is possible [2], the toe pressure reaches a flat on measurement immediately after walking [3] and the toe pressure transiently reaches a flat after the completion of walking [4], but serially appears again (Figure 2).
In 31.1% of outpatients undergoing HD, the e-ZETS was observed [7]. Furthermore, the “zero TBI sign”, which reflects severe perfusion disorder, was present in approximately 9.6% [7]. This suggests that, in a 3-fold number of HD patients with severe perfusion disorder of the toes in HD, e-ZETS is latently present.
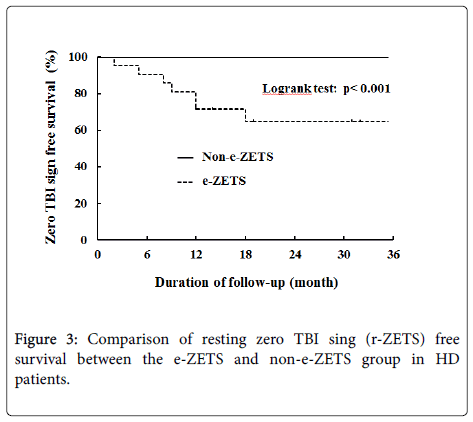
In our study [7], the TBI at rest in HD patients with the e-ZETS was slightly lower than the normal value [15,16] and there were no findings, such as cyanosis, ischemic pain at rest, ulcers, or gangrene. However, the results of a 36-month follow-up showed that the e-ZETS progressed to the zero TBI sign, involving CLI, in 36.4% of the patients (Figure 3). This suggests that the e-ZETS in HD patients reflects mild perfusion disorder, whereas the condition may become severe in the future.
In clinical practice, it is necessary to predict the risk of severe perfusion disorder by measuring the TBI regularly. However, no area of the TBI suggestive of “progression to severe perfusion disorder” has been reported. From this viewpoint, the e-ZETS progressed to the zero TBI sign at a high rate; it may indicate “progression to severe perfusion disorder”. Therefore, e-ZETS assessment by Ex-TBI measurement is useful for the early detection of severe perfusion disorder of the toes and prognostic assessment.
Conclusion
In HD patients, the incidence of PAD is high. PAD is asymptomatic, and rapidly progresses, leading to a severe condition in many patients. Therefore, it is important to detect latent PAD in the early stage before the appearance of clinical symptoms and perform treatment. The ABI and TBI measured immediately after walking indicate the presence of latent PAD; they are useful for the early detection of PAD.
References
- Webb AT, Franks PJ, Reaveley DA, Greenhalgh RM, Brown EA, et al. (1993) Prevalence of intermittent claudication and risk factors for its development in patients on renal replacement therapy. Eur J Vasc Surg 7: 523-527.
- Cheung AK, Sarnak MJ, Yan G, Dwyer JT, Heyka RJ, et al. (2000) Â Atherosclerotic cardiovascular disease risks in chronic hemodialysis patients. Kidny Int 58: 353-362.
- O’Hare A, Johansen K (2001) Lower-extremity peripheral arterial disease among patients with end-stage renal disease. J Am Soc Nephrol 12: 2838-2847.
- Okamoto K, Oka M, Maesato K, Ikee R, Mano T, et al. (2006) Peripheral arterial occlusive disease is more prevalent in patients with hemodialysis: Comparison with the findings of multidetector-row computed tomography. Am J Kidney Dis 48: 269-276.
- Tsuyuki K, Kohno K, Ebine K, Ohara T, Aoki T, et al. (2013) Exercise-ankle brachial pressureindex with one-minute treadmill walking in patients on maintenance hemodialysis. Ann Vasc Dis 6: 52-56.
- Tsuyuki K, Kohno K, Ebine K, Ohzeki Y, Ishiwata Y, et al. (2015) Usefulness of exercise-ankle brachial pressure index test and its diagnostic criteria in patients on maintenance hemodialysis. J Jpn Coll Angiol 55: 21-25.
- Tsuyuki K, Kohno K, Ebine K, Tamura S, Ohzeki Y, et al. (2016) Utility of exercise-induced zero TBI sign in patients on maintenance hemodialysis. Ann Vasc Dis 9: 125-129.
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, et al. (2007) Inter-society consensus for the management of PAD. J Vasc Surg S45: S5-67.
- Tsuyuki K, Kohno K, Ebine K, Tamura S, Ohzeki Y, et al. (2012) Accuracy of one minute walking on treadmill exercise test using automatic measurements of ankle-brachial pressure index. J Jpn Coll Angiol 52: 175-179.
- Watanabe S, Tsuyuki K, Sakamoto T, Ohzeki Y, Ebine K, et al. (2011) Safty of exercise-ankle brachial pressure index in patients with cardiovascular disease: Comparison of standard method and one minute method. Rehab sports 30: 2-5.
- Cortez-Cooper MY, Supak JA, Tanaka H (2003) A new device for automatic measurements of arterial stiffness and ankle-brachial index. Am J Cardiol 91: 1519-1522.
- Koji Y, Tomiyama H, Ichihashi H, Nagae T, Tanaka N, et al. (2004) Comparison of ankle-brachial pressure index and pulse wave velocity as markers of the presence of coronary artery disease in subjects with a high risk of atherosclerotic cardiovascular disease. Am J Cardiol 94: 868-872.
- Masaki H, Morita I, Tabuchi A, Ishida A, Hamanaka S, et al. (2003) Evaluation of intermittent claudication by Form PWV/ABI . J Jpn Coll Angio 43: 303-306.
- Matsui K, Murakami Y, Shimada K, Yoshioka T, Suzuki C, et al. (2005) Non-invasive Evaluation for Therapeutic Angiogenesis. J Jpn Coll Angio 45: 44-47.
- Working group for clinical guidelines for the evaluation and the treatment of cardiovascular complications in hemodialysis patients. Clinical guidelines for the evaluation and the treatment of cardiovascular complications in hemodialysis patients: Chapter 8, Peripheral artery disease. J Jpn Soc Dial Ther (2011) 44: 412–418.
- Ohtake T, Oka M, Ikee R, Mochida Y, Ishioka K, et al. (2011) Impact of lower limbs’ arterial calcification on the prevalence and severity of PAD in patients on hemodialysis. J Vasc Surg 53: 676-683.
Citation: Tsuyuki K, Kohno K, Ebine K, Tamura S, Ohzeki Y, et al. (2017) Ankle and Toe-Brachial Pressure Index after Exercise in Patients on Maintenance Hemodialysis. Atheroscler open access 2: 105.
Copyright: © 2017 Tsuyuki K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 4530
- [From(publication date): 0-2017 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 3652
- PDF downloads: 878