Review Article Open Access
An Evolutionary Concept Analysis of Palliative Care
Qiaohong Guo1*, Cynthia S. Jacelon1 and Jenna L. Marquard21University of Massachusetts Amherst School of Nursing, MA, USA
2University of Massachusetts Amherst College of Engineering, MA, USA
- *Corresponding Author:
- Qiaohong Guo, RN, PhD student
University of Massachusetts Amherst School of Nursing, MA, USA
Tel: 413-687-4854
E-mail: qguo@nursing.umass.edu
Received date: August 02, 2012; Accepted date: August 22, 2012; Published date: August 23, 2012
Citation: Citation: Guo Q, Jacelon CS, Marquard JL (2012) An Evolutionary Concept Analysis of Palliative Care. J Palliative Care Med 2:127. doi: 10.4172/2165-7386.1000127
Copyright: © 2012 Guo Q, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Aim: This paper reports a concept analysis of palliative care in the United States.
Background: There has been a significant development of palliative care in the United States. The early years of 21st century have been characterized by a proliferation of diverse models of palliative care. Methods: A review of literature was conducted to explore the development of palliative care in the United States. Retrieved articles were published in English between years 2004 and 2011. Reference lists from relevant publications were reviewed. Rodgers’s evolutionary concept analysis strategy was used to guide this paper. The matrix method was used to analyze the identified articles.
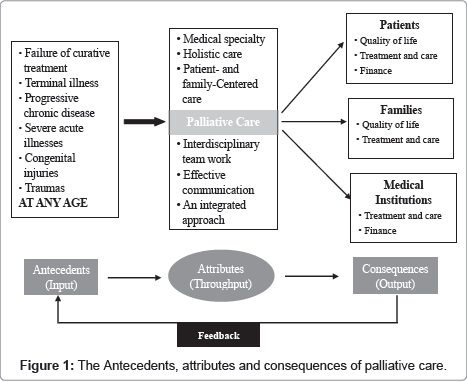
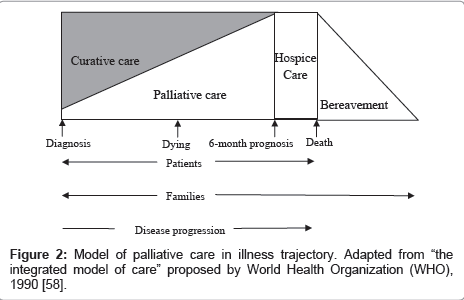
Results: The definition of palliative care has evolved in the United States in recent years. Six attributes were identified: (1) medical specialty, (2) holistic care, (3) patient- and family-centered care, (4) interdisciplinary team work, (5) effective communication, and (6) an integrated approach. The consequences of palliative care for patients, families, and medical institutions were from three aspects: (1) quality of life, (2) treatment and care, and (3) finances. The adapted palliative care model shows that palliative care should be integrated into illness management from the beginning of diagnosis and can be delivered concurrently with curative treatment through the whole trajectory of illness.
Conclusions: Both the definition and application of palliative care have evolved over the last decade. The ultimate success of developing palliative care as a medical specialty will rest upon the integration of the changing concept of palliative care into everyday practice.
Keywords
Concept analysis; Palliative care; Hospice care; United States
Introduction
The U. S. population is aging at increasing rates. By 2030, one in five Americans will be age 65 or older [1]. As more people live to later years, a new pattern of illness is emerging and more and more people are approaching the end of life. Thus, palliative care will be an important part of future medical care in the United States. Data from the 2008 American Hospital Association (AHA) Annual Survey of US Hospitals shows that 1299 hospitals (31%) have palliative care programs today [2]. This represents a rapid increase over the 632 programs reporting palliative care programs in 2000. In addition to rapidly emerging hospital-based palliative care programs, the early years of 21st century have also been characterized by a proliferation of diverse models of palliative care. These diverse models include outpatient palliative care clinics [3], palliative care consultation services [4], palliative care in community and primary care settings [5], and integration of palliative care in acute care hospitals [6]. This rapid growth in palliative care models has raised concerns about the quality of palliative care, particularly at the national level [7]. Two such quality-promoting efforts are the Clinical Practice Guidelines for Quality Palliative Care [8] and a state-by-state report card effort developed by the Center for the Advancement of Palliative Care [9]. These reports identify the characteristics of a quality palliative care program, and programs that include these characteristics.
