Research Article Open Access
An Explorative Analysis of Binge Eating Disorder Impulsivity among Obese Candidates to Bariatric Surgery
Fausta Micanti*, Giuseppe Pecoraro, Raimondo Costabile, Giuseppe Loiarro and Diana GallettaDepartment of Neuroscience, Reproductive Science and Odontostomatology, School of Medicine “Federico II” Naples, Naples, Italy
- *Corresponding Author:
- Fausta Micanti
Department of Neuroscience
Reproductive Science and Odontostomatology
School of Medicine “Federico II” Naples, Naples, Italy
Tel: +39 330875129
Fax: +39 0817462372
E-mail: micanti@unina.it
Received date: December 09, 2016; Accepted date: December 24, 2016; Published date: December 31, 2016
Citation: Micanti F, Pecoraro G, Costabile R, Loiarro G, Galletta D (2016) An Explorative Analysis of Binge Eating Disorder Impulsivity among Obese Candidates to Bariatric Surgery. J Addict Res Ther 7:302. doi:10.4172/2155-6105.1000302
Copyright: © 2016 Micanti F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Introduction: DSM-5 included Binge Eating Disorder (BED) in Eating Disorders indicating binge as psychopathological marker. Impulsivity formed by neuroanatomical and psychosocial factors contributes to binge. Obesity mental dimensions: impulsivity, body image, mood and anxiety participate to eating behaviours. They can be distinguished in gorging, snacking, grazing and binge. Impulsivity is generally investigated in obese subjects without making differences among them. This study's aim is to highlight the differences between obese BED and non-BED candidates to bariatric surgery assessing: quantity and quality of impulsivity among eating behaviors; different facets of impulsivity; weight regain after bariatric surgery as consequence of impulsivity disorder.
Methods: 1355 obese subjects underwent psychiatric assessment before bariatric surgery. 984 were selected and enrolled in this study, divided into two groups based on eating behavior: binge eating and gorging/snacking considered as sample of low psychopathology. Every patient underwent psychiatric evaluation. It consists of: psychiatric examination, eating behavior structured interview, impulsivity psych diagnosis: BIS-11, BES and EDI-2. Barratt inner factors: cognitive, motor and non-planning factors were also considered associated with EDI-2 subscales indicating impulsivity. Statistical analysis was performed using Pearson Chi square test, Ancova and TTest. Significance was set at p<0.001.
Results: Data analysis shows a global increase of impulsivity in obese BED versus non BED. Inner impulsivity facets indicate that binge is characterised by increase of CF and MF higher than NPF related to increase of EDI-2 subscales: I, IR, IA, Bu.
Conclusion: This study shows that BED obese subjects suffer from a global impulsivity disorder. The alterations of its inner factors associated to EDI-2 subscales: interoceptive awareness, insecurity and insufficient impulse regulation stress emotional regulation disorder and the inability to control food-intake. This lack of control determines poor compliance after bariatric surgery and weight regain.
Keywords
Binge eating disorder; Eating behaviors; Impulsivity; Bariatric surgery.
Introduction
The Fifth Edition of Diagnostic and Statistical Manual of Mental Disorder (DSM 5) included Binge. Eating Disorder (BED) among the Eating Disorders. BED is defined as “recurring episodes of eating significantly more food in a short period of time than most people would eat under similar circumstances, with episodes marked by feelings of lack of control. Someone with BED may eat too quickly, even when he or she is not hungry. The person may have feelings of guilt, embarrassment or disgust and may binge eat alone to hide the behavior. This disorder is associated with marked distress and occurs, on average, at least once a week over three months” [1]. Before DSMIV TR listed it as an Eating Disorder not otherwise Specified (EDNOS) needed future definition. “This change is intended to increase awareness of the substantial differences between binge eating disorder and the common phenomenon of overeating” (DSM 5) [1,2].
BED is commonly associated with obesity even if many studies underline that it is independent from BMI. Its principal symptoms according to DSM-5 are binge behaviour determining obesity. It is often used as synonymous of BED in an incorrect way. Binge can be symptom among others of psychiatric disorders such as bipolar disorders, psychosis and depression describing the type of food-intake related to the specific mental disorders. BED psychopathological frame is still being studied above all among obese subjects. Researchers stress that excessive concerns about food, body shape and weight, associated with higher depression, higher body dissatisfaction and poorer related quality of life are considered markers of BED [3,4]. However, loss of control provoked by impulsivity is the feature determining binge behaviour [5,6].
