Research Article Open Access
An Evaluation of the Current State of Cancer-Related Palliative and Supportive Care Research in the UK
Alex Molassiotis1* and Chris Jacobs21Alex Molassiotis, Professor of Cancer & Supportive Care; School of Nursing, Midwifery & Social Work, University of Manchester, Manchester, UK
2Chris Jacobs, Medical Student, School of Medicine, University of Manchester, Manchester, UK
- *Corresponding Author:
- Alexander Molassiotis
RN, PhD, Professor of Cancer & Supportive Care
University of Manchester, School of Nursing
Midwifery & Social Work, University Place
Manchester M13 9PL, UK
Tel: +44 (0)161-3067830
Fax: +44 (0)161-3067894
E-mail: alex.molassiotis@manchester.ac.uk
Received date: April 11, 2012; Accepted date: May 22, 2012; Published date: May 24, 2012
Citation: Molassiotis A, Jacobs C (2012) An Evaluation of the Current State of Cancer-Related Palliative and Supportive Care Research in the UK. J Palliative Care Med 2:112. doi:10.4172/2165-7386.1000112
Copyright: © 2012 Molassiotis A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
The aim of this study was to establish the current state of the research environment in the UK in relation to cancer supportive and palliative care. Three approaches were used to evaluate the current research environment in supportive and palliative care. A) A bibliometric analysiswas conducted on published research output between 2005 and 2010. B) An analysis of the UKCRN portfolio of trials was undertaken to establish the current research environment. C) A questionnaire survey was distributed to research groups in the field with the purpose of mapping the workforce, exploring funding/funding sources and gauging opinions about challenges in supportive and palliative care research. 586 papers met inclusion criteria for the bibliometric analysis, 76 studies were included in the UKCRN portfolio analysis and 36 questionnaires (overall response rate 74.5%) were received from UK research groups. An expansion in research activity is reflected by an increased trend in research output (57% over 5 years) and an increased proportion of studies registered with the NCRN portfolio of trials. Study designs were dominated by observational methods, however, a trend towards increased interventional methods was identified. In the workforce, an aging researcher population was identified and an increased tendency to work in few but large research groups was evident. Group opinions included increased collaboration in the field over the past 5 years, however, the withdrawal of a major funding partner from the field is currently a major challenge for the majority.
Introduction
While there have been large amounts of research resources focusing on new treatments for cancer, there has been relatively little looking at supporting patients during their illness and improving their quality of life - just 4.3% of the UK's National Cancer Research Institute (NCRI) funding budget was spent on palliative and supportive care in 2002 [1]. Workforce mapping research done for the NCRI strategic planning group [2] shows a clear focus on service delivery, organization, psychological research and measuring outcomes in terms of quality of life. This may have a lot to do with national strategies and targets surrounding improving service provision. The National Institute for Health and Clinical Excellence (NICE) guidance in 2004 [2] identified symptom management and complementary therapies of particular importance for future research, having been neglected in the past. This includes areas such as pain management, controlling nausea and vomiting and psychological symptoms.
One of the major problems identified by the NCRI [1] was one of organization and collaborative working. The workforce analysis revealed fragmentation across multiple sites, with often small groups of researchers working independently and with little interdisciplinary communication. The analysis also revealed inadequate numbers of senior researchers, thought to be due to a lack of funding at postdoctoral level. Few research groups had access to dedicated statisticians and methodologists, which makes using more complicated research methods and improving the quality of research difficult. Another issue identified was one of funding, where it was thought that health services research, and palliative care in particular, was not adequately funded.
In response to these problems, the NCRI strategic planning group published a number of recommendations to improve the research environment. These included trying to create a more collaborative research environment by forming 'clinical study groups' in areas such as palliative care and psychosocial oncology, funding for more formal research collaboratives, funding partners being encouraged to fund more posts for post-doctoral researchers, statisticians and methodologists, and availability of targeted funding for supportive and palliative care. Furthermore, following on from extensive research on service models carried out around the world, NICE commissioned the production of guidance in 2004 on improving service provision in the UK [2].
Since 2004, there is evidence that some of the recommendations made have been acted upon, but there is little data on their effect. Two supportive and palliative care research collaboratives were setup by the NCRI partners in 2006, and initially were awarded £3.8 million over 5 years [3]. These included the CECo collaborative [4] linking groups in Southampton, Manchester, Liverpool, Lancaster and Nottingham, and the COMPASS collaborative [5] linking groups in London, Edinburgh and Leeds. A one-off 'Capacity Building Grant Scheme' was also setup in 2006 worth just under £1M to complement the collaboratives and to provide more collaborative opportunities for clinical researchers working in other groups [6]. In addition in 2007/8, there was an influx of funding totaling £2.5 million for supportive and palliative care research specifically for lung cancer [3], and more recently in 2010 the Health Technology Assessment funding arm of the NIHR has had a funding call specifically for supportive and palliative care research.