With the aforementioned upward trends in aging, changing illness trajectories, longer life expectancies, changing goals of care, and advances in health care technologies, the historical view of palliative care has been challenged. The concept of palliative care in the US has evolved to address the needs of a wide range of patient populations who may not be termed “dying” but for whom alleviation of suffering and improvement of quality of life may be relevant goals. Meanwhile, the implementation time of palliative care has been recommended to be the early stage of illness, at the time of illness diagnosis or at the time of symptom onset. This evolution necessitates that every health professional, regardless of his or her clinical specialty, understand the dramatically changing palliative care concept.
Palliative care is a dynamic concept changing with time, understanding of disease and evaluation of what constitutes quality of life and death for people with serious illness [10]. The concept analysis presented in this paper was guided by Rodgers’ evolutionary method of concept analysis [11]. For Rodgers, concepts may be changeable based on contextual or temporal elements. The goal of the evolutionary method of concept analysis is not to search for an absolute truth but for a relative reality that is pragmatic, temporal and context-dependent [10]. Since it has been argued that palliative care “is in the process of dynamic change” [12, p86], an evolutionary method was chosen for the concept of palliative care. The purpose of this paper was to analyze the concept of palliative care based on recent developments in this field, starting from Meghani’s [10] concept analysis of palliative care. In the discussion section the current concept definition will be compared with the findings of Meghani [10]. The goal of this analysis is to explore the evolution of the concept of palliative care, explicate the contemporary meaning of the concept, and compare it with other related concepts such as hospice care and end-of-life care within the context of the US health care system.
Materials and Methods
The authors performed a keyword search of 5 electronic databases including: Medline (PubMed), CINAHL, PsycINFO, Academic Search Premier, and Sociological Abstracts in March 2011. The key words, “palliative care” and “United States” were used in the search. This approach was supplemented by systematic analysis of references cited in all identified articles. Articles were included in the sample if the article: (a) was published in English, with publication year between 2004 and 2011, (b) addressed palliative care in the United States in recent years rather than summarized palliative care from years before 2003, (c) and helped to clarify the concept of palliative care by delineating its evolution, contemporary meaning, antecedents, attributes and consequences. The search strategy yielded 449 articles. Titles and/or abstracts of each article were reviewed, and 328 articles were excluded due to not meeting the inclusion criteria or because of duplicate articles. One hundred twenty one full text articles were obtained for further evaluation. After reviewing these articles based on the inclusion criteria, 35 articles were included in this study. Review of the reference lists of these 35 identified articles yielded 9 additional articles. The final sample included 44 articles. This exceeded the 30 articles that Rodgers stated was the minimum needed to facilitate a credible analysis [13,14]. These 44 articles can be categorized as follows: 14 research articles, 5 review articles, 10 opinion articles, 3 notes, 1 book source, 5 reports, 1 policy documents, 2 clinical guidelines, 2 editorials, and 1 letter. The sample was evaluated according to levels of scientific evidence used by the US Agency for Health Care Policy and Research [15].
The matrix method was used to analyze the identified articles [16]. Information on the definitions, attributes, antecedents, consequences, references, and related terms of the concept of palliative care were recorded in tabular form using Microsoft Excel. The researcher reviewed the listing, then summarized and coded the information in each column. These data were categorized into 5 themes that emphasized the following aspects: (a) definitions of palliative care; (b) antecedents of palliative care; (c) attributes of palliative care; (d) consequence of palliative care; (e) related concepts.
Results
Existing definitions of palliative care
Recently, the definition of palliative care has changed dramatically. In 2002, the World Health Organization (WHO) [17] amended the definition of palliative care as:
An approach which improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual problems (P. 84).
In 2004, the National Consensus Project for Quality Palliative Care [8] defined palliative care in a more detailed way:
Palliative care is medical care provided by an interdisciplinary team, including the professions of medicine, nursing, social work, chaplaincy, counseling, nursing assistants and other health care professions, focused on the relief of suffering and support for the best possible quality of life for patients facing serious life-threatening illness, and their families. The goal of palliative care is to prevent and relieve suffering and to support the best possible quality of life for patients and their families, regardless of the stage of the disease or the need for other therapies. It can be delivered concurrently with life-prolonging care or as the main focus of care (p. 611-612).
