Review Article Open Access
An Unusual Case of High Grade Triple Negative Intracystic Solid Papillary Carcinoma of Breast with Invasive Component
Junainah E1*, Baslaim M2, Huwait HF3, Shigairi S4, Nemenqani D1, Saber A5, Junainah M6, Alzahrani S7, Junainah J8 and Junainah F91Department of Pathology, University of Taif, Jeddah, Kingdom of Saudi Arabia
2Department of Surgery, MOH, King Fahad Hospital, Kingdom of Saudi Arabia
3Department of Pathology, Om Alqura University, Kingdom of Saudi Arabia
4Department of Radiology, MOH, King Fahad Hospital, Kingdom of Saudi Arabia
5Department of Medicine, MOH, Kingdom of Saudi Arabia
6Department of Surgery, MOH, Alnoor Hospital, Kingdom of Saudi Arabia
7Department of Medicine, University of Taief, Kingdom of Saudi Arabia
8Department of Medicine, King Abdulaziz Hospital, Kingdom of Saudi Arabia
9MOH, King Abdul Aziz Hospital, Kingdom of Saudi Arabia
- *Corresponding Author:
- Enaam Junainah
Department of Pathology, University of Taif
Jeddah, Kingdom of Saudi Arabia
Tel: 0096654442556
E-mail: mennastar3@yahoo.com
Received date: September 13, 2016; Accepted date: March 13, 2017; Published date: March 16, 2017
Citation: Junainah E, Baslaim M, Huwait HF, Shigairi S, Nemenqani D, et al. (2017) An Unusual Case of High Grade Triple Negative Intracystic Solid Papillary Carcinoma of Breast with Invasive Component. J Clin Exp Pathol 7:305. doi: 10.4172/2161-0681.1000305
Copyright: © 2017 Junainah E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
Background: Intracystic (encysted) papillary carcinoma (IPC) is a rare distinct entity of breast cancer, usually asymptomatic, sometimes presented as breast mass or nipple discharge. It shows benign appearance on imaging. Ultrasonography shows pure cyst or mixed image, sometime solid mass. Pathologically can be divided into pure form, or associated with ductal carcinoma in situ (DCIS) or invasive carcinoma. It is considered as noninvasive or minimally invasive, because there is no infiltrating growth pattern and metastases are rare. Traditionally considered to lack a myoepithelial layer, it has favorable prognosis even with invasion. Stromal invasion found in 92%. In case of high grade variant which diagnosed by high nuclear grade and high mitotic activity, usually triple negative and p53+ as we have in our case?
Case presentation: We report a case of breast cancer that occurred in 42-year-old woman presented with a painless lump in the left breast, FNA yielded hemorrhagic fluid. Patient underwent wide local Excision. The final histopathological finding shows encapsulated/intra cystic carcinoma, papillary variant with high grade features, as defined by nuclear pleomorphic and increased mitotic activity. This tumor is also hormone receptor and HER-2- negative, and is associated with stromal invasion by high grade NOS.
Conclusion: High grade encapsulated papillary carcinoma is extremely rare variant, usually associated with invasive component; morphologically it is more aggressive. It behaves like its invasive counterpart.
Keywords
Intra cystic; Invasive; Papillary carcinoma; Wide local excision
Abbreviations
IPC: Iinvasive papillary carcinoma; IHC: Immunohistochemistry; DCIS: Ductal carcinoma insitu; NOS: Not otherwise specified; EPCs: Encapsulated papillary carcinoma.
Background
Encapsulated papillary carcinoma (EPC) of the breast, it is considered as variant of ductal carcinoma in situ (DCIS) based on its indolent behavior. It accounts for approximately 0.5% to 2% of all breast cancers and typically occurs in postmenopausal women, but can occur in younger age group aging from 25-80 [1-3]. Histologically EPC is characterized by papillary configuration within a well-circumscribed cystic or distended duct with cytological features similar to papillary DCIS. These lesions lack myoepithelial cells at their periphery, in contact to DCIS which exhibits myoepithelial cell at the periphery; recently many authors have considered EPCs as, invasive carcinomas with an expansile growth [4-7].
The most extensively studied proteins that constitute the basal lamina component of the basement membrane are type IV collagen and laminin [8]. Those have been studied by Immunohistochemical targeting these proteins which demonstrated linear and continuous basement membranes in benign and in situ lesions and discontinuous or absent expression in invasive carcinoma [1-9].
