An Unusual Case of Palatal Abscess in A Pediatric Patient: A Case Report
Received: 10-May-2022 / Manuscript No. jdpm-22-61687 / Editor assigned: 12-May-2022 / PreQC No. jdpm-22-61687 / Reviewed: 26-May-2022 / QC No. jdpm-22-61687 / Revised: 31-May-2022 / Manuscript No. jdpm-22-61687 / Accepted Date: 06-Jun-2022 / Published Date: 07-Jun-2022 DOI: 10.4172/jdpm.1000124
Abstract
Diagnoses of a palatal swelling can often present a challenge to the clinician. Swellings may arise from manifold reasons including neoplasms, periapical lesions and periodontal abscesses. Diagnoses can be aided with examination of clinical presentation such as growth pattern, surface texture, base and consistency of lesion. Appropriate radiological and laboratory testing also provide support to a definitive diagnosis. In pediatric patients, dental abscesses are common, however, palatal presentations are rare. Most frequently, the etiology involves the palatal roots of the posterior teeth or occasionally the lateral incisor. Thorough knowledge of differential diagnoses and presentation of such lesions along with physiologic and anatomic factors that influence the spread and localization of dental infections is important to facilitate timely intervention for improved prognosis. The current report highlights an unusual case of a 5 year old boy presenting with a palatal abscess crossing the midline.
Keywords: Oral Pathology, Pediatric dentistry, Abscess
Keywords
Oral Pathology, Pediatric dentistry, Abscess
Introduction
Palatal swellings often pose a diagnostic challenge to the clinician and can be congenital or acquired in origin. Swellings may arise due to a variety of reasons including periapical lesions, periodontal abscesses or neoplastic processes whereas congenital origins include unerupted teeth and torus palatinus [1]. For masses on the hard palate, the differential diagnosis is relatively limited and can be concised by assessing the growth pattern of the mass [2]. Diagnoses for acutely presenting masses on the hard palate frequently includes reactive lesions, commonly mucoceles and abscesses [2]. In the paediatric patient, dental abscesses are common, however, palatal presentations are rare [3]. Abscesses are often associated with developmental anomalies of the teeth, infections of the pulp due to destruction of tooth structure or they may occur spontaneously without any apparent etiological factor [4]. Early intervention can prevent serious complications such as septicaemia, cavernous sinus thrombosis, brain abscess, shock, and occasionally death [5]. This report presents an unusual case of a pediatric patient with a palatal abscess crossing the midline.
Case Report
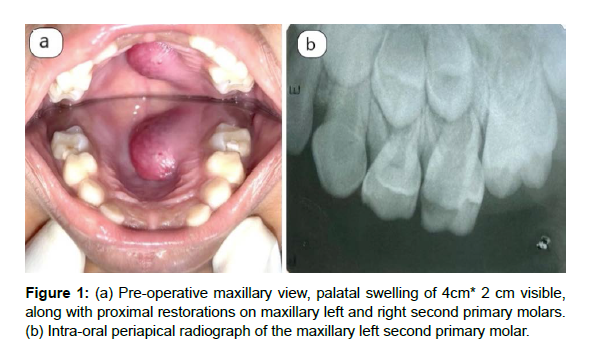
A 5 year old boy reported to the Department of Pedodontics and Preventive Dentistry with a chief complaint of a painless mass on the palatal region since the last 3 days. The patient had a history of pain on chewing in the upper left and right back tooth region for which he had visited a local dentist. He had decreased oral intake due to the mass and was also more fussy than usual with decreased activity. A detailed case history of the patient was obtained which provided no relevant medical history. Intraoral examination revealed a soft, erythematous, non- ulcerated, fluctuant swelling measuring 4cm x 2 cm present on the left half of the palate which crossed the midline. Further examination revealed proximal restorations on the upper left and right second primary molar which was associated with a periapical abscess. Proximal caries was also observed on the upper right primary first molar. The maxillary primary central incisors had exfoliated (Figure 1a).
Discussion
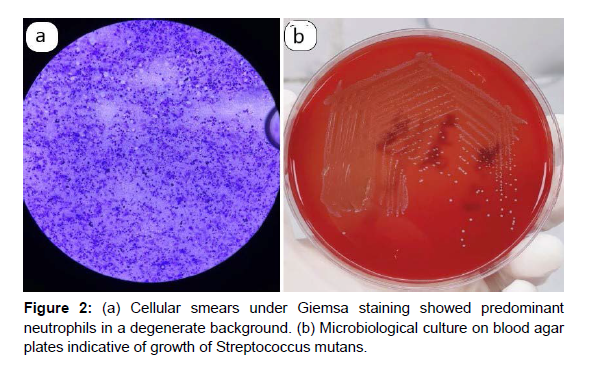
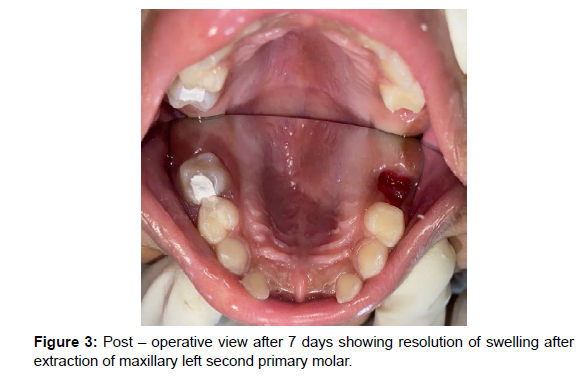
Odontogenic infections are the most common of all the infections of head and neck [6]. Dental infections spread beyond the tooth socket along the path of the least resistance into anatomic spaces removed from the site of initial infection. Advancement relies upon number, virulence of organism along with host resistance and anatomy of concerned area [7, 8]. The pathogenesis of dentoalveolar abscesses implicates a complex flora of obligate anaerobes and facultative anaerobes. Obligate outnumber facultative anaerobes with Streptococci, Fusobacterium species and the black-pigmented anaerobes such as Prevotella and Porphyromonas species being isolated most commonly [5]. Facultative anaerobes belonging to the viridans group streptococci and the anginosus group streptococci are commonly implicated in dental abscess. The viridans group Streptococci includes mitis group, oralis group, salivarius group, sanguinis group, and the mutans group [9]. A palatal abscess, as was observed in this case, is characterized by a diffuse, erythematous swelling with sudden onset. The