Currently, palliative care is recognized as a medical specialty with an inherent interdisciplinary nature by the American Board of Medical Specialties (ABMS) [18]. In the past, it was not widely accepted that curative care and palliative care could exist simultaneously in a patient’s illness management. What is new in the field of palliative care now is the exploration of palliative as a continuum of interventions and better ways to integrate curative treatment with palliative care. Twaddle et al. [19] proposed that: “The continuum of palliative care begins at the time of diagnosis of serious illness and creates a seamless delivery of supportive care for those whose diagnosis can at any time be terminal. The emphasis of palliative care is to clarify the goals of care in the context of the individual patient’s definition of quality and meaning of life. With the goals defined and communicated, care moves from crisis intervention to crisis avoidance, resources for support and advocacy are defined earlier in the illness, and discussions of the burdens and benefits of interventions are recurrently pursued” [19, p87] Carlson et al. [20] asserted that life-prolonging treatments and palliative care can be better integrated, and the shift from predominantly curative to predominantly palliative care can be more gradually managed to reflect the natural course of disease.
Antecedents of palliative care
Historically, an antecedent of palliative care was the inability of curative medical treatment to meets the needs of clients, for which cure was not possible. Terminal illnesses, especially cancer and more recently AIDS, have been two clear antecedents of palliative care [10,21]. More recently, however, palliative care has not been limited to providing services for terminally-ill patients or cancer-diagnosed patients. Research has shown that palliative care can be effective for chronic conditions such as lung disease [22], heart failure [23,24], degenerative neurological diseases [25] and dementia [26]. Palliative care has also been advocated for patients with severe acute illnesses such as those admitted to intensive care settings [27]. Increasing attention has been paid to palliative care for older adults [1] and pediatric patients [28]. The current antecedents of palliative care include not just debilitating illness, acute, serious, and life-threatening illness but also progressive chronic conditions, congenital injuries, chronic and life-threatening injuries from accidents or other forms of trauma at any age.
Attributes of palliative care
From the literature, six attributes of palliative care were identified: (1) medical specialty, (2) holistic care, (3) patient- and family-centered care, (4) interdisciplinary team work, (5) effective communication, and (6) an integrated approach.
Medical specialty: In 2006, palliative care was identified as a medical specialty by the American Board of Medical Specialties (ABMS) [18]. Specialty-level palliative care service means providing services by palliative care professionals within an interdisciplinary team whose work reflects substantial involvement in the care of patients with life-threatening or debilitating chronic illnesses, and their families [8]. As a subspecialty of medicine, education on palliative care has been strengthened, accreditation requirements have been developed and certification exams are required.
Holistic care: Clark and Seymour [29] state that aligning the notion “palliative” to the notion of “care” is the key to understanding this concept because the concept of “care” directs attention from linearity to holism, from patient to care. The goal of palliative care is not to cure but to achieve the best quality of life through providing care that addresses the physical, psychological, social, spiritual, and practical supportive needs of patients and their families. Holistic palliative care not only stresses alleviating suffering from pain and other symptoms but also emphasizes reducing emotional, social and spiritual suffering. In addition, culturally sensitive delivery of care in this increasingly diverse society is a growing priority in today’s health care system [30], and this is likely particularly important in taking care of dying patients.
Patient and family-centered care: Palliative care service should be patient-and family-centered [31]. The family is defined by the patient or, in the case of minors or those without decision-making capacity, by their surrogates. In this context, family members may be related or unrelated to the patient; they are individuals who provide support and with whom the patient has a significant relationship (8, P613). In addition to meeting patients’ physical, psychological, social and spiritual needs, providing services for their family members is also important in of palliative care. These services include: promotion of shared decisionmaking between the patient and family members; attention to the needs of the family members for information and skills for taking care of the patient; physical, emotional and financial supports; promotion of family members’ dignity; provision of bereavement services prior to and after patient’s death; and coordination of care across settings of care and the patient’s illness trajectory [31], and so on.
Interdisciplinary team work: A team-oriented approach to care is a foundation of palliative care [32]. Palliative care teams include a core group of professionals from many disciplines including: medicine, nursing and social work, and may include some combination of volunteer coordinators, bereavement coordinators, chaplains, psychologists, pharmacists, nursing assistants and home attendants, dietitians, physical-, occupational-, art-, play-, child–, life-, and music therapists, case managers and trained volunteers [8]. The different members of the palliative care team bring different perspectives to the patient’s illness experience and diverse expertise towards achieving the common goal of palliative care [33]. From the perspective of both patients and caregivers, high-quality care occurs when the care team controls physical symptoms well, assists with emotional suffering, supports shared decision-making, coordinates care smoothly, provides adequate information, and treats the dying patient with respect and kindness [34].