Impulsivity can be described as “swift action without forethought or conscious judgment” [7]. Its models are related to brain structure and functioning or to psychosocial mediator. Neuroscience studies distinguish “reward sensitivity” and “rash-spontaneous impulsiveness” [8,9]. Moeller and Barratt considered Self-report impulsivity referring to general impulsivity. They distinguished two types of impulsivity: “response impulsivity”, the inability to withhold a proponent response and “choice impulsivity”, the inability to delay gratification for a larger payout [7,10]. Self-report impulsivity can be evaluated by Barratt Impulsiveness Scale consisting in several subscales forming three factors: attentional impulsivity (CF), motor impulsivity (MF), nonplanning impulsivity (NFP) [11]. Attentional impulsivity is defined as the inability to focus attention or concentrate. Its score seems positively related to volumes of the left medial frontal gyrus, right medial frontal gyrus and left middle frontal gyrus. In BED subjects attentional impulsivity “was related to decreased response inhibition performance and hypoactivity in the prefrontal control network, which was activated when response inhibition was required” [12,13]. Motor impulsivity indicates acting without thinking and it is related to the reward system connected to decision making. Neuroimaging studies show that BED subjects have an increase of activation in food reward regions testifying the difficulty in receiving, processing and integrating body signals. Motor impulsivity, also named response or rapidresponse impulsivity, refers to impairment in the ability to stop motor responses following changes in environmental circumstances [14,15]. Non-planning impulsivity is lack of future orientation or forethought and is related positively to the volumes of the left anterior cingulates gyrus, right middle cingulates gyrus, left middle cingulates gyrus and right orbital frontal gyrus [16]. The differences of impulsivity between obese BED and obese non-BED are not yet clearly defined above all because many studies compare BED to the obese population in general without any distinction of the type of food-intake [17]. Furthermore, there are few studies that consider the difference between BED and binge behaviour [5,18]. The latter can be a symptom of psychiatric or genetic disorders such as bipolar disorder, schizophrenia, Prader Willi and its characteristics can belong to the primary psychopathology or be related to craving [19-24]. Binge in obese BED is associated to food addiction and Impulse control disorder even if the relationship between them is still unclear. Similar to addictive disorders, binge eaters are also less successful in delaying gratification of rewards [25,26]. Schulte stresses that BED and addictive disorders are “marked by loss of control over consumption, continued excess use despite negative consequences, and repeated, failed attempts to cut down on consumption” [27]. Many studies on obesity investigate the different type of food-intake expressed by the eating behaviors. They are: gorging, snacking, grazing, sweet eat-eating and binge distinguished according with the food intake rhythm. Gorging is defined as eating a large amount of food three times a day.
It determines a lower increase of Body Mass Index (BMI) than the other types and it is a more positive index for the therapeutic outcome [28]. Snacking is characterised by frequent assumption of snacks in between meals in a person who generally eats at fast foods [29,30]. Grazing is the repeated ‘‘consumption of smaller amounts of food over an extended period of time with an accompanying sense of a lack of control over this eating’’ [31-33]. Sweet-eating is an eating behavior in which at least 50% of daily consumed carbohydrates consist of simple carbohydrates and which can be triggered by emotional factors [34].
The aim of this is to consider the difference of impulsivity in obese BED compared to a sample of obese non BED candidates to bariatric surgery based on eating behaviors. Gorging and snacking are considered as eating behaviors among obese subjects of low psychopathology [28,29]. We believe that these characteristics allow us to compare impulsivity facets among the obese population of our sample with similar features but with different intensity of mental disorder. Gorging and snacking obese subjects are grouped in non- BED obese subjects. Moreover, to stress: 1) the quality of BED impulsivity compared to our non-BED sample studying the impulsivity inner factors related to disorder of impulse regulation, 2) impulsivity disorder can be the reason of weight regain in long term after bariatric surgery.
Materials and Method
Recruitment
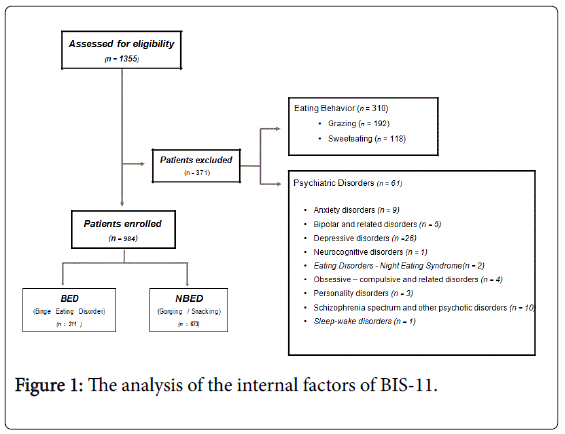
From January 2013 to October 2016, 1355 obese subjects underwent psychiatric assessment before bariatric surgery. The assessment is part of the multidisciplinary program for bariatric surgery at Naples School of Medicine ‘‘Federico II”. Candidates to surgery undergo psychiatric assessment to exclude mental disorders that interfere with weight loss or can worsen after bariatric surgery according with the International Guidelines for Bariatric surgery [35,36] and that of The Italian Society for obesity surgery (SICOb) [37]. Based on the eating behavior we excluded obese with grazing and sweet-eating behaviour because they are considered maladaptive behaviors and have disorders of the mental dimensions of medium intensity [31-34]. For this reason we did not select them as sample to compare with obese BED. According with this exclusion criteria, 984 obese subjects were enrolled in this study. They were visited as outpatients at the Eating Disorder and Obesity Unit specialized in Eating Disorders, Obesity and Bariatric surgery of Department of Psychiatry, University of Naples. Specifically every obese patient candidate to bariatric surgery undergoes psychiatric evaluation to assess the lack of mental disorders and the possibility to cope with post-operation programme. Patients were divided into two groups based on eating behavior: obese with binge as symptoms of BED and subjects with gorging and snacking forming the non-BED sample. Every patient underwent psychiatric evaluation. It consists of: psychiatric examination, eating behaviour structured interview according to the cognitive-behavioural model of Garner and Dalle Grave, psychodiagnosis [38]. Exclusion criteria were: invalid psychodiagnosis; binge as symptom of psychiatric disorder, subjects under psychopharmacological treatment inducing obesity, genetic and metabolic disorder (e.g. Prader Willi) determining craving, grazing and sweet-eating (Figure 1). Demographic features were presented in Table 1. All participants signed an informed consent form before entering the study.
