Review Article Open Access
An Integral Concept of Regulating Immune Homeostasis
Zemskov Andrey M1 and Zemskov Vladimir M2*
1Department of Microbiology of Burdenko Voronezh State Medical Academy, Voronezh, Russia
2Clinical Immunology Group of Vishnevsky Institute of Surgery, Moscow, Russia
- *Corresponding Author:
- Zemskov Vladimir M
Clinical Immunology Group of Vishnevsky Institute of Surgery
Moscow, Russia
Tel: +79161548170
E-mail: arturrego@netvox.ru
Received date: Feb 01, 2016; Accepted date: April 04, 2016; Published date: April 07, 2016
Citation: Andrey ZM, Vladimir ZM (2016) An Integral Concept of Regulating Immune Homeostasis. J Clin Exp Pathol 6:267. doi: 10.4172/2161-0681.1000267
Copyright: © 2016 Andrey ZM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Clinical & Experimental Pathology
Abstract
The problem of regulating immune reactivity is discussed. The role of various nonspecific internal and external factors that influence the clinical course of diseases and their nature, pathogenesis, organ and tissue localization, developmental stages of allergization, associations of various diseases (including a concomitant pathology of consistent and different genesis), and ongoing treatment on the development of immunopathology and the effectiveness of immunocorrection disease therapy are considered in detail. Types of targeted immunocorrection are discussed
Keywords
Immune reactivity; Immunocorrection; Immunopathology; Immunoreaction
Abbreviations:
CNS: Central Nervous System; RNA: Ribonucleic Acid; FDIS: Formulas Disorders of the Immune System; ABO system: Genetic System of Blood; Rh factor: Rhesus; cAMP\cGMP: Adenosine Monophosphate Cyclo\Guanosine Monophosphate Cyclo; PI: Phagocytic Index- average number of bacteria in the phagocyte after 30 and 120 minutes after the start of phagocytosis; CIC: Circulating Immune Complexes; MSM: Medium Mass Molecules-the criterion of endogenous intoxication, breakdown products of proteins 500 to 5000 Da; T-and B-Lym: T- and B-Lymphocytes
Introduction
It was established definitively that the immune system performs the following important functions: (1) elimination of exogenous and endogenous subjects containing foreign genetic information (xenogenic and allogenic, automodified, malignant, and aging cells); (2) cell fertilization by spermatozoon; (3) anatomical development of fetus; (4) induction of childbirth; (5) realizing of aging; (6) regulation of metabolic homeostasis, etc. These processes are based on specific (concrete) and nonspecific (body-wide) reactions. However, the first is determinant; it is more delayed, insignificant, and inertial than the second [1]. Inductors of immunoreactions are (1) a solid high frequency mutation of lymphoid cells, producing almost every type of antibody with antigen-related selection and cloning of approximate lymphocytes; (2) transferal of infection and carriage of bacteria; (3) the presence of cross-reacting antigens in representatives of normal intestinal flora; (4) the formation of an anti-idiotype cascade carrying an immunological internal image capable of providing a specific “antibody” immune response; (5) release of antigens stored in an organism when the membrane permeability of cells is increased due to endo- and exotoxin activities, corticosteroids, low-molecular nucleic acids, radiation, and other factors [2,3]. We are of the opinion that there are three dynamic phases of the condition of immune reactivity in situ . The first is background; with minimal activity determined by two above mechanisms (nonspecific and specific) provided “routine” resistance. The second is the phase of activity, inducted while the pathological process is developed; this phase consists of a nonspecific inflammatory response and primary stimulation of a specific antigenrelated immune response. The third is the phase of normalization and the formation of immune memory. Since the duration of immune reactivity variations in disease is longer than the achievement of clinical remission and recovery, usually only the second phase of the activation of host defence mechanisms is analyzed in the immunoassay of patients in the acute stage [4,5].