Effective communication: Effective communication is one of the core elements of quality palliative care [8]. Achieving the goals of palliative care is not possible without effective communication among patients, families, and their interdisciplinary care team [35]. These communication skills include developmentally appropriate and effective sharing of information, active listening, determination of goals and preferences, assistance with medical decision-making, and effective communication with all individuals involved in the care of patients and their families [8].
An integrated approach: Palliative care, including discussion of prognosis and advance directives, management of symptoms and comorbidities, and hospice, should be integrated with optimal medical management at the diagnosis of any serious disease [24,36]. The American Hospice Foundation Guidelines Committee recommends integration of relevant aspects of palliative care in introductory, diagnostic, treatment, and closing sections of management guidelines for all significant illnesses [36]. Palliative care can be delivered in concert with curative or life-prolonging efforts, provided these therapies are of benefit to the patient [8]. In 2005, the 58th World Health Assembly fully integrated palliative care into its resolution WHA 58.22 to improve cancer prevention and control [37]. This resolution recognized palliative care as an essential component of comprehensive cancer care, equal to medical, surgical, and radiation oncology and urged member nations to fully integrate palliative care into their national cancer control programs. The purpose of integrated palliative care is to provide high-quality care for both patients and their families in the whole trajectory of illness.
Consequences of palliative care
With the changing definition of palliative care, the practices of palliative care have increased attention on the effects of early palliative care [19,38-42], integrated palliative care with medical management and care [24,30,43-45], Hospital-Based Palliative Care [4,46] and palliative care concurrent with life-prolonging treatment [47]. The literature demonstrates that palliative care has implications for patients, their families and medical institutions.
Palliative care has improved quality of life of patients and their families in several ways. It has decreased symptom distress [30,32,46,48], inhospital death rates [39,48], and negative moods [47]. It has improved well-being of patients and families [49], human dignity [50] and bereavement outcomes [51]. It has enhanced quality of treatment and care by decreasing patients’ hospital admissions [19,39] and in patient stays [4,39,48]. It has also increased opportunities for care and cure [19,30,46], decision making [30,46], satisfaction with care and treatment [46,48], explication of care and treatment goals [19,30] and coping ability of families [51]. In addition, palliative care can help to reduce expenditure of both patients and medical institutions [48,52,53]. Table 1 summarizes the consequences of palliative care for patients, families and medical institutions.
| Patients | Families | Medical institutions |
|---|---|---|
| Quality of life: ↓ pain and distressing symptoms ↑ well-being ↓ depressed moods ↓ anxiety and suffering ↑ relationships with self, others, and religious icons ↑ human dignity ↑ quality of life Treatment and care ↓ hospital admissions ↓ inpatient stays ↓ inhospital death rates ↑ opportunity for care and cure ↑ decision-making ↑ clarify goals of care ↑ satisfaction with care Finance: ↓ costs |
Quality of life: ↑ well-being ↓ psychological distress ↓ feelings of guilt ↑ bereavement outcomes Treatment and care: ↑ satisfaction with care ↑ improved coping ↑ decision-making |
Treatment and care: ↑ the quality of care ↑ care coordination ↑ clarify treatment goals Finance: ↓ hospital cost |
Table 1: Consequences of palliative care.
Related concepts
There has been a lack of definitional clarity related to palliative care, end-of-life care, and hospice care; too often they are frequently used interchangeably. This concept confusion may be a barrier to the development of palliative care. For instance, using palliative care synonymously with end-of-life care or terminal care has created the confusion that the concept of palliative care is valid only at the endof- life [10]. Referrals to palliative care continue to occur late in the trajectory of illness. It was hypothesized that the perceived association between the name palliative care and hospice was a barrier to early patients’ referral [54].