| NOBED pts. 673 | OBED pts. 311 | P-value | ||
|---|---|---|---|---|
| SEX | <0.001a | |||
| F | 406 (60.3%) | 250 (80.4%) | ||
| M | 267 (39.7%) | 61 (19.6%) | ||
| AGE, mean (SD) | 37.37 | -11.6 | 34.05 (10.94) | <0.001b |
| BMI, mean (SD) | 45.98 | -8.6 | 43.71 (10.19) | <0.001b |
Table 1: Demographic characteristics of the sample distinguished by group; aPearson Chi-square test; bT test; OBED: Obese BED subjects; NOBED: Obese non-BED subjects.
Methods
Psychiatric assessment consisted of:
1. Psychiatric examination to exclude psychiatric disorders according to the Diagnostic and Statistical Manual of Mental Disorders-5 (Figure 1) [1].
2. Structured eating interview to identify binge, gorging and snacking eating behaviour [38].
3. Psychometric evaluation performed by rating scales validated for the psychopathological dimension to be investigated: Binge Eating Scale (BES), Barratt Impulsiveness Scale (BIS-11) and Eating Disorder Inventory (EDI-2).
BES is one of the most common instruments used to screen binge eating severity in unidimensional way. It is used to assess the presence of binge eating behavior indicative of an eating disorder [39-41].
BIS-11 was chosen according to the Barratt model of impulsivity for measuring Self-report impulsivity. We considered the Global score to assess impulsivity tendency in general associated to BES Global score; the inner factors of BIS-11 (cognitive impulsiveness-CF, motor impulsiveness-MF, non-planning impulsiveness-NPF) to determine the quality of impulsiveness disorder. [11,42-45].
EDI-2 is a self-reported questionnaire used to assess the presence of Eating Disorders included BED. Specifically the following subscales investigate impulsivity: Bulimia (Bu) indicates episodes of binge eating and purging, Impulse Regulation (IR) shows the ability to regulate impulsive behavior, especially the binge behaviour, Ineffectiveness (I) assesses feelings of inadequacy, insecurity, worthlessness and having no control over their lives; Interoceptive Awareness (IA) measures the ability of an individual to discriminate between sensations and feelings, and between the sensations of hunger and satiety [46]. They were chosen and associated to BIS-11 factors to investigate the quality of impulsivity. Global BES score, BIS-11 total score and EDI-2 Bu subscale were used to assess impulsivity quantity; BIS-11 inner factors and EDI-2 subscales: IR, I, IA to assess impulsivity quality. In this study the analysis of every score and their relationship were be used to clarify the difference of impulsivity between obese BED subjects and obese non BED. This study met the criteria of a cross-sectional design.
Statistics
The Chi square test was used to assess the homogeneity of gender distribution among the groups. T-test was performed to analyse the differences in mean values on rating scales scores in between the two groups of obese subjects with the different eating behaviors. The analysis of covariance (ANCOVA) in a univariate general linear model was performed to test the interaction of age and gender scores as covariates. In all tests, significance was set at p<0.05 (two-tailed). All analyses were carried out using IBM(C) SPSS(C) Statistics version 20.
| Group (OBED/NOBED) *age interaction | Group (OBED/NOBED) *gender interaction | |||||
|---|---|---|---|---|---|---|
| Significance a | Partial Eta squared | Result | Significancea | Partial Eta squared | Result | |
| BES | p=0.863 | <0.001 | No interaction | p=0.466 | 0.001 | No interaction |
| BIS-11 (Ba) | p=0.545 | <0.001 | No interaction | p=0.760 | <0.001 | No interaction |
| - CF | p=0.610 | <0.001 | No interaction | p=0.897 | <0.001 | No interaction |
| - NPF | p=0.467 | 0.001 | No interaction | p=0.866 | <0.001 | No interaction |
| - MF | p=0.729 | <0.001 | No interaction | p=0.247 | 0.001 | No interaction |
| EDI-2 (I) | p=0.153 | 0.002 | No interaction | p=0.560 | <0.001 | No interaction |
| EDI-2 (Bu) | p=0.656 | <0.001 | No interaction | p=0.617 | <0.001 | No interaction |
| EDI-2 (IA) | p=0.329 | 0.001 | No interaction | p=0.298 | 0.001 | No interaction |
| EDI-2 (IR) | p=0.900 | <0.001 | No interaction | p=0.082 | 0.003 | No interaction |
Table 2: Interaction of age and gender on mean scores of each psychopathological dimension among the two groups; aAnalysis of covariance (ANCOVA); OBED: Obese BED subjects; NOBED: Obese non-BED subjects.