Internal Control Factors and their Integration
Immunoglobulins and products of their degradation under certain conditions, stimulate or inhibit immune response; Fc-fragment debris increases the migration and viability of polymorphonuclear leukocytes, stimulates presentation of the antigen by A-cells, contributes to the activation of T-cells, and accelerates thymic-dependent antigen immunoreaction. Interleukins causes a direct effect on the functional activity of the immune competent cells and regulate immune response. Interferons not only implement an antiviral effect but regulate immunoreactions. Complement system causes opsonization of microorganisms (which makes their absorption by phagocytes easier), activation of leukocytes and their transferal to inflammatory tissue, direct lysis of infectious agents, processing of immune complexes, induction of specific antibodies, etc. Myelopeptides are synthesized by bone marrow cells no allogenic or xenogenic barriers, stimulate antibody production at the peak of the immune response, including a deficit of antibody-producing cells in the case of using poorly immunogenic antigens, T- and B-lymphocytes and macrophages are targets for modulators.
Thymus peptides (thymomimetics) are constantly synthesized by the thymus. They are having been obtained from the thymus: tactivin, thymalinum, thymopoietin, etc. With reduced immune status decrease, thymus modulators increase the number of T-lymphocytes and their functional activity, contribute to the transformation of immature Tlymphocytes to adult, and stimulate the process of detecting thymic-dependent antigens, as well as helper and killer activity. They activate the formation of antibodies, delete immune tolerance, increase α- and γ-interferons, intensify phagocytic reactions, and stimulate factors of nonspecific antiinfectious resistance and tissue regeneration processes.
Central nervous system: The connection between the CNS and the immune system is well supported. Mediators of the immune system are formed in CNS cells: interferon, interleukins, tumor necrosis factor, thymomimetics, etc. Neurons and immunocompetent cells have common receptors. Chemical compounds stimulating training (nerve growth factor) can potentiate immunoreactions.
Endocrine system: It has long been established that endogenous hormones are the main regulators of immune homeostasis. The spectrum of activity of these compounds includes nonspecific stimulation and the suppression of specific immunoreactions. There is a dose-effect dependence, in which low concentrations are activated and high concentrations are suppressed by immune mechanisms.
Metabolic immunosuppression is induced by a disturbance in the cell membranes of intensely functioning cells and an increase in the content of lipid peroxygenation, peracid, diene conjugate of fatty acid, malondialdehyde, anomalous metabolites of lipid exchange (oxidative modificated cholesterol, low-density, and very low density lipoproteids), and glycosaminoglycane in the blood.
Metabolic immunomodulation: The main role of immune deficit in stress and pathology is a decrease in antioxidant protection and an extension of the cell membrane’s lipid peroxidation. In the first case there are superoxide dismutase, catalase, glutathione peroxidase, and glutathione reductase and proteins containing metals with mixed valences (transferrin, ferritine, and ceruloplasmin). In the second case - carotenoids (β-carotene and retinol), tocopherols, polyunsaturated phospholipids, ascorbic acid, glutathione, some amino acids, urea, uric acid, and selenium compounds. Very important is essential which activates the absorption and digestion functions of macrophages, development of the T-dependent and T-independent immune responses.
Enzymatic immunomodulation: Proteolytic and glycolytic enzymes of medical purpose occupy a special place among metabolic immunomodulators. Activation of the endogenous and exogenous (entering into an organism) of a protease has a pronounced influence on the various forms of T-dependent immune response. Proteolytic enzymes influence the receptor apparatus of lymphocytes, the migration of T- and B-lymphocytes, and proliferation of lymphocytes of peripheral blood. They also function as T-mitogens.
Inhibitory factor: At the peak of antibody response, albumin factor, which temporarily decreases the activity of IgM antibodies without influencing their concentrations, is formed in the liver. Thus, excessively strong reactions of humoral immunity are inhibited [6].
Nucleic modulation: There is good reason to believe that an accumulation of low-molecular nucleic acids in the initial period of development causes stimulation of the growth of microorganisms of different taxonomic groups, the selection of virulent clones, and an intensified production of exotoxins, which leads to potentiation of infections thereby induced in the organism. These substances enhances: 1) natural antimicrobial and antiviral resistance, 2) antibiotic sensitivity bacteria, 3) functions of phagocytes, 4) the formation of interferon, 5) detoxication of bacterial exotoxins, 6) of cellular and humoral immune responses, 7) activation of stem cells and T-helper migration, 8) cooperation of T- and B-cell, 9) “revaccination” effect induced as the result of stimulation of T- and B-cell cooperation, redeposition of antigens. Immunomodulation provided 1) by the pluripotent influence of low-molecular RNA on metabolic and immune processes; 2) tissue regeneration caused by positive changes in the synthetic processes in the organism; 3) a radioprotective effect via activation of metabolic processes in cells, 4) the stimulation of bone marrow, 5) and the potentiation of immunoprotective and nonspecific antiinfectious resistance; 6) desensitization caused by modulation of the suppressor level immunity, stabilization of membranes and the enzymatic system, which destroys biogenic amines and other mechanisms [7-9].