Hospice is a level of care that is reimbursed by Medicare with the definition of “care designed to give supportive care to people in the final phase of a terminal illness and focus on comfort and quality of life, rather than cure” [55]. It was created to provide compassionate and cost-effective care for patients and families facing a terminal illness [56]. The differences between palliative care and hospice care are summarized in Table 2.
| Palliative care | Hospice care |
| A more general term and is applicable to patients who have a significant burden of illness but are earlier in the disease trajectory. | Subset of palliative care in the end-of-life setting. |
| Admit and serve patients who are receiving either curative or non-curative therapies. | Patients who receive hospice care no longer accept any curative treatments. |
| No specific prognostic requirement for patients referred to a palliative care. | Requires acknowledgment and acceptance of the inevitability of death. |
| Can be provided in all health care delivery system settings, such as hospital, emergency department, nursing home, home care, outpatient service. | Includes primarily routine home care, general inpatient care, and respite care. |
| The goal of palliative care is to relieve suffering and to maximize the patient's dignity and quality of life and death. | Aims to improve the quality of death and dying process. |
Table 2: Differences between palliative care and hospice care.
Discussion
The limitations of this study predominately relate to the narrow scope of the literature. Identified articles in this paper were limited to the United States; no articles about palliative care in other countries were included, so the notion of palliative care in other countries cannot be drawn from this paper. Due to the huge range of differences in palliative care between the United States and other countries, this paper could not show these differences.
This paper provides an updated, comprehensive understanding of the concept of palliative care in the United States. The authors synthesized the definition of palliative care as follows: palliative care is a kind of care that addresses the multifaceted needs of patients, providing thorough symptom management and relief of physical and psychological suffering, meeting family caregiver needs, and providing clear communication among patients, families, and interdisciplinary palliative care team workers; it should be a significant part of disease management, especially for life-threatening illness; it can be provided in concert with curative treatment and should be initiated as early as possible in order to achieve the goals of good living, good dying and good death.
Compared with Meghani’s concept analysis paper [10], this paper provides an updated definition, broader and more up-to-date antecedents and attributes, and more detailed consequences of palliative care. The authors adopted the General System Theory (GST) [57] to display antecedents, attributes and consequences of palliative care in this paper (Figure 1). The antecedents, attributes and consequences are separately regarded as input, throughput and output in the general system theory (GST).
In addition, the authors developed a model of palliative care in illness trajectory (Figure 2) based on the synthesized definition and the integrated model of care proposed by the World Health Organization (WHO) [58]. From this model we can see that: (1) palliative care is patient- and family-centered through the whole trajectory of patients’ illnesses. After patients’ deaths, bereavement care is continually provided for families; (2) curative care and palliative care can occur simultaneously from the onset of a patients’ diagnosis, and palliative care may be the focused care for some patients at the time of diagnosis; and (3) hospice care is a part of palliative care, which is provided for patients who have a 6-month terminal prognosis certified by two physicians.
Conclusions
There has been a significant evolution in the understanding of the concept of palliative care in the 21st century. This paper provides the most updated meaning of palliative care in the United States. In fact, palliative care has evolved across the globe in different contexts and in different ways. Differences include, length of stay in palliative care, models of services, terminology and treatments used, public and professional perceptions, legal framework for euthanasia, funding mechanisms, and so on [59]. We need evidence on the most effective ways to provide palliative care, and there is much that the US and other countries could learn from each other to understand better what constitutes quality palliative care.
To develop palliative care as a medical specialty, we urgently need to consolidate infrastructure such as outpatient clinics and PCUs, increase training of palliative care professionals and oncologists, conduct research on novel integration models and quality improvement measures, educate patients and their families, and advocate for public health policy changes. We need comprehensive and rigorous research to evaluate the effects of well-delineated and generalizable palliative care structures and processes on important clinical and utilization outcomes to guide the further development of the field [39]. Oncologists, palliative care specialists, executives, educators, researchers, and political leaders need to work closely together to ensure access to high quality palliative care for all patients with life-threatening illness in the United States.
Acknowledgements
This paper was partially supported by the Hluchyj Doctoral Fellowship, we would like to thank Mr. and Mrs. Hluchyj for their support; we would also like to thank Peter Blood, Clinical Assistant Professor in the School of Nursing, University of Massachusetts Amherst for his edit of an earlier draft of this manuscript.
References
- Kapo J, Morrison LJ, Liao S (2007) Palliative care for the older adult. J Palliat Med 10: 185-209.
- http://www.capc.org/news-and-events/releases/news-release-4-14-08
- Casarett DJ, Hirschman KB, Coffey JF, Pierre L (2002) Does a palliative care clinic have a role in improving end-of-life care? Results of a pilot program. J Palliat Med 5: 387-396.
- Morrison RS, Penrod JD, Cassel JB, Caust-Ellenbogen M, Litke A, et al. (2008) Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med 168: 1783-1790.