Aims
The aim of the current study is to investigate how the cancerrelated field has changed since the NCRI supportive and palliative care (SUPAC) strategic planning group analysis in 2004. The specific objectives of the study were:
a. To measure the published research output in the field over the past 5 years. By doing this we will look to establish trends in output over time, make an assessment of the quality of the output and also look into the type of research being undertaken.
b. To ascertain the current research being undertaken in the field. We will look at the unpublished trials registered with the NCRN portfolio currently taking place to help establish the current research environment. This includes measuring the quantity, location and type of research being undertaken, as well as looking at the funding bodies currently involved.
c. To survey the current workforce to gain an indication of the makeup of the research groups active in the area. This includes information on the demographics of researchers, supporting institutions and the amounts and sources of funding. We will also look to subjectively examine how researchers feel the field has changed over the past 5 years, and also the main challenges currently experienced.
Methods
Assessment of publication output (2005 - 2010)
A bibliometric analysis was conducted on the literature published over the past 5 years from June 2005 to May 2010. Publications were retrieved through the Pubmed database using specific search terms thought to comprehensively cover topics in the field. The specific keywords used were 'Palliative care', 'Supportive care', 'End of life care', 'Symptom management', 'information', 'communication', 'complementary', 'quality of life', 'bereavement', 'professional issues', 'patient experiences', 'service delivery' and 'psychosocial'. Additional terms 'UK' and 'cancer' were applied to improve the sensitivity of the search, and a five year date limit applied.
The title of each study was manually assessed against specific inclusion criteria, including the topics described earlier, being cancerspecific and being UK-based research. It was decided to exclude interventional palliative chemotherapy and surgical trials, as it was thought that such trials tend to be relevant to specific diagnostic fields rather than palliative and supportive care directly, and conducted by teams outside of the field. With the intention of analyzing original research output, we also excluded review articles, case studies, opinion pieces, editorials and letters returned in the PubMed results. Two exceptions to this were systematic reviews and meta-analyses which were thought to be of higher quality and contribute significantly to the body of knowledge and were therefore included.
Each title was manually assessed for inclusion and then reviewed by a senior researcher and a decision made. A list was then compiled of included studies and the abstracts reviewed in full, those that still met the inclusion criteria were formally entered into the study and assessment variables collected before being added to a data sheet. Data retrieved included information on the year of publication, the journal of publication, the study design, the geographic location of the research group, the area of supportive and palliative care most relevant to the study and whether there was a diagnostic focus. An assessment of the quality of publications was made based on the Impact Factor (IF) assigned to the journal of publication, regarded as an indirect reflection on a journal's importance within its field. The latest Impact factors (for 2009) were retrieved for all journals included that were listed on the ISI Web of Knowledge index.
Assessment of current research
Data on current registered research was obtained from the UK Clinical Research Network (UKCRN) portfolio database, where all ongoing trials funded by UK Clinical Research Collaboration (UKCRC) partners are required to be registered. This was thought to be the most comprehensive database in the UK, acknowledging however that some studies funded from outside the NCRN partners would not be registered. Although no attempt was made to account for trials outside the NCRN partners, these funding are deemed to be small as all the major cancer funders in the UK are NCRN partners. The site was accessed on a single day and a list of studies categorized as 'Palliative Care', 'Psychosocial', and 'Complementary Therapies' within the 'Cancer' section of the portfolio was assessed for inclusion against the inclusion criteria mentioned earlier. Each title was manually assessed for inclusion and then reviewed by a senior researcher and a decision made. Those that met the inclusion criteria were entered onto a data sheet and information regarding the research group, study design, area of palliative and supportive care most relevant to the study, diagnostic focus, sample size and funding body was collected.
Workforce mapping
A questionnaire survey was designed to send to research groups in the field. Groups were identified via those studies included in the UKCRN portfolio, as well as personal knowledge of contacts in the field and identification of a supportive and/or palliative care research group from all UK universities through the web and the 2008 Research Assessment Exercise in the UK. Questions included details on the group and geographical location, number of researchers together with a more detailed breakdown of each researcher's demographics, total funding and funding sources, and two open questions asking 'How do you feel the field of palliative and supportive care research has changed over the past 5 years? In what ways has it changed?' and 'What are the particular challenges you are facing in the field of palliative and supportive care research at the current time?'