Results
Demographics of the sample are reported in Table 1. The distribution of gender throughout the groups was significantly different, with a progressive increase in female percentage in obese non BED (gorging/snacking) and obese BED (binge) groups (Chi square test, p<0.001). Since mean age and gender distribution were significantly different among the two groups, the analysis of covariance (ANCOVA) was carried out in a univariate general linear model to establish whether the significant differences in psychopathology assessment described above may also be affected by these two variables. Results are reported in Table 2. Partial Eta squared scores are also reported as estimates of effect size. No significant interaction was found. The binge behaviour as symptom was found associated to psychiatric disorder (16.2%). Specifically: general anxiety disorder (2.43%), bipolar and related disorders (1,35%), depressive disorders (7,3%), cognitive disorders (0,3%), obsessive-compulsive and related disorders (1,08%), personality disorders (0,8%), schizophrenia spectrum and other psychotic disorders (2,7%), sleep-wake disorders (0,3%),Night Eating Syndrome (6,13%). At Impulsiveness assessment, significant differences were found on the mean Global scores of BES, BIS-11, (T-Test, p<0.001 for each one). In all these assessments, mean scores were significantly higher in obese BED subjects compared to obese non BED (T-test, p<0.001 in all assessments). Significant differences among the two samples were found at BIS-11: CF, MF, NPF, factors (T-test, p<0.001 for each factor).
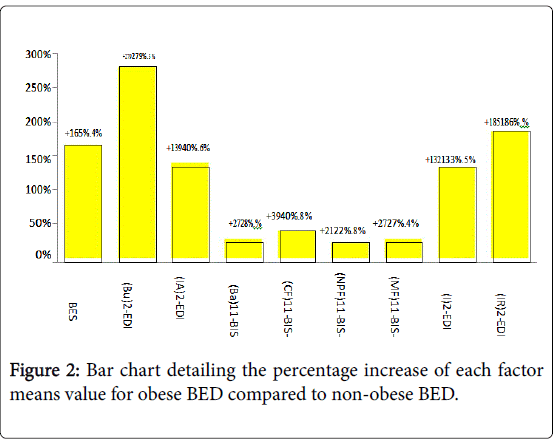
Mean scores were significantly higher in obese BED subjects compared to the other groups (T-test, p<0.001 in all assessments). Results were reported in Table 2. The analysis of the internal factors of BIS-11 showed a higher increase of CF and Mf than NPF (Figure 1). EDI-2 subscales showed a higher increase of IR, I, BU, IA in obese BED subjects compared to obese non BED (Table 3; Figure 2).
| Gorging/Snacking pts. 673 | BED pts. 311 | Total pts. 984 | P-value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| BES | 10.59 (6.38) | 28.11 (6.28) | 16.13 (6.35) | <0.001a |
| EDI-2 (Bu) | 2.22 (2.78) | 8.42 (4.75) | 4.18 (3.40) | <0.001a |
| EDI-2 (IA) | 4.37 (4.42) | 10.47 (6.13) | 6.30 (4.96) | <0.001a |
| BIS-11 (Ba)* | 59.02 (9.57) | 75.44 (11.24) | 64.21 (10.1) | < 0.001a |
| *subscales: | ||||
| Â - BIS-11 (CF) | 13.93 (3.22) | 19.48 (4.44) | 15.68 (3.61) | <0.001a |
| Â - BIS-11 (NPF) | 25.09 (4.75) | 30.57 (4.98) | 26.82 (4.82) | <0.001a |
| Â - BIS-11 (MF) | 20.13 (4.10) | 25.64 (4.85) | 21.87 (4.34) | <0.001a |
| EDI-2 (I) | 4.83 (4.88) | 11.23 (6.61) | 6.85 (5.43) | <0.001a |
| EDI-2 (IR) | 3.06 (3.85) | 8.74 (6.59) | 4.85 (4.72) | <0.001a |
Table 3: Mean scores with standard deviations among the groups for every mental dimension; Notes: aT test; Ba=Barratt; EDI-2: Bu=Bulimia; IA=Interoceptive Awareness; EDI-2: IR=Impulse Regulation; I=Ineffectiveness.
