An Examination of Epidemiology, Medical Diagnosis, and Treatment
Received: 01-May-2023 / Manuscript No. ECR-23-94343 / Editor assigned: 04-May-2023 / PreQC No. ECR-23-94343 / Reviewed: 18-May-2023 / QC No. ECR-23-94343 / Revised: 22-May-2023 / Manuscript No. ECR-23-94343 / Published Date: 29-May-2023
Abstract
The most frequent reason for peripartum hysterectomy at the moment is placenta accreta, a serious pregnancy complication. It is becoming a more widespread complication, mostly as a result of the rising prevalence of caesarean deliveries. A prior caesarean delivery, especially when combined with a pre-existing placenta, is the main risk factor for placenta accreta. An important element in enhancing the prognosis for mothers appears to be antenatal diagnosis. Most of the time, ultrasonography can be used to make a diagnosis. Usually, caesarean sections are used to deliver women who have placenta accreta. It is appropriate to plan a caesarean at 34 to 35 weeks in order to prevent an emergency delivery and to reduce prematurity-related problems. To lower neonatal and maternal morbidity and death, a multidisciplinary team approach and delivery at a facility with sufficient resources, especially those for large transfusion, are both necessary. The paucity of randomised controlled trials and sizable cohort studies makes it difficult to determine the best course of action once the neonate is delivered. The best course of action is probably a caesarean hysterectomy. When fertility is desired in a small number of cases, conservative management may be carefully explored. The epidemiology, risk factors, pathophysiology, diagnostic techniques, clinical ramifications, and treatment possibilities of this disorder are all included in the current review.
Keywords
Epidemiology; Diagnosis; Genotype; Medical diagnosis and treatment; Risk factor
Introduction
On the basis of histology, it is classified into three grades: placenta accreta, in which the chorionic villi are in contact with the myometrium, placenta increta, in which they infiltrate the myometrium, and placenta percreta, in which they pierce the uterine serosa. Placenta accreta is regarded as a serious pregnancy problem that may be accompanied by substantial haemorrhage during labour and after delivery that could be fatal. That is now the main reason for urgent hysterectomy. Up to 60% of women with placenta accreta were found to experience maternal morbidity, and up to 7% of these women were reported to die. Moreover, preterm birth and tiny for gestational age foetuses are the main causes of the increased frequency of perinatal problems [1].
Placenta accreta, once an uncommon condition, is now a common pregnancy complication, mostly because the prevalence of caesarean deliveries has increased over the past 50 years. The prevalence of placenta accreta is anticipated to keep rising given that the criteria for caesarean birth appear to be progressively expanding, including caesarean delivery at the mother's request. When compared to earlier estimates from the 1970s and 1980s, which ranged from 1: 4027 to 1: 2510 births, Wu et al. observed an incidence of 1: 533 births during the period from 1982 to 2002, showing that this increase is mostly due to the rising rate of caesarean delivery. A previous caesarean delivery, especially when combined with a pre-existing placenta, has been listed as one of the risk factors for placenta accreta. Placenta accreta risk increases exponentially as the number of previous caesarean deliveries rises [2].
Placenta accreta's precise aetiology is uncertain. Decidua maldevelopment, severe trophoblastic invasion, or a mix of the two is among the suggested hypotheses. Prior instrumentation is thought to be the cause of defective decidualization, aberrant maternal vascular remodelling, excessive trophoblastic invasion, or combinations of these. Accurate preoperative diagnosis of placenta accreta is essential in the therapy of these circumstances because of the substantial morbidity linked to this illness. Prenatal sonography is utilised to guide clinical therapy and support the diagnosis, likely resulting in positive outcomes. Hysterectomy has long been recognised as the only effective treatment for placenta accreta. Conservative solutions, such as keeping the placenta in place entirely or in part when fertility preservation is needed, have also been proposed. Together with surgery, a number of adjuvant strategies have been explored. They included the use of methotrexate therapy and/or the implantation of internal iliac artery balloon catheters prior to surgery for arterial embolization and/or occlusion to lessen intraoperative blood loss and the need for transfusions [3].