Respondents were given a total of 6 weeks to reply, during which time two reminder emails were sent. Replies were recorded and completed questionnaire data was entered onto a datasheet. Negative replies from those no longer conducting research in the field or unable to complete the questionnaire were anticipated and recorded separately.
Data analysis
Data was entered onto Microsoft Excel spreadsheets and tabulated, and descriptive analysis was carried out. Content analysis was used to analyse the results of the open questions, establishing common trends in responses and tabulating accordingly.
Results
Assessment of publication output (June 2005 - May 2010)
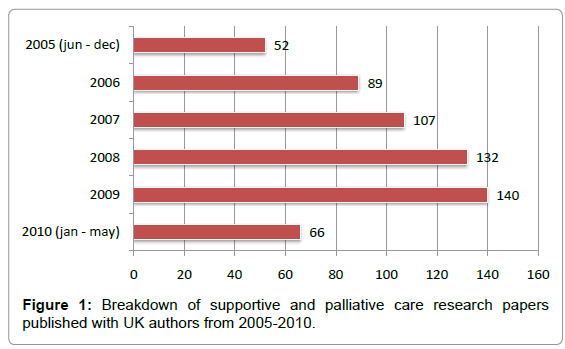
PubMed was searched and the literature retrieved at the end of May 2010. The initial search identified 3737 publications whose titles were subsequently reviewed. Out of these 664 publications were identified for further review. Upon review of the abstracts a further 78 studies were excluded (23 being conducted outside of the UK, 14 having no abstract for review and 44 not meeting the study inclusion criteria, many being review articles and case studies). A total of 586 papers were therefore included in the analysis. This translated into a mean of 117 publications per year, however, the breakdown of publications over time (Figure 1) shows a clear upward trend in research output, rising from 89 in 2006 to 140 in 2009.
Papers were published in 158 journals over a wide range of disciplines. The most popular journals included the European Journal of Cancer Care (46 studies), Supportive Care in Cancer (38), European Journal of Oncology Nursing (37), Palliative Medicine (33) and Psycho-Oncology (29). Impact factors were available and assigned for 508 (86.7%) of the papers. Out of those papers assigned impact factors, 34.8% (177) had an impact factor of less than two, 59.8% (304) had an impact factor of between two and ten, and 5.1% (26) were published in journals with an impact factor over 10. The mean impact factor was 3.24. Of note, 13 papers were published in the Journal of Clinical Oncology (IF 17.8), 9 in the British Medical Journal (IF 13.66) and 2 in the Lancet (IF 30.76).
The study designs were dominated by qualitative methods (169 papers, 29%) and descriptive quantitative (largely cross sectional) methods (164, 29%). There was a clear observational focus, with just 40 randomized controlled trials being conducted over the timeframe (7%). Other designs included mixed methods (7%), systematic reviews (13%), feasibility/pilot studies (5%), case series (4%), case control studies (3%), longitudinal studies (2%) and clinical audits (1%). Geographical location was assigned to all but 10 of the studies analysed. There was a clear domination by groups based in London (London includes several institutions; 146 papers, 25.3%) and Manchester (54 papers, 9.4%), followed by Leeds, Liverpool, Bristol and Southampton, however a wide range of 79 locations from all over the country were recorded .
Each paper was assigned a category of supportive and palliative care that best described the focus of research (Table 1). Research into symptoms was the most popular, being the focus of 92 (15.7%) studies. Breaking this down (Table 3), research into pain, psychological symptoms such as depression and anxiety, and fatigue dominated. Other popular areas of research included Quality of Life (85 studies, 14.5%), patient experiences (60, 10.2%) and complementary therapies (50, 8.5%). Notable neglected areas included bereavement support (1 study), spiritual support (3 studies), primary care (4 studies), and specific areas of symptom research (i.e. nutrition, weight loss and symptoms in advanced disease). (Table 1)
| Theme | Number |
|---|---|
| Symptoms (including psychological symptoms): | 92 |
| Pain | 19 |
| Fatigue | 13 |
| Breathlessness | 10 |
| Psychological symptoms | 15 |
| Cachexia / anorexia | 9 |
| Nausea / vomiting | 7 |
| Menopausal symptoms | 6 |
| Sexual dysfunction | 4 |
| Dysphagia | 2 |
| Trismus | 2 |
| Insomnia | 2 |
| Cognitive impairment | 1 |
| Xerostomia | 1 |
| Other symptoms | 16 |
| Care sites / settings | 12 |
| Communication | 9 |
| Treatment Decision | 7 |
| Cultural Differences | 7 |
| Under-served groups | 7 |
| User Involvement | 6 |
| Self Management | 5 |
| Primary Care | 4 |
| Spiritual Support | 3 |
| Social Care Research | 2 |
| Bereavement Support | 1 |
| Professional Issues | 1 |
Table 1: Area of Palliative and Supportive care breakdown according to publications, 2005-2010.