Discussion
Generally obese subjects were considered as a global entity without any difference except for subjects suffering from BED. Previous studies showed that differences exist examining eating behaviours, emotional regulation and the response to food stimuli [47-51]. In this study we selected obese subjects with gorging and snacking behavior that can, in a continuous spectrum, be regarded as subjects with low psychopathology in all obese mental dimensions such as body image, mood and anxiety [28,29] (Table 4).
| Grazing pts. 261 | BED pts. 311 | Total pts. 572 | P -value | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | ||
| BES | 19.72 (6.40) | 28.11 (6.28) | 24.28 (6.34) | <0.001a |
| EDI-2 (Bu) | 4.81 (3.87) | 8.42 (4.75) | 6.77 (4.35) | <0.001a |
| EDI-2 (IA) | 7.03 (4.77) | 10.47 (6.13) | 8.90 (5.51) | <0.001a |
| BIS-11 (Ba)* | 66.36 (9.42) | 75.44 (11.24) | 71.3 (10.41) | <0.001a |
| *subscales: | ||||
| - BIS-11 (CF) | 16.13 (3.52) | 19.48 (4.44) | 17.95 (4.02) | <0.001a |
| - BIS-11 (NPF) | 28.11 (4.58) | 30.57 (4.98) | 29.45 (4.8) | <0.001a |
| - BIS-11 (MF) | 22.12 (4.36) | 25.64 (4.85) | 24.03 (4.63) | <0.001a |
| EDI-2 (I) | 7.8 (5.55) | 11.23 (6.61) | 9.66 (6.13) | <0.001a |
| EDI-2 (IR) | 5.44 (5.00) | 8.74 (6.59) | 7.23 (5.87) | <0.001a |
Table 4: Mean scores with standard deviations among the groups for every mental dimension; Notes: aT test; Ba=Barratt; EDI-2: Bu=Bulimia; IA=Interoceptive Awareness EDI-2: IR=Impulse Regulation; I=Ineffectiveness.
Actually, in our knowledge, there is no study about the differences of impulsivity among obese subjects distinguished by eating behaviours. Moreover they compared obese BED to all obese subjects [17]. The analysis of the peculiar facets of impulsivity in obese BED compared to non-obese BED distinguished by the eating behavior can contribute to highlight the quality of impulsive disorder and establish different therapeutic program for bariatric surgery candidates. Bariatric surgery studies about the possible causes of weight regain highlight that BED is a high risk for weight regain in post-operation period especially in long term [52-56]. Data analysis of BES, BIS-11global score and of EDI-2: Bulimia shows that obese non BED has no tendency to binge. On the contrary, obese BED has high scores of impulsivity stressing that the impulse regulation disorder induces binge. These data are consistent with other study underlining that BED has a peculiar form of dishinibition of the impulse control [9,57-59]. So that impulsivity can be considered among obesity mental dimensions marker of BED psychopathology even if also disorder of body image, anxiety and mood contribute to it [29]. The quality analysis of impulsivity show that obese non BED have low levels of attentional, motor and non-planning factors , with the prevalence of attentional and motor factors. These data can explain their tendency to overeat related to low dysregulation of the inhibition system of the food-related reward [16,17,60,61]. Obese BED has high levels of attentional and motor impulsivity. The high levels of CF and MF related to the high level of EDI-2 Ineffectiveness stressing the inability to control own’s life indicates that the impulsivity disorder is reinforced by feelings of inadequacy and insecurity. These data are consistent with other researches emphasizing the critical role of ineffectiveness in Eating Disorders [62,63]. The increase of Impulse Regulation subscale can be associated to cognitive and motor factors reinforcing the relationship between impulse control disorder and emotional regulation. The arousal of food intake felt by obese BED determining an immediate action could be explained by the interaction of these components. Non planning impulsivity has a higher score than obese non BED but the internal analysis of BIS-11 factors show a less increase. This data is consistent with the other studies [58,59,61] underlining that the inability to think for future (non-planning) seems not to be specific of BED, but can be inserted in the spectrum of Impulse Control disorder to which BED could belong [57,62-67]. Moreover, the high score of EDI-2 Interoceptive Awareness subscale testify the lack of body stimuli perception: specifically the ability to distinguish hunger or satiety signals. It strongly contributes to the complete dysregulation of the impulsive system in obese BED compared to obese non BED. High score of Interoceptive Awareness can be related to high level of Cognitive Factor and affected the reward-related decision making determining the impossibility to stop eating [14,61,67]. Data analysis highlights that impulsivity in obese BED seems to be a very articulated construct formed by disrupt of impulsivity system associated to a dysregulation of the emotional regulation system. These features are peculiar of obese BED impulsive psychopathology compared to obese non BED. This latter have sufficient ability to have control of own’s life and better impulse regulation that associated to the internal prevalence of cognitive factor indicate, according to other studies, the ability to stop and control food-intake [18,28]. Obese non BED show low levels of all the factors examined and for this reason they are able to stop eating, have impulse control and feel satiety. These features are predictor of achieving weight loss and maintenance after bariatric surgery in short and long term [68,69].