Genetic markers of blood: IR and other genes that control antigens of the ABO system, Rh factor, and serum haptoglobins regulate the exhibition and character of immune disorders, the effectiveness of pharmacologic correction, clinical progression, relapses, synchronization diseases, etc.
Integration of internal factors: Functions of the immune system have a “degrading” and integrated orientation. At the same time, by focusing on the destruction (degradation) of immunoreaction targets, they cause the accumulation of many factors facilitating integrative processes. These can be divided into intersystemic (between immune and hematological criteria), intrasystemic (between immune criteria), and nonsystemic (between immune, biochemistry, etc. criteria) mechanisms. This is discussed in detail in our publications [10].
Outer Regulated Factors
These include diet and bloodletting, has on the immune system of immunostimulating or immunosuppressive action depending on dose.
Diet: It is known [11]: (1) a diet with no animal proteins increases the formation of immune globulins; (2) exclusion of nucleic acids from the diet, even in significant calorific value, suppresses cellular immunity; (3) the same effect is determined by vitamin deficiency; (4) a lack of zinc leads to secondary immune deficiency in the main components of immune system and fasting for days decreases immune reactivity and total resistance.
Bloodletting: Bloodlettings in physiological doses stimulate antibody response to a wide range of antigens. Found [12]: (1) the volume of phlebotomy in 0.5-0.8% of body weight after 3-5 treatments every 5-10 days at 4-64 fold increase the synthesis of normal antibodies to many bacterial pathogens that after reaching peak within 1-2 weeks of initial titers drop to or below a further 4 weeks increase again; (2) for bloodletting at a higher level - activity (avidity, affinity) of macromolecular antibody dramatically reduced, without blocking of process of their formation by inhibiting the effect of hepatic factor, the nature of the protein [6]. However, very important are the other (other effects are detailed below).
We have developed specific formulas disorders of the immune system (FDIS), taking into account three basic significantly more variable immune parameters. This allows us to objectively examine the specific changes in the immune system (immunopathology) of patients with a variety of diseases and the impact on the state of various factors. It turned out that this has influenced the clinical course of diseases, their pathogenesis, localization, character, stage, and presence of concomitant allergic complications. In each case, they had their respective FDIS. Before you calculate the formulas disorders of the immune system (FDIS) is necessary to determine the degree of immune disorders for which we developed a universal formula, because not every formation immunodeficiency or immune hyperfunction is the basis for the appointment of immunomodulators [13]:
If the calculated value is "minus" sign, the patient is determined by the deficiency of the immune system (DIS), and "plus" - hyperactivity of the immune system (GIS). When the obtained value is in the range from 1 to 33%, this corresponds to the first degree of immune disorders or hyperactivity, of 34 to 66% - the second, more than 66%- the third. In the latter two cases, the elimination of immune disorders or hyperactivity is a must, and the differences are considered to be significantly different from that of the norm. Further defined qualitative characteristic of disorders of the immune system by calculating the coefficient of the diagnostic value of the following formula [13]:
Where δ- standard deviation, M1 and M2-the arithmetic mean value of immune and laboratory parameters in patients groups. The smaller the value Kj, the more active is different from the specified level.
Finally, FDIS calculated based on the lowest values Kj, which includes three key parameters that are most different from the level of the norm of the vector indicating the direction and degree of these dynamics changes- e.g., chronic bronchitis FDIS has the form-T3-B2- IgA2-, that corresponds to a given pathology deficit 3rd degree T-Lym, 2nd degree B-Lym and 2nd degree of IgA, - ie, the localization of the pathological process in the lungs was observed preferential suppression of T-dependent and two in-dependent indicators. The FDIS - B3-Tc3- CIC3+ - deep in deficit-B-Lym and cytotoxic T-Lym amid a sharp increase in the content of circulating immune complexes; or - PI3+MSM2-CIC3+ - increase in phagocytic index and circulating immune complexes 3rd degree and a deficit of 2nd degree medium mass molecules.