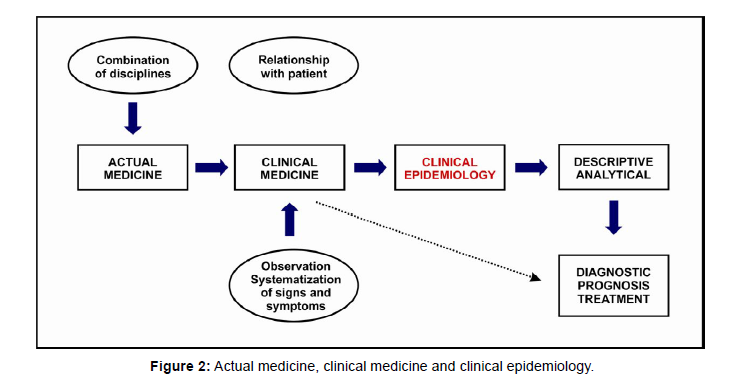
Clinical epidemiology focuses on generating and identifying reliable diagnostic and therapeutic tests, with the ultimate goal of improving patient care. It is an integral part of evidence-based medicine (EBM), which aims to utilize the best available evidence for individual patient diagnosis and treatment. In essence, clinical epidemiology extends the principles of traditional epidemiology, which primarily address population-level public health strategies, to encompass clinical decision-making in the context of individual patient care. By applying the principles of clinical epidemiology, healthcare practitioners can enhance their ability to make informed and evidence-based decisions that directly impact the well-being of their patients shown in (Figure1).
Clinical epidemiology encompasses the entire spectrum of patient outcomes, ranging from the onset of disease to its resolution through healing, sequelae, or death. As a result, the subjects of study in clinical epidemiology are typically individuals who are receiving care in healthcare facilities, and their contributions are particularly relevant, especially in terms of diagnosis and the secondary and tertiary prevention of disease.
Clinical epidemiology can be further divided into descriptive and analytical components. The descriptive aspect focuses on understanding the variations in clinical prognosis, while the analytical aspect delves into investigating the factors that contribute to these variations. These factors include the main predictors for prognosis, diagnosis, and treatment, which are fundamental concepts in both clinical epidemiology and the practice of clinical medicine (Figure 2). While demographic epidemiology primarily addresses the general population, clinical epidemiology has a more specific focus on the individual level. It aims to examine and address the unique characteristics and circumstances that influence the health outcomes of individual patients shown in (Figure2).
Materials and Methods
Data sources: A wide range of data sources were utilized to gather information on epidemiology, medical diagnosis, and treatment. These included scientific literature, research articles, textbooks, public health reports, clinical guidelines, and reputable online databases. The data sources were selected based on their relevance, credibility, and recency to ensure the accuracy and comprehensiveness of the examination.
Literature search: A systematic literature search was conducted using various electronic databases such as PubMed, Google Scholar, and Scopus. Relevant keywords and search terms, such as "epidemiology," "medical diagnosis," "treatment," and specific diseases or conditions, were used to retrieve articles and studies related to the topic. The search was limited to a specific time frame to focus on recent research and advancements [4].
Data collection: Pertinent data related to epidemiology, medical diagnosis, and treatment were extracted from the identified sources. This included information on disease prevalence, incidence, risk factors, diagnostic methods, treatment modalities, clinical trials, and patient outcomes. The data collected were organized and compiled for analysis and synthesis [5].
Data analysis: The collected data were thoroughly analyzed to identify key findings, trends, and patterns. Quantitative data, such as prevalence rates and diagnostic accuracy measures, were subjected to statistical analysis using appropriate statistical software. Qualitative data, such as expert opinions and case studies, were analyzed thematically to extract meaningful information.
Case studies: In order to provide practical examples and insights, relevant case studies were included in the examination. These case studies represented real-world scenarios where epidemiology, medical diagnosis, and treatment were applied. They illustrated the challenges faced, diagnostic approaches used, and treatment outcomes observed. Ethical considerations were taken into account to protect the privacy and confidentiality of individuals involved [6].
Expert consultation: Experts in the fields of epidemiology, medical diagnosis, and treatment were consulted to obtain their perspectives,insights, and expert opinions. These experts were selected based on their expertise and research contributions in the respective domains. Interviews or discussions were conducted either in person, via email, or through teleconferencing. The information obtained from the experts' input was incorporated into the examination to provide a well-rounded understanding [7].
Ethical considerations: Throughout the examination, ethical considerations were carefully observed. Patient privacy and confidentiality were respected, and any personally identifiable information was appropriately anonymized or excluded. The study adhered to the ethical guidelines and regulations outlined by relevant institutions and ethics committees [8].
Limitations: It is important to acknowledge the limitations of the examination. The availability and quality of the data sources, as well as the scope of the research, may have influenced the comprehensiveness and generalizability of the findings. Additionally, the examination was conducted based on existing knowledge and may not capture the most recent advancements in the field [9].