High grade variant of this tumor is characterized histologically by high nuclear grade as well as high index of mitotic Figure and of larger size, furthermore has associated with invasive component, of usually NOS type but can be of papillary or any other subtypes [10-13]. Imunohistochemical study, shows lack of expression of ER, PR and Her-2 (triple negative group) has been detected in this remarkable case report. 12 cases have been reviewed by Dr Rakha in 2015. They reach to conclusion that it behaves in similar fashion to conventional form of invasive breast carcinomas [14].
Case Report
A 42-year-old woman presented with left side painful breast mass since one month, she has positive first degree relative with history of breast and endometrial carcinoma. On examination show left side large define cystic mass measures 6.5 cm, aspiration of the mass done and was reported as positive for malignant cells, the mass recurred after aspiration within 4 weeks, no palpable lymph node seen, wide local excision of the mass done with sentinel lymph node, the pathology report show cystic papillary carcinoma, high grade with invasive area of NOS grade III sentinel lymph node was negative.
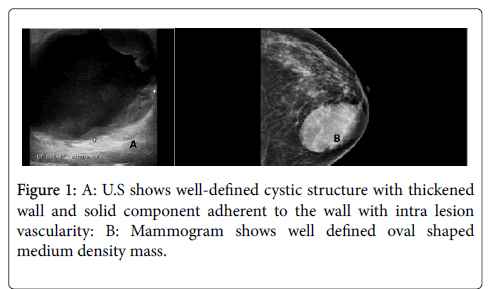
Ultrasonography finding
Large well-defined cystic structure with thickened wall and solid component adherent to the wall with intra lesion vascularity.
Mammogram finding
Large well-defined oval shaped medium density mass in the left breast lower inner quadrant (Figure 1).
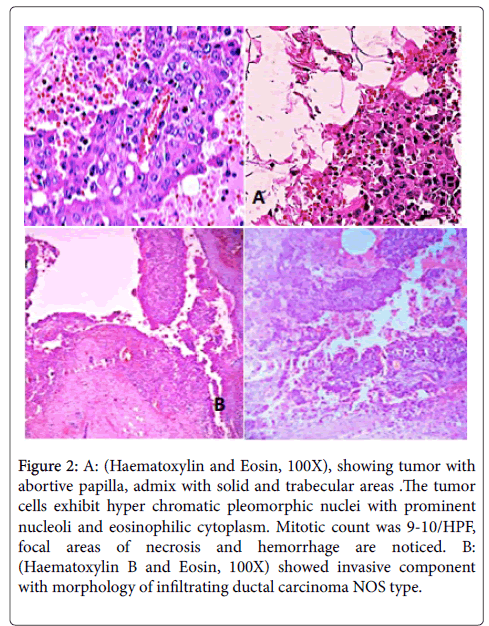
Patient underwent wide local excision of left breast lump with sentinel lymph node biopsy. On gross examination excised specimen measures 7 × 5 × 3 cm, it was well circumscribed. Cut section showed a cystic mass measures 4 × 3.4 × 2 cm filled with friable papillary greyish white tumor mass. The surrounding area shows irregular greyish white tumor measuring 3 × 0.1 × 1cm. The margins of excised mass appeared grossly uninvolved by the tumor. Histopathological examination shows tumor arranged in abortive papillary and focal solid and trabecular pattern with individual tumor cells showing hyper chromatic pleomorphic nuclei with prominent nucleoli and moderate eosinophilic cytoplasm (Figure 2).
Figure 2: A: (Haematoxylin and Eosin, 100X), showing tumor with abortive papilla, admix with solid and trabecular areas .The tumor cells exhibit hyper chromatic pleomorphic nuclei with prominent nucleoli and eosinophilic cytoplasm. Mitotic count was 9-10/HPF, focal areas of necrosis and hemorrhage are noticed. B: (Haematoxylin B and Eosin, 100X) showed invasive component with morphology of infiltrating ductal carcinoma NOS type.
Mitotic count was 9-10/HPF. Focal areas of necrosis and hemorrhage evident in between the papillae. The encysted papillary area measures 3 cm in maximum diameter (Figure 2). Surrounding breast parenchyma showed an invasive component with the morphology of infiltrating duct carcinoma (NOS) type, it measures 0.7 cm in maximum diameter.