Under similar localization of clinical entities, such as non-specific inflammatory lung diseases (acute (FDIS - T2 -IgM1 -IgA2-), protracted (FDIS- T2 -B2 -IgM1-) and chronic (FDIS- T3 -IgA2 -IgM2-) pneumonia, exogenous (FDIS- T2 -B2 -IgA2-) - and endogenous (FDIS- T3 -B2 -IgA3-) asthma, chronic bronchitis (FDIS- T3 -B2 -IgA2-), infectious lung destruction (FDIS- T3-B3 -IgA2-) change FDIS (state immunopathology) had similarities-in all cases, a significant decrease in T-cells, B-lymphocytes - in five of the seven cases, IgA - in six out of seven. In other words, the localization of the pathological process in the lungs was observed preferential suppression of T- dependent and two B-dependent indicators. Approximately the same pattern observed in the localization of the disease in the digestive system (stomach ulcer (FDIS-T2 -B2 -IgA2-), duodenalulcer (FDIS-T2 -B2 -IgA2-), nonspecific ulcerative colitis (FDIS-T2 -B2 -IgA2-), a disease of the resected stomach [FDIS-T2 -B2 -IgA2-]). It is equally important that a variety of diseases, burdened by a true allergy, characterized by significant changes in immunopathology. The symptoms and clinical status in these pathologies are not used in calculating FDIS, since it carried out only on the basis of indicators of immune-laboratory status. The classification of symptoms and clinical course of disease in these patients was performed according to the standards developed by the Ministry of Health of Russia [11,14]. Influence of combinations of diseases. A recent achievement is the determination of the wide variability of immune reactivity terms, typical reactions, and the selection of targeted immune correction. This situation is simple if the patient has only one disease but becomes ambiguous if there are several pathological processes, providing all the more reason for a lack of research on a specific assessment of the influence on immune profile of certain factors of combined pathology. Influence of combined pathology of homogenous genesis. Estimation of the immune status in patients with bronchial asthma and chronic pneumonia showed that there was an imbalance of parameters in the first case, a suppression of immune reactivity in the second case, and summary suppression of immune reactivity in the third case. Thus, immune disorders that are typical for chronic pneumonia prevail in combinations of pathological processes. In patients with variants of more serious diseases (corticodependent asthma and chronic obstructive bronchitis), the expressiveness of immune disorders was much higher and the compositions of FDIS in all three cases of diseases were different. In patients suffering from duodenal and stomach ulcers there were 3-4 parameters that were abnormal. In the case of combinations of pathological processes, there were 6. In this case FDIS variations were monotone with the availability of monodiseases. In the study of the impact of comorbidity of various origins and managed to find its own characteristics in the change of immunopathology in patients. Many facts have been accumulated regarding the influence of practically any therapeutic intervention on immune parameters, aside from the main effect. At the same time, most antibiotics with a wide spectrum (antihistamines, anti-inflammatories, narcotic drugs with immune suppression activity, macrolides, methabolics, antioxidants, replacement plasma solutions, and vitamins) have a stimulating effect. Moreover, they also exert influence on the metabolic chains-on protein, lipid, and carbohydrate exchanges and on modulation of the cyclic cAMP/cGMP nucleotide ratio. On the other hand, so-called immunotropic interventions actively affect the same biochemistry mechanisms that implement the stimulation or suppression of reparative processes and the modification of the structures and functions of cells of various organs and tissues. Influence of clinical progression on effects of immune correctors
It should be recognized that the obvious fact of the participation of the immune system in the development of any pathological processes is supported in the vast majority of cases by nonspecific methods [15,16]. Indeed, any method of detecting the number of distinct populations and subpopulations of lymphoid cells, level of mediators of immunity, the concentration of immunoglobulins, and the absorbency rate and the metabolic ability of phagocytes, etc., does not test a specific immune response in patients. On the other hand, the range of immunotropic influences, except for the use of serum drugs and vaccine therapy in patient treatment, is also nonspecific in selected observations of “immune” RNA and some other cases. However, such a treatment strategy is positive. It means that the tactic provided correction of specific immune disorders. The immunotropic influences provided by thymic drugs, myelopeptides, corticosteroids, thyrotropic hormones, polysaccharidic and lipopolysaccharidic drugs, nucleic derivatives (sodium nucleinate, encad, ridostin, and derinat), its synthetic variants poly-I:C and poly-A:U, methyluracil, pentoxyl, riboxinum, sodium orotate, interferons and interferon inducer, vitamin B, brewer’s yeast, etc., reproduce some naturally occurring situations that are sufficiently effective in their expression but are certainly nonspecific in nature.