Discussion
Placenta accreta, once an uncommon condition, is now a common pregnancy complication, most likely as a result of the rise in caesarean deliveries over the past 50 years. Around 1 in 1000 births results in placenta accreta, with reported rates ranging from 0.04% to 0.9%. This vast range could be explained by variations in the study population and terminology. The extra uterine organ that is most usually affected by a placenta percreta is the bladder. Significant morbidity and mortality are linked to placenta percreta that invades the urinary bladder [10].
The median parity is 2.5, and the usual maternal age is about 34. The number of prior caesarean deliveries raises the likelihood of having placenta accreta. They range from 2% in those who have only had a placenta previa to 39–60% in those who have had two or more prior caesarean deliveries. Concomitant placenta previa affects up to 88% of women. Submucous myoma, prior curettage, Asherman's syndrome, advanced maternal age, grandmultiparity, smoking, and chronic hypertension are risk factors other than a prior caesarean section. Moreover, 72 cases of placenta accreta that were given conservative care were evaluated by Alanis et al. Prior placenta accreta is probably a significant risk factor as 15% of women who had a subsequent pregnancy experienced a second placenta accreta, meaning that it is likely to occur frequently [11].
Placenta accreta's precise aetiology is uncertain. In hysterectomy specimens, placenta accreta has typically been identified when an area of accretion revealed chorionic villi in close proximity to the myometrium and the lack of decidua. While the decidua is found in regions close to the foci of accreta in certain cases, this result may be localised. Placenta accreta decidual maldevelopment is typically linked to prior instrumentation, such as prior caesarean sections or uterine curettages [12]. Decidua maldevelopment, severe trophoblastic invasion, or mix of both is suggested as possible explanations. According to Tseng and Chou, the primary causes of placenta accretion are the aberrant expression of growth, angiogenesis, and invasion-related factors in the trophoblast populations. Moreover, according to Cohen et al., cytotrophoblast produce substances that encourage invasion, but decidua appears to play a little role in controlling cytotrophoblast invasion in vitro [13].
They contend that increta and percreta are more likely to develop as a result of a scar dehiscing, which gives cells from the trophoblast column better access to large outer myometrial vessels, rather than a pre-existing defect in trophoblastic growth that would produce unfavourable trophoblastic invasion. They contend that excessive trophoblastic invasion is unlikely to play a significant role in the pathogenesis of placenta accreta [14].
It was demonstrated in vitro that a sharp decidual incision mimicking a caesarean section significantly increased the potential for invasion of the trophoblastic cells. Additionally, it was demonstrated that complete approximation of the incised edges of the decidua made the incised decidua behave similarly to intact decidua while limiting the extent of the invasiveness. The invasion capacity of trophoblastic cells in vitro altered in accordance when the same cohort of trophoblast cells was used, highlighting the influence of decidua on the invasion potentiall. Women who have a placenta previa, particularly anterior [15], and a history of caesarean or other uterine surgery should be on the lookout for placenta accreta. The diagnosis of this illness during pregnancy is the main factor influencing the prognosis. It provides the chance to create a delivery plan that accurately accounts for the anticipated blood loss and other potential delivery problems. Also, since the optimal scenario necessitates the involvement of a multidisciplinary surgical team, it provides the chance to electively time the process [16].
The method of choice for making the diagnosis and directing therapeutic treatment is antenatal ultrasonography. Accrual symptoms could appear as early as the first trimester. Comstock looked back into the ultrasound tests done up to 10 weeks gestation in women who later had placenta accreta found on pathological testing. All of them had gestational sacs that were low to the ground and obviously linked to the uterine scar. In comparison to normal early gestational sacs, the myometrium was thin in the region of the scar to which the sac was linked [17].
Placental implantation site, lack of a hypoechoic border (myometrial zone) between the placenta and the myometrium, bulging of the placental/myometrial site into the bladder and increased vasculature evident on colour Doppler sonography, compared threedimensional power Doppler with gray-scale and colour Doppler ultrasonography for the diagnosis of placenta accreta and found that using a composite scoring system of 6 sonographic findings performed with gray-scale and Doppler sonography had 89% sensitivity and 98% specificity [18]. Power in three dimensions Doppler was used to look for angioarchitecture in the placenta's basal and lateral views. The final diagnosis established during the Cesarean delivery was taken into consideration while analysing the ultrasound results. The best single criterion for the diagnosis of placenta accreta, according to the authors, was "many coherent vessels" seen by three-dimensional power Doppler in the basal view, with a sensitivity of 97% and a specificity of 92%. They came to the conclusion that three-dimensional power Doppler could be an additional approach for detecting or ruling out placenta accreta in utero [19].