Conclusion
This study shows that impulsivity can be considered marker of obese BED psychopathology. Data analysis of the impulsivity facets, according with neurobiological studies indicates that a disorder of the three components occurs. The association with low interoceptive awareness, insecurity and insufficient impulse regulation emphasize that obese BED suffer from disorder of the emotional regulation system. It determines the inability to cope with bariatric surgery program and is a risk for side surgical effects and weight regain in long period. Obese BED need psychiatric treatment before surgery to reduce binge and increase the ability to feel the satiety that bariatric surgery induces. Obese non BED undergoes bariatric surgery without a previous psychiatric treatment according to the substantial regulation of the impulsivity system associated to low psychopathological levels of the other mental dimensions.
Limits
One limit of this study is the lack of control clinical study on the effect of obese BED treatment before bariatric surgery to show that impulse control is sufficient to determining satisfactory weight loss and maintenance after the operation. Moreover no longitudinal data are shown to demonstrate that the association with personality traits such as insecurity, worthlessness and the dysregulation of the hunger-satiety system provoke risk of weight regain. Similarly this study does not show results after bariatric surgery of the effects of low psychopathology of the obese non BED sample.
Contributors
All the authors included in this work have taken part in conceiving the research, in collecting data and interpreting the results. All the authors have contributed to manuscript review. Everyone has approved the final version.
Fausta Micanti has conceived, interpreted and revised the manuscript.
Giuseppe Pecoraro has contributed to subject’s recruitment and follow-up.
Raimondo Costabile has conceived and performed the statistical analysis.
Giuseppe Loiarro has contributed to subject’s recruitment and follow-up.
Diana Galletta has interpreted and revised the psychometric data and revised manuscript.
Fausta Micanti, Giuseppe Pecoraro, Raimondo Costabile, Giuseppe Loiarro, Diana Galletta, declare that no funding source are involved in this study.
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, DSM-5, 5th American Psychiatric Publishing, Arlington, VA.
- American Psychiatric Association (2000) American psychiatric association diagnostic and statistical manual of mental disorders, 4th Edition.
- Dingemans AE, van Furth EF (2012) Binge eating disorder psychopathology in normal weight and obese individuals. Int J Eat Disord 45: 135-138.
- Grilo CM, White MA, Gueorguieva R, Wilson GT, Masheb RM (2013) Predictive significance of the overvaluation of shape/weight in obese patients with binge eating disorder: Findings from a randomized controlled trial with 12 month follow-up. Psychol Med 43: 1335-1344
- Amianto F, Ottone L, Abbate Daga G, Fassino S (2015) Binge-eating disorder diagnosis and treatment: A recap in front of DSM-5. BMC Psychiatry 15: 70.
- Leombruni P, Rocca G, Fassino S, Gastaldi F, Nicotra B, et al. (2014) An exploratory study to subtype obese binge eaters by personality traits. Psychother Psychosom 83:114-118.
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC (2001) Psychiatric aspects of impulsivity. Am J Psychiatry 158: 1783-1793.
- Dawe S, Loxton NJ (2004) The role of impulsivity in the development of substance use and eating disorders. Neurosci Biobehav Rev 28: 343-351
- Schag K, Teufel M, Junne F, Preissl H, Hautzinger M, et al. (2013) Impulsivity in binge eating disorder: Food cues elicit increased reward responses and disinhibition. PLoS One 16: e76542.
- Mitchell MR and Potenza MN (2014) Recent Insights into the neurobiology of impulsivity. Curr Addict Rep 1: 309-319.
- Patton JH, Stanford MS, Barratt ES (1995) Factor structure of the Barrett impulsiveness scale. J Clin Psychol 51: 768-774.
- Cho SS, Pellecchia G, Aminian K, Ray N, Segura B, et al. (2013) Morphometric correlation of impulsivity in medial prefrontal cortex. Brain Topogr 26: 479-487.
- Hege MA, Stingl KT, Kullmann S, Schag K, Giel KE, et al. (2015) Attentional impulsivity in binge eating disorder modulates response inhibition performance and frontal brain networks. Int J Obes (Lond) 39: 353-360.
- Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, et al. (2016) Reward-related decision making in eating and weight disorders: A systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev 61: 177-96.
- Fineberg NA, Chamberlain SR, Goudriaan AE, Stein DJ, Vanderschuren LJ, et al. (2014) New developments in human neurocognition: Clinical, genetic and brain imaging correlates of impulsivity and compulsivity. CNS Spectr 19: 69-89.
- Kessler RM, Hutson PH, Herman BK, Potenza MN (2016) The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev 63: 223-238.
- Schag K1, Schönleber J, Teufel M, Zipfel S, Giel KE (2013) Food-related impulsivity in obesity and binge eating disorder-A systematic review. Obes Rev 14: 477-495.
- Mitchell JE, King WC, Courcoulas A, Dakin G, Elder K, et al. (2015) Eating behavior and eating disorders in adults before bariatric surgery. Int J Eat Disord. 48: 215-222.