Analysis of the data confirmed that the positive activity of modulation was realized generally at the second phase of activation of immunoreactivity via operative stimulation of a wide range of nonspecific low-expressed protective factors over 2-3 weeks. This is commonly perceived by immunologists as the main effect, because the term of clinical laboratory monitoring usually does not exceed several weeks/months. The frequent finding of immune system parameter hyperfunctioning upon the release of patients can serve as proof of this phenomenon.
However, at this period the pathological process “excludes” and “includes” specific populations of competent cells, which are more than 1-2% of all factors and are detected in an immunity status test to intensive immune response. Subsequently, this localized immune response is inhibited, sometimes in the recuperation process or clinical remission. It is already the prerogative of the third phase of normalization or correction of immunoreactivity. It is possible that the modulators assigned to patients take part in the reaction of a feedback cycle. All of the detected mechanisms are under regulated control by endogenous and exogenous factors. We formulated principles of targeted immune correction as a result of these data [11,14,17,18].
Types of Targeted Immunocorrection
Systemic immunocorrection is has a major impact on the main components of the immune system (T-, B- and phagocytal) that can be induced by nonmedical factors, one universal or several drugs (thymical derivates and myelopeptides), synthetic drugs (levamisole, polyoxidonium, and licopid); and a combination of immune stimulators with suppressions. Local immune correction is the activation of local resistance in organs that communicate with the outside environment (urinal, respiratory, and digestive tracts) by kipferon (complex immunoglobulin protein), viferon, superlimph, vilosenum, and other drugs in aerosols, drops, and suppositories. Auxiliary immunocorrection is mediated by membrane-protectors, energizers that normalize oxidative phosphorylation (riboflavin and nicotinamide), activators of glycolysis and the pentose-phosphate pathway (thiamine and riboxinum), the oxidation of free fatty acids (pantothenate and carnitin), stimulators of citric acid cycle (biothinum and lipoate), and a rational combination of traditional drugs with stimulation and suppression features. Thus, the function of immune system that focuses on the elimination of nonself- objects is realized by a complex of specific (immune) and nonspecific reactions, providing the destruction of different targets with the introduction of bioactive compounds, fragments of nucleic acids, endotoxins, acute-phase proteins, products of decomposition of erythrocytes and other tissue with a powerful body-wide effect, which alters the protein, lipid, carbohydrate, and mineral metabolism in the organism.
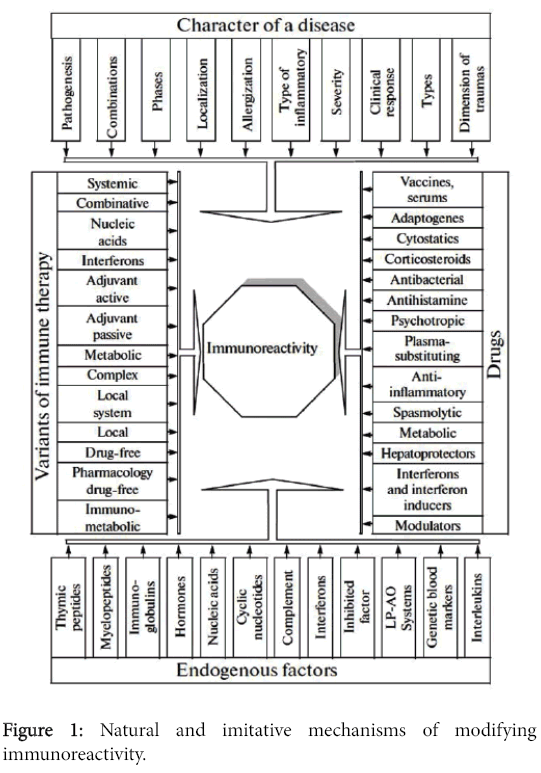
In generally, the factors that regulate immune reactions are shown in the Figure 1. Each of the factors that regulate immune reactions them influences components of immunoreactivity overtly or covertly, increasing it via the stimulation of inter-systemic, non-systemic, and in trasystemic integration. These mechanisms have existed throughout the evolution of all life and are regular participants in the development and elimination of pathological processes. It is hard to declare that one of components (immune, biochemical, endocrine, or others) is the main one. In certain cases, it is determined by the level of laboratory methods used in examining the patient, the erudition of the investigator, and performance targets.