- Ferrell BR, Borneman T (2002) Community implementation of home care palliative care education. Cancer Pract 10: 20-27.
- Davis MP, Walsh D, LeGrand SB, Lagman R (2002) End-of-Life care: the death of palliative medicine? J Palliat Med 5: 813-814.
- Grant M, Elk R, Ferrell B, Morrison RS, von Gunten CF (2009) Current status of palliative care--clinical implementation, education, and research. CA Cancer J Clin 59: 327-335.
- American Academy of Hospice and Palliative Medicine, Center to Advance Palliative Care, Hospice and Palliative Nurses Association, Last Acts Partnership, National Hospice and Palliative Care Organization (2004) National Consensus Project for Quality Palliative Care: Clinical Practice Guidelines for quality palliative care, executive summary. J Palliat Med 7: 611-627.
- Morrison RS, Dietrich J, Meier DE (2008) For the Center to Advance Palliative Care and the National Palliative Care Research Center. America’s Care of Serious Illness: A State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals. New York, NY: Center to Advance Palliative Care.
- Meghani SH (2004) A concept analysis of palliative care in the United States. J Adv Nurs 46: 152-161.
- Rodgers BL (2000) Concept analysis: an evolutionary view. In: Rodgers BL, Knafl KA. Concept Development in Nursing (2ndedn), PA: Saunders, Philadelphia, USA.
- Pickett M, Cooley ME, Gordon DB (1998) Palliative care: past, present, and future perspectives. Semin Oncol Nurs 14: 86-94.
- Rodgers BL (1989) Concepts, analysis and the development of nursing knowledge: the evolutionary cycle. J Adv Nurs 14: 330-335.
- Rodgers BL (1989) Exploring health policy as a concept. West J Nurs Res 11: 694-702.
- [No authors listed] (1992) Clinicians' quick reference guide to acute pain management in infants, children, and adolescents: operative and medical procedures. Pain Management Guideline Panel. Agency for Health Care Policy and Research, US Department of Health and Human Services. J Pain Symptom Manage 7: 229-242.
- Garrard J (2010) Health sciences literature made easy: The matrix method. (3rdedn), Boston: Jones & Bartlett.
- http://www.who.int/hiv/topics/palliative/PalliativeCare/en/
- http://www.abms.org/who_we_help/physicians/specialties.aspx
- Twaddle ML, Maxwell TL, Cassel JB, Liao S, Coyne PJ, et al. (2007) Palliative care benchmarks from academic medical centers. J Palliat Med 10: 86-98.
- Carlson MD, Morrison RS, Bradley EH (2008) Improving access to hospice care: informing the debate. J Palliat Med 11: 438-443.
- Adelstein W, Burton S (1998) Palliative care in the acute hospital setting. J Neurosci Nurs 30: 200-204.
- Abrahm JL, Hansen-Flaschen J (2002) Hospice care for patients with advanced lung disease. Chest 121: 220-229.
- Albert NM, Davis M, Young J (2002) Improving the care of patients dying of heart failure. Cleve Clin J Med 69: 321-328.
- Markowitz AJ, Rabow MW (2004) Palliative care for patients with heart failure. JAMA 292: 1744-1744.
- Macleod AD (2000) Ondansetron in multiple sclerosis. J Pain Symptom Manage 20: 388-391.
- Boyd CO, Vernon GM (1998) Primary care of the older adult with end-stage Alzheimer's disease. Nurse Pract 23: 63-66, 74-6, 79-80 passim.
- Muir JC, Arnold RM (2001) Palliative care and the hospitalist: an opportunity for cross-fertilization. Am J Med 111: 10S-14S.
- Duncan J, Spengler E, Wolfe J (2007) Providing pediatric palliative care: PACT in action. MCN Am J Matern Child Nurs 32: 279-287.
- Clark C, Seymour J (1999) Facing Death: Reflections on Palliative Care. Open University Press, Philadelphia.
- Sanft TB, Von Roenn JH (2009) Palliative care across the continuum of cancer care. J Natl Compr Canc Netw 7: 481-487.
- Teno JM, Connor SR (2009) Referring a patient and family to high-quality palliative care at the close of life: “We met a new personality... with this level of compassion and empathy”. JAMA 301: 651-659.
- Wiebe LA, Von Roenn JH (2010) Working with a palliative care team. Cancer J 16: 488-492.