If the ultrasound results are deemed inconclusive or if the placenta is seen on the posterior wall, gadolinium contrast agent may be administered intravenously during magnetic resonance imaging. Among the magnetic resonance imaging findings suspected of indicating the presence of placenta accreta are placental heterogeneity, mass effect of the placenta into the underlying bladder or extending laterally or posteriorly beyond the normal uterine contour, obliteration of the myometrium zone visible on initial uptake of gadolinium, and a beading nodularity within the placenta. By employing any prenatal diagnostic technique, the doctor can no longer be assured with absolute certainty that a placenta accreta is present. Placenta accreta is often definitively diagnosed postpartum on hysterectomy specimens when a region of accretion displays chorionic villi in direct contact with the myometrium and the absence of decidua [20].
Conclusion
An increasingly frequent pregnancy problem is placenta accreta. For women with placenta accreta, improving counselling, treatment, and outcomes appears to depend heavily on prenatal diagnosis. The best course of action is probably a caesarean hysterectomy. Only extremely rare circumstances may conservative management be employed. Although there may be a reason for adding adjuvant therapy in these circumstances, there is no evidence to support either the benefit of or the absence of risk from such therapy.
Acknowledgement
None
Conflict of Interest
None
References
- Diez Roux AV, Merkin SS, Arnett D (2001) Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 345:99-106.
- Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47:1245-1251.
- Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613-619.
- Westfall JM, Mold J, Fagnan L (2007) Practice-based research-“Blue highways” on the NIH roadmap. J Am Med Assoc 297:403-406.
- Wilson CB (2006) Adoption of new surgical technology. Br Med J 332:112-114.
- Ronco C, McCullough P, Anker SD (2010) Cardio-renal syndromes: report from the consensus conference of the acute dialysis quality initiative. Eur Heart J 31:703-711.
- Goldberg A, Hammerman H, Petcherski S (2005) Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J 150:330-337.
- Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM, et al. (2008) Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med 168:987-995.
- Logeart D, Tabet JY, Hittinger L (2008) Transient worsening of renal function during hospitalization for acute heart failure alters outcome.Int J Cardiol 127:228-232.
- Metra M, Nodari S, Parrinello G (2008) Worsening renal function in patients hospitalised for acute heart failure: clinical implications and prognostic significance. Eur J Heart Fail 10:188-195.
- Drazner MH, Rame JE, Stevenson LW, Dries DL (2001) Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med 345:574-581.
- Rudiger A, Singer M (2007) Mechanisms of sepsis-induced cardiac dysfunction. Crit Care Med 35:1599-1608.
- Brun-Buisson C (2000) The epidemiology of the systemic inflammatory response. Intensive Care Med 26:64-74.
- Parmar A, Langenberg C, Wan L, May CN, Bellomo R, et al. (2009) Epidemiology of septic acute kidney injury. Curr Drug Targets 10:1169-1178.
- Singh AK, Szczech L, Tang KL (2006) Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 355:2085-2098.
- Brinton LA (2015) Prediagnostic sex steroid hormones in relation to male breast cancer risk. Journal of Clinical Oncology 33:18.
- Thomas DB, Jimenez LM, McTiernan A (1992) Breast cancer in men: risk factors with hormonal implications. Am J Epidemiol 135:734-748.
- Mavraki E, Gray IC, Bishop DT, Spurr NK (1997) Germline BRCA2 mutations in men with breast cancer. Br J Cancer 76:1428-1431.
- Haraldsson K, Loman N, Zhang QX, Johannsson O, Olsson H, et al. (1998) BRCA2 germ-line mutations are frequent in male breast cancer patients without a family history of the disease. Cancer Res 58:1367-1371.
- Csokay B, Udvarhelyi N, Sulyok Z (1999) High frequency of germ-line BRCA2 mutations among Hungarian male breast cancer patients without family history. Cancer Res 59:995-998.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar Crossref, Indexed at
Google Scholar, CrossRef Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Citation: Peter J (2023) An Examination of Epidemiology, Medical Diagnosis, andTreatment. Epidemiol Sci, 13: 493.
Copyright: © 2023 Peter J. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2252
- [From(publication date): 0-2023 - Dec 05, 2025]
- Breakdown by view type
- HTML page views: 1913
- PDF downloads: 339