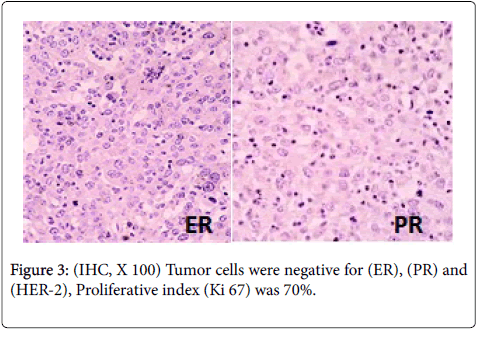
Final histopathological diagnosis given was intracystic papillary carcinoma, high grade with invasive component. Immunohistochemistry (IHC) study show complete negativity for all myoepithelial markers in both the encysted and the invasive component which is usually the case with such type of cases. The hormonal receptor revealed tumor cells were negative for estrogen (ER), Progesterone (PR), Her2/neu suggestive of high-grade to moor (Figure 3). Patient was referred for adjuvant treatment and was free from disease after (Hematoxylin and Eosin, X 100) (Figure 2) showing tumor with abortive papilla, admix with solid and trabecular areas. The tumor cells exhibit hyper chromatic pleomorphic nuclei with prominent nucleoli and eosinophilic cytoplasm. Mitotic count was 9-10/HPF, focal areas of necrosis and hemorrhage is noticed. B: (Haematoxylin B and Eosin 100X) showed invasive component with morphology of infiltrating ductal carcinoma NOS type.
Discussion
The papillary carcinoma of the breast is characterized by a papillary growth pattern with thin fibro vascular stalk lined by neoplastic epithelial cells. Malignant papillary neoplasms of the breast consist of a wide spectrum of lesions that include ductal carcinoma in situ arising in intra ductal papilloma, papillary DCIS, encapsulated papillary carcinoma, solid papillary carcinoma and invasive papillary carcinoma. Lack of myoepithelial cell layer within papillae differentiates benign papillary neoplasm from malignant papillary neoplasm [4]. Intra cystic papillary carcinoma is a solitary, centrally located malignant papillary proliferation within an encysted or cystically dilated duct. IPC was considered to be a variant subtype of DCIS but a recent review of literature shows its association with DCIS or invasive breast cancer in about 40% cases [5]. In IPC (pure) form, solid papillary tumor is confined within a cystic dilated duct without DCIS or invasion into the surrounding tissue. A minority of IPC may be associated with invasive component without features of papillary tumor but rather show morphological features of invasive ductal carcinoma, not otherwise specified type [4]. Similar morphological features were noted in our case. Detection of associated pathology (DCIS or invasive form) is the mainstay as prognosis? and treatment modalities depend upon these associated lesions [6]. Usually intra cystic papillary breast cancers reveal low or intermediate nuclear grade without necrosis. They show strong immunopositivity for estrogen and progesterone receptor and negativity for Her2 net [7]. IPC associated with invasive carcinoma are of high nuclear grade and necrosis. In our case IHC study showed ER, PR, SMA, Her2 net negativity with high proliferation index. Histopathological findings revealed high nuclear grade and necrosis.
Papillary carcinoma of breast generally occurs in elderly postmenopausal women aged 63-67 years. Clinically, patient presents with palpable mass or bloody nipple discharge. It may also manifest as asymptomatic lesion identified at screening mammography. Radiological findings may show on mammography as an oval lobulated, circumscribed lesion and on USG as a complex cystic mass with solid component but differentiation between invasive and papillary DCIS is difficult and requires histopathological confirmation [8].
Cytological diagnosis may be inconclusive as aspirate from cystic component yield hemorrhagic fluid, most of the time which could be negative for malignancy and give false negative result as occurred in our case. Ultrasound guided core biopsy of suspected intra cystic mass has been suggested by many authors to differentiate benign from malignant papillary neoplasms but failed to distinguish in situ from invasive papillary carcinoma as invasion is found in peripheral part of the tumor [9]. Tomonori et al. [10] also suggested necessity of excisional biopsy. FNA and core needle biopsy have not found sufficient most of the time.