- Von Gunten C, Ferris F, Portenoy R, Glajchen M (2001) CAPC Manual: How to establish a palliative care program. Center for Palliative Studies, San Diego Hospice and The Department of Pain Medicine and Palliative Care, Beth Israel Medical Center, New York.
- Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, et al. (2004) Family perspectives on end-of-life care at the last place of care. JAMA 291: 88-93.
- Chopra A; Centre for Aging, New Jersy School of Osteopathic Medicine (2001) Communicating effectively at the end of life. J Am Osteopath Assoc 101: 594-598.
- Emanuel L, Alexander C, Arnold RM, Bernstein R, Dart R, et al. (2004) Integrating palliative care into disease management guidelines. J Palliat Med 7: 774-783.
- http://apps.who.int/gb/ebwha/pdf_files/WHA58/WHA58_22-en.pdf
- Bruera E, Neumann CM, Gagnon B, Brenneis C, Quan H, et al. (2000) The impact of a regional palliative care program on the cost of palliative care delivery. J Palliat Med 3: 181-186.
- Morrison RS (2005) Palliative care outcomes research: the next steps. J Palliat Med 8: 13-16.
- Fromme EK, Bascom PB, Smith MD, Tolle SW, Hanson L, et al. (2006) Survival, mortality, and location of death for patients seen by a hospital-based palliative care team. J Palliat Med 9: 903-911.
- Penrod JD, Deb P, Luhrs C, Dellenbaugh C, Zhu CW, et al. (2006) Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. Journal of Palliative Medicine 9: 855-860.
- Connor SR (2009) U.S. hospice benefits. J Pain Symptom Manage 38: 105-109.
- Higginson IJ, Finlay IG, Goodwin DM, Hood K, Edwards AG, et al. (2003) Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? J Pain Symptom Manage 25: 150-168.
- Meyers FJ, Linder J, Beckett L, Christensen S, Blais J, et al. (2004) Simultaneous care: a model approach to the perceived conflict between investigational therapy and palliative care. J Pain Symptom Manage 28: 548-556.
- Wright AA, Zhang B, Ray A, Mark JW, Trice E, et al. (2008) Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 300: 1665-1673.
- Kuebler KK, Lynn J, Von Rohen J (2005) Perspectives in palliative care. Semin Oncol Nurs 21: 2-10.
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, et al. (2009) Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 302: 741-749.
- Morrison RS, Maroney-Galin C, Kralovec PD, Meier DE (2005) The growth of palliative care programs in United States hospitals. J Palliat Med 8: 1127-1134.
- Meier DE, Thar W, Jordan A, Goldhirsch SL, Siu A, et al. (2004) Integrating case management and palliative care. J Palliat Med 7: 119-134.
- Krisman-Scott MA (2001) The room at the end of the hall: Care of the dying, 1945--1976. Ph.D. United States -- Pennsylvania: University of Pennsylvania.
- Lynn J (2001) Serving patients who may die soon and their families: the role of hospice and other services. JAMA 285: 925-932.
- Smith TJ, Coyne P, Cassel B, Penberthy L, Hopson A, et al. (2003) A high-volume specialist palliative care unit and team may reduce in-hospital end-of-life care costs. J Palliat Med 6: 699-705.
- Elsayem A, Swint K, Fisch MJ, Palmer JL, Reddy S, et al. (2004) Palliative care inpatient service in a comprehensive cancer center: clinical and financial outcomes. J Clin Oncol 22: 2008-2014.
- Fadul N, Elsayem A, Palmer JL, Del Fabbro E, Swint K, et al. (2009) Supportive versus palliative care: what's in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer 115: 2013-2021.
- http://www.medterms.com/script/main/art.asp?articlekey=24267
- Feeg VD, Elebiary H (2005) Exploratory study on end-of-life issues: barriers to palliative care and advance directives. Am J Hosp Palliat Care 22: 119-124.
- Von Bertalanffy L (1969) General system theory: foundation, development, and applications (Revisededn) George Braziller, Inc.
- [No authors listed] (1990) Cancer pain relief and palliative care. Report of a WHO Expert Committee. World Health Organ Tech Rep Ser 804: 1-75.
- Higginson IJ (2005) End-of-life care: lessons from other nations. J Palliat Med 8 Suppl 1: S161-173.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 14984
- [From(publication date):
November-2012 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9883
- PDF downloads : 5101