palatal abscess is commonly observed lateral to the midline in the premolar-molar region and presents as a compressible mass or swelling which eases the diagnoses [10]. Etiology often includes periodontal abscesses from palatal pockets, palatal roots of posterior teeth and occasionally the lateral incisor as a source of infection [1]. However, infrequently, the palatal abscess can be localized in the midline and can pose a difficult diagnostic dilemma [10]. In such cases, a provisional diagnosis may also be arrived at by systematically eliminating scenarios on the basis of presentation such as growth, surface texture, base and consistency. Slow growing lesions include benign and malignant salivary gland tumors, pyogenic granuloma, torus palatinus and fibromas among others [2]. Lesions with smooth surface may be reactive hyperplastic in nature, salivary gland or mesenchymal lesions whereas presentation with rough surface may be indicative of squamous papilloma or verruca vulagris [11]. Definitive treatment for odontogenic abscesses involves draining the abscess, providing antibiotic support, pain control and removal or pulpectomy of the offending tooth. Oral antibiotics are usually sufficient and hospital admission is required in cases with features such as fever, dyspnea or airway compromise secondary to swelling [12]. Penicillins and cephalosporins are often used in odontogenic infections, but increasing antimicrobial resistance due to B-lactamase production makes the use of extended spectrum antibiotics or combinations with other antimicrobials such a metronidazole more suitable [13]. Clindamycin can be employed as an option for patients allergic to penicillin and/or cephalosporin antibiotics. This antibiotic is effective for infections (e.g., abscesses) with gram-positive aerobic bacteria and gram-positive or gram-negative anaerobic bacteria. However, Clindamycin may lead to serious adverse reaction such as Clostridioides difficile [14]. Anti-pseudomonal antibiotics like fourthgeneration or higher cephalosporins may be considered for patients with severe infection or immunocompromised state [12].
Conclusion
Acutely arising masses of the hard palate are uncommon in children, however, the clinician requires a thorough knowledge of the differentials in acute, subacute and chronic presentations. A palatal swelling may resemble a cyst, abscess or any benign or malignant tumor which may lead to delayed diagnoses and treatment. Early clinical and histopathological diagnosis along with appropriate treatment shortens the course of disease and improves the prognosis.
References
- Houston GD, Brown FH (1993) Differential Diagnosis of the Palatal Mass. Compendium 14: 1222-1224.
- Lasseter R, Sterner S (2013) Palatal Mass in A 2-Year-Old Boy. Pediatr Emerg Care 29: 78-79.
- Nidoni M, Shivashankara C, Nagarajappa D, Ahmed T (2014) A Report of A Rare Case of A Midline Palatal Abscess in A Paediatric Patient. Int J Dent Sci Res 2: 5-8.
- Seow WK (2003) Diagnosis and Management of Unusual Dental Abscesses in Children. Aust Dent J 48: 156-168.
- Shweta, Prakash SK (2013) Dental Abscess: A Microbiological Review. Dent Res J (Isfahan) 10: 585-591.
- Topazian RG, Goldberg MH, Hupp JR (2002) Oral and Maxillofacial Infections. Philadelphia : W.B. Saunders.
- Mitchell CS, Nelson MD Jr (1993) Orofacial Abscess of Odontogenic Origin in the Pediatric Patient: Report of Two Cases. Pediatr Radiol 23: 432-434.
- Jimenez Y, Bagan JV, Murillo J, Poveda R (2004) Odontogenic Infections. Complications. Systemic Manifestations. Med Oral Patol Oral Cr Bucal 9: 139-147.
- Fowell C, Igbokwe B, MacBean A (2012) The Clinical Relevance of Microbiology Specimens in Orofacial Abscesses of Dental Origin. Ann R Coll Surg Engl 94: 490-492.
- Sumer AP, Celenk P (2008) Palatal Abscess in A Pediatric Patient: Report of A Case. Eur J Dent 2: 291-293.
- Mortazavi H, Safi Y, Baharvand M, Rahmani S, Jafari S (2017) Peripheral Exophytic Oral Lesions: A Clinical Decision Tree. Int J Dent 2017: 9193831.
- Sanders JL, Houck RC (2021) Dental Abscess. StatPearls Publishing.
- Stephens MB, Wiedemer JP, Kushner GM (2018) Dental Problems in Primary Care. Am Fam Physician 98: 654-660.
- American Academy of Pediatric Dentistry (2021). Useful Medications for Oral Conditions. The Reference Manual of Pediatric Dentistry. American Academy of Pediatric Dentistry Chicago Ill
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Indexed at, Crossref, Google Scholar
Citation: Kalra N, Tyagi R, Khatri A, Goyal T, Kulood MK (2022) An Unusual Case of Palatal Abscess in A Pediatric Patient: A Case Report. J Dent Pathol Med 6: 124. DOI: 10.4172/jdpm.1000124
Copyright: © 2022 Kalra N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1898
- [From(publication date): 0-2022 - Nov 23, 2024]
- Breakdown by view type
- HTML page views: 1649
- PDF downloads: 249