- Lopresti AL, Drummond PD (2013) Obesity and psychiatric disorders: Commonalities in dysregulated biological pathways and their implications for treatment. Prog Neuropsychopharmacol Biol Psychiatry 1: 92-99.
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, et al. (2010) Overweight, obesity and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67: 220-229.
- Kivimäki M, Batty GD, Singh-Manoux A, Nabi H, Sabia S, et al. (2009) Association between common mental disorder and obesity over the adult life course. Br J Psychiatry 95: 149-55.
- Lin HY, Huang CK, Tai CM, Lin HY, Kao YH, et al. (2013) Psychiatric disorders of patients seeking obesity treatment. BMC Psychiatry 2: 1-13.
- Schmidt F, Körber S, de Zwaan M, Müller A (2012) Impulse control disorders in obese patients. Eur Eat Disord Rev 20: e144-147.
- Ng L and Davis C (2013) Cravings and food consumption in binge eating disorder. Eat Behav 14: 472-475.
- Davis C, Patte K, Curtis C, Reid C (2010) Immediate pleasures and future consequences. A neuropsychological study of binge eating and obesity. Appetite 54: 208-213.
- Manwaring JL, Green L, Myerson J, Strube MJ, Wilfley DE (2011) Discounting of various types of rewards by women with and without binge eating disorder: Evidence for general rather than specific differences. Psychol Rec 61: 561-582.
- Schulte EM, Grilo CM, Gearhardt AN (2016) Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clin Psychol Rev 44: 125-139.
- Masheb RM and Grilo CM (2006) Eating patterns and breakfast consumption in obese patients with binge disorder. Behav Res Ther 44: 1545-1553.
- Micanti F, Iasevoli F, Cucciniello C, Costabile R, Loiarro G, et al. (2016) The relationship between emotional regulation and eating behaviour: A multidimensional analysis of obesity psychopathology Eat Weight Disord.
- Faria SL, Kelly EO, Faria OP, Ito MK (2009) Snack-eating patients experience lesser weight loss after roux-en-y gastric bypass surgery. Obes Surg 19: 1293-1296.
- Conceicao EM, Mitchell JE, Scott GE, Machado PP, Lancaster K, et al. (2014) What is âÂ?Â?âÂ?Â?grazingâÂ?Â?âÂ?Â?? Reviewing its definition, frequency, clinical characteristics and impact on bariatric surgery outcomes and proposing a standardized definition. Surg Obes Relat Dis 10: 973-982.
- Colles SL, Dixon JB, OâÂ?Â?Brien PE (2008) Grazing and loss of control related to eating: Two high-risk factors following bariatric surgery. Obesity 16: 615-622.
- Lane B, Szabo´ M (2013) Uncontrolled, repetitive eating of small amounts of food or âÂ?Â?grazingâÂ?Â?: Development and evaluation of a new measure of atypical eating. Behav Chang 30: 57-73.
- van den Heuvel M, Hörchner R, Wijtsma A, Bourhim N, Willemsen D, et al. (2011) Sweet eating: A definition and the development of the Dutch Sweet Eating Questionnaire. Obes Surg 21: 714-721.
- Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, et al. (2013) Clinical practice guidelines for the perioperative nutritional, metabolic and nonsurgical support of the bariatric surgery patient-2013 update: Cosponsored by American Association of Clinical Endocrinologists, the Obesity Society and American Society for Metabolic & Bariatric Surgery. Surg Obes Relat Dis 9: 159-191.
- Sogg S, Lauretti J, West-Smith L (2016) Recommendations for the presurgical psychosocial evaluation of bariatric surgery patients. Surg Obes Relat Dis. 12: 731-749.
- Foschi D, Di Lorenzo N, Piazza L (2016) Linee Guida di chirurgia dellâÂ?Â?obesità . SICOb.
- Dalle Grave R (2001) Terapia cognitivo comportamentale dellâÂ?Â?obesità . Verona Positive Press: 249-260.
- Gormally J, Black S, Daston S, Rardin D (1982) The assessment of binge eating severity among obese persons. Addict Behav 7: 981-989.
- Grupski AE, Hood MM, Hall BJ, Azarbad L, Fitzpatrick SL, et al. (2013) Examining the Binge Eating Scale in screening for binge eating disorder in bariatric surgery candidates. Obes Surg 23: 1-6.
- Duarte C, Pinto-Gouveia J, Ferreira C (2015) Expanding binge eating assessment: Validity and screening value of the Binge Eating Scale in women from the general population. Eat Behav 18: 41-47.
- Barratt ES (1965) Factor analysis of some psychometric measures of impulsiveness and anxiety. Psychol Rep 16: 547-554.
- Fossati A, Di Ceglie A, Acquarini E, Barratt ES (2001) Psychometric properties of an Italian version of the Barratt Impulsiveness Scale-11 (BIS-11) in nonclinical subjects. J Clin Psychol 57: 815-828.
- Vasconcelos AG, Malloy-Diniz L, Correa H (2012) Systematic review of psychometric properties of Barratt Impulsiveness Scale Version 11 (BIS-11). Clin Neuropsychiatry 9: 61-74.