References
- Khaitov RM (2011) Immunologiya (Immunology). Moscow. GEOTAR-Media.
- Burnet F (1969) Cellular Immunology. New York: Cambridge Univ. Press.
- Petrov RV (1987) Immunologiya (Immunology), Moscow: Meditsina.
- Novikov DK, Novikov PD (2009) Klinicheskayaimmunopatologiya (Clinical Immunopathology). Moscow: Med. Liter.
- Belozerov ES, Mitkovskaya OA, Zhdanov KV (2011) Klinicheskayaimmunologiyai al- lergologiya: Rukovodstvo (Clinical Immunology and Allergology: Manual), Elista: Dzha- ngar.
- Zemskov MV, Zhuravleva NV (1977) Yavlenieingibirovaniyaaktivnostiantitel (The Cases of Inhibition of Antibody Activity). ? 69.
- Zem skov VM (1970) [The role of nucleic acids in infection and immunity (review of the literature)]. ZhMikrobiolEpidemiolImmunobiol 47: 65-70.
- Zemskov VM, LidakMYu, Zemskov AM, Mikstays UY (1985) Nizkomolekulyarnaya RNK. Poluchenie, gidroliziprimenenie v meditsine (Low-Molecular RNA: Isolation, Hydrolysis, and Implementation in Medicine). Riga: Zinatne.
- Zemskov V, Zemskov A (1992b) The Immunomodulating Effects of a Low Molecular Weight RNA. Paris: Harwood.
- Zemskov AM, Zemskov VM, Kozlov VA, Suchih GT, Diashev AN, et al. (2007) NelimfoidnyemekhanizmyImmunopatologii (Nonlymphoid Mechanisms of Immunopatho- logy). Moscow: Belyi B ereg.
- Zemskov AM, Zemskov VM, Karaulov AV (1999a) Klinicheskayaimmunologiya (Clinical Immunology). Moscow: Med. Inform. Agent.
- Zemskov MV (1966) Actovayarech (Acts of speech). Voronezh State Medical Institute.
- Zemskov AM, Zemskov VM, Karaulov AV, Novikova LA (1997) Klinicheskayaimmunologiyaiallergologiya. Spravochnikoperativnoyiinformatcii (Clinical Immunology and Allergology. Directory operational information). Voronezh: Voronezh State University.
- Zemskov AM, Zemskov VM, SergeevYuV, Vornovskii VA, Karaulov AV (2003) Tysyachaformulklinichekoiimmunologii (The Thousand Formulas of Clinical Immunology), Moscow: MeditsinadlyaVsekh.
- Zemskov AM, Zemskov VM, Karaulov AV, Zoloedov VI, Vornovskii VA (1999b) Immunnayareaktivnostigeneticheskiemarkerykrovi (Immune Reactivity and Genetic Blood Markers). Moscow: Polidiz.
- Zemskov AM, Zemskov VM, Karaulov AV, Kuprina NP, Malinovskaya VV (2010) Fenotipicheskayamodifikatsiyaimmunologicheskoireaktivnosti (Phenotype Modification of Im-munological Reactivity). Moscow: Mass. Inform. Kommun.
- Zemskov AM, Zemskov VM, Karaulov AV, Kuprina NP, Malinovskaya VV (2010) Fenotipicheskayamodifikatsiyaimmunologicheskoireaktivnosti (Phenotype Modification of Im-munological Reactivity). Moscow: Mass. Inform. Kommun.
- Zemskov AM, Zemskov VM, Mamchik NP, Konovalov IM (2011b) Immunoagressivnoedeistvieekologo-gigienicheskikhfaktorov (Immune Aggressive Effect of Ecological Hygienic Factors). Moscow: Meditsina.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 11133
- [From(publication date):
April-2016 - Dec 19, 2024] - Breakdown by view type
- HTML page views : 10386
- PDF downloads : 747