Review of literature showed 12 high-grade EPCs without associated conventional stromal invasion. To further characterize these highgrade tumors, a series of invasive papillary carcinomas were assessed for the coexistence of EPC. The literature was also reviewed. Approximately 3% of pure EPCs showed high-grade features as defined by nuclear pleomorphic and increased mitotic activity. These tumors not only showed histological features associated with aggressive behavior, but were also often hormone receptor-negative, tended to be of larger size, and were more frequently associated with stromal invasion. Of the 10 patients with follow-up data, one with pure high-grade EPC developed recurrence and died of her disease. No definitive guidelines for treatment of IPC. In case of IPC alone, IPC with DCIS and IPC with invasion complete surgical excision of the tumor with clear surgical margins is the recommended surgical management [11,14]. Sentinel lymph node biopsy may be alternative to full axillary dissection in patient with IPC and associated invasive carcinoma [12]. Wide local excision was performed in our case in view of atypical ductal epithelial cells on cytology and sentinel lymph node biopsy was not done. Data published in many articles recommends adjuvant radiotherapy for IPC associated with invasion and or DCIS. Mayanja et al. [6] concluded that most important factor determining use of radiotherapy and endocrine therapy is associated pathology and patients with pure IPC were less likely to undergo radio and endocrine therapies.
Although rare, IPC has an excellent prognosis. The largest reported study of 917 cases carried out on IPC patients found no difference in the relative cumulative survival rate in the patients with IPC alone or associated invasive cancer followed up at 10 Years [13].
Conclusion
High grade encysted papillary carcinoma is seen associated with invasion usually its triple negative and behave like invasive counterpart.
Ethics Approval and Consent to Participate
This retrospective study was performed in compliance with the ethical committee of the University of Taif.
Authors’ contributions
EJ was responsible for the acquisition of all necessary data and their interpretation and for the draft of the manuscript. MB contributed equally to drafting the manuscript. AS helped to revise the manuscript. SS, DN, FJ, SA, JJ conceived of the study, and initiated its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Acknowledgement
Almamlka Lab, KSA for their support.
References
- Rosen PP (1997) Papillary carcinoma. In: Rosen’s breast Pathology. Lippincott Raven: Philadelphia, USA, pp: 335-354.
- Carter D, Orr SL, Merino MJ (1983) Intracystic papillary carcinoma of the breast. After mastectomy, radiotherapy or excisional biopsy alone. Cancer 52: 14-19.
- Baykara M, Coskun U, Demirci U, Yildiz R, Benekli M, et al. (2010) Intracystic papillary carcinoma of the breast: one of the youngest patient in the literature. Med Oncol 27: 1427-1428.
- Pal SK, Lau SK, Kruper L, Nwoye U, Garberoglio C, et al. (2010) Papillary Carcinoma of the breast: An overview. Breast Cancer Res Treat 122: 637-645.
- Calderaro J, Espied M, Duclos J, Giachetti S, Wehrer D, et al. (2009) Breast Intracystic papillary carcinoma: an update. Breast J 15: 639-644.
- Fayanju OM, Ritter J, Gillanders WE, Eberlein TJ, Dietz JR, et al. (2007) Therapeutic management of intracystic papillary carcinoma of the breast: the roles of radiation and endocrine therapy. Am J Surg 194: 497-500.
- Leal C, Costa I, Fonseca D, Lopes P, Bento MJ (1998) Intracystic (encysted) papillary carcinoma of the breast: a clinical, pathological, and immunohistochemical study. Hum Pathol 29: 1097-1104.
- Liberman L, Feng TL, Susnik B (2001) Case 35: Intracystic papillary carcinoma with invasion. Radiology 219: 781-784.
- Benkaddour YA, Hasnaoui SE, Fichtali K, Fakhir B, Jalal H, et al . (2012) Intracystic Papillary Carcinoma of the Breast: Report of Three Cases and Literature Review. Case Reports in Obstetrics and Gynecology 2012: 979563.
- Tomonori K, Takayuki S, Tadahiko T, Hojo S, Akashi-Tanaka S, (2009) Clinical and pathological features of intracystic papillary carcinoma of the breast. Surg Today 39: 5-8.
- Harris K, Faliakou E, Exon D, Nasiri N, Sacks NP, et al. (1999) Treatment and outcome of intracystic papillary carcinoma of the breast. Br J Surg 86: 1274.
- Solorzano CC, Middleton LP, Hunt KK, Mirza N, Meric F, et al. (2002) Treatment and outcome of patients with intracystic papillary carcinoma of the breast. Am J Surg 184: 364-368.
- Grabowski J, Salzstein SL, Sadler GR, Blair S (2008) Intracystic papillary carcinoma: a review of 917 cases. Cancer 113: 916-922.
- Rakha EA, Varga Z, Elsheik S, Ellis IO (2014) High-grade encapsulated papillary carcinoma of the breast: an under-recognized entity. Histopathology 66: 740-746.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 5129
- [From(publication date):
April-2017 - Jul 11, 2025] - Breakdown by view type
- HTML page views : 4251
- PDF downloads : 878