- Spinella M (2007) Normative data and a short form of the Barratt Impulsiveness Scale. Int J Neurosci 117: 359-368.
- Garner DM (1991) Eating disorder inventory-2 professional manual. Psychological Assessment Resources, Odessa, FL.
- Gianini LM, White MA, Masheb RM (2013) Eating pathology, emotion regulation and emotional overeating in obese adults with binge eating disorder. Eat Behav 14: 309-313.
- Opolski M, Chur-Hansen A, Wittert G (2015) The eating related behaviours, disorders and expectations of candidates for bariatric surgery. Clin Obes 5:165-197.
- Gade H, Rosenvinge JH, Hjelmesæth J, Friborg O (2014) Psychological correlates to dysfunctional eating patterns among morbidly obese patients accepted for bariatric surgery. Obes Facts 7: 111-119.
- Carter FA and Jansen A (2012) Improving psychological treatment for obesity. Which eating behaviours should we target? Appetite 58: 1063-1069.
- Stice E, Yokum S, Bohon C, Marti N, Smolen A (2010) Reward circuitry responsivity to food predicts future increases in body mass: Moderating effects of DRD2 and DRD4. Neuroimage 50: 1618-1625.
- Masheb RM, Lutes LD, Kim HM, Holleman RG, Goodrich DE, et al. (2015) High-frequency binge eating predicts weight gain among veterans receiving behavioral weight loss treatments. Obesity (Silver Spring) 23: 54-61.
- Bradley LE, Sarwer DB, Forman EM, Kerrigan SG, Butryn ML, et al. (2016) A survey of bariatric surgery patientsâÂ?Â? interest in post-operative interventions. Obes Surg 26: 332-338.
- Kofman MD, Lent MR, Swencionis C (2010) Maladaptive eating patterns, quality of life and weight outcomes following gastric bypass: Results of an internet survey. Obesity (Silver Spring) 18: 1938-1943.
- Meany G, Conceição E, Mitchell JE (2014) Binge eating, binge eating disorder and loss of control eating: Effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev 22: 87-91.
- Karmali S, Brar B, Shi X, Sharma AM, de Gara C, et al. (2013) Weight recidivism post-bariatric surgery: A systematic review. Obes Surg 23: 1922-33.
- Schmidt F, Körber S, de Zwaan M, Müller A (2012) Impulse control disorders in obese patients. Eur Eat Disord Rev 20: 144-7.
- Froreich FV, Vartanian LR, Grisham JR, Touyz SW (2016) Dimensions of control and their relation to disordered eating behaviours and obsessive-compulsive symptoms. J Eat Disord 4: 14.
- Fernández-Aranda F, Pinheiro AP, Thornton LM, Berrettini WH, Crow S, et al. (2008) Impulse control disorders in women with eating disorders. Psychiatry Res 157: 147- 57.
- Meule A (2013) Impulsivity and overeating: A closer look at the subscales of the Barratt Impulsiveness Scale. Front Psychol 10: 177.
- Miller KY and Limberg B (2011) Binge eating behaviors and motoric, attentional and non-planning impulsivity. Graduate Student Journal of Psychology, p: 13
- Kakoschke N, Kemps E, Tiggemann M (2015) External eating mediates the relationship between impulsivity and unhealthy food intake. Physiol Behav 1: 117-121.
- Hamilton KR, Sinha R, Potenza MN (2014) Self-reported impulsivity, but not behavioral approach or inhibition, mediates the relationship between stress and self-control. Addict Behav 39: 1557-64.
- McElroy SL, Keck PE Jr, Phillips KA (1995) Kleptomania, compulsive buying, and binge-eating disorder. J Clin Psychiatry 56 Suppl 4: 14-26.
- Gearhardt AN, White MA, Potenza MN (2011) Binge eating disorder and food addiction. Curr Drug Abuse Rev 4: 201-207.
- Ivezaj V, White MA, Grilo CM (2016) Examining binge-eating disorder and food addiction in adults with overweight and obesity. Obesity (Silver Spring) 24: 2064-2069.
- Fassino S, Pierò A, Gramaglia C, Abbate-Daga G (2004) Clinical, psychopathological and personality correlates of interoceptive awareness in anorexia nervosa, bulimia nervosa and obesity. Psychopathology 37: 168-74.
- Raman J, Smith E, Hay P (2013) The clinical obesity maintenance model: An integration of psychological constructs including mood, emotional regulation, disordered overeating, habitual cluster behaviours, health literacy and cognitive function. J Obes: 240128.
- Livhits M, Mercado C, Yermilov I, Parikh JA, Dutson E, et al. (2012) Preoperative predictors of weight loss following bariatric surgery: Systematic review. Obes Surg 22: 70-89.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 4018
- [From(publication date):
December-2016 - Dec 31, 2024] - Breakdown by view type
- HTML page views : 3273
- PDF downloads : 745