| Rank | Institution | Researchers |
|---|---|---|
| 1 | Kings College London | 39 |
| 2 | Psychological Medicine Research Centre, Edinburgh | 33 |
| 3 | Psychological oncology research group, Leeds | 26 |
| 4 | Cancer, Palliative and End of Life Care research group, Southampton | 26 |
| 5 | SUPAC Research Group, Manchester | 23 |
| 6 | Marie Curie Palliative Care Research Unit, UCL | 23 |
| 7 | Sue Ryder Study Centre, Nottingham | 19 |
| 8 | Children’s palliative care research centre, Bangor | 16 |
| 9 | Middlesex University | 15 |
| 10 | International observatory on end of life care, Lancaster. | 10 |
Table 2: Group sizes according to the survey results.
| Funding body | Number of groups funded |
|---|---|
| Cancer Research UK | 11 |
| National Institute for Health Research | 9 |
| Dimbleby Cancer Care | 8 |
| Macmillan Cancer Support | 8 |
| NCRI | 7 |
| Department of Health | 5 |
| Big Lottery Fund | 4 |
| Marie Curie Cancer Care | 4 |
| Burdett Trust for Nursing | 3 |
| Other Charitable Grants | 3 |
Table 3: Top 10 funders according to the survey results.
With respect to diagnostic focus, 337 (58%) of the papers had no specific cancer diagnostic focus. Out of those studies that did focus on a cancer diagnostic group, the most popular was breast cancer, which 64 studies (10.9%) focused on exclusively. Head and neck cancer was the focus of 47 studies (8%), mostly published in their specialty journals. Common cancers encountered in palliative care, such as lung, prostate and colon cancer accounted for the next three most popular, with 27 (4.6%), 25 (4.3%) and 24 (4.1%) studies respectively.
Assessment of current NCRN portfolio research
The UKCRN portfolio was accessed at the end of May 2010 and suitable study details downloaded. There were 910 trials registered in the 'cancer' section of the database, of which 76 (8.4% of the cancer portfolio) met inclusion criteria. Trials at all stages were represented from those at the 5-year follow-up stage to those open to recruitment until 2012. The majority of studies were observational (40 studies, 58%), however there were 27 (36%) interventional trials registered. 8 (11%) studies reported using both interventional and observational methods. The most commonly used design was qualitative methods (19 studies, 25%), and together with cross sectional (15 studies, 20%) and longitudinal (7 studies, 10%) studies made up the majority of studies. There were 14 (19%) randomized controlled trials registered, together with 12 feasibility studies whose methods were either mixed or undocumented. A further 6 studies had undocumented design on the database.
Most trials (62%, 47 studies) had a sample size of over 100, and 18% (14) reported a sample of over 500 participants. The majority of studies did not have a diagnostic focus (51 studies, 68%). Breast cancer (12 studies, 16%) was the most common of those that did have a diagnostic focus, followed by head and neck (4 studies, 5%) and lung cancer (3 studies, 4%). The only other trials to report a focus were two on colorectal cancer, and one each on prostate cancer, oesophageal cancer and biliary tract malignancy.
Research into symptoms was the most common research theme, with 14 studies (18%) looking into a range of cancer related symptoms including pain (5 studies), breathlessness (3 studies), fatigue (3 studies), nausea/vomiting (2 studies), psychological symptoms (2 studies) and menopausal symptoms (1 study). Other popular themes were quality of life (12 studies, 16%), complementary therapies (9 studies, 12%) and patient experiences (9 studies, 12%). There were no studies looking at the use of technology and only one study looking at service delivery. The most popular geographic locations of studies were London (16 studies) and Leeds (15 studies) . With respect to primary funders, Cancer Research UK was by far the most dominant partner registered (31 studies, 41%). The next most common funders were Macmillan Cancer Support (5 studies), Dimbleby Cancer Care (3 studies), the NIHR Research for Patient Benefit fund (3 studies), the Medical Research Council (3 studies), NIHR Service Delivery and Organisation (2 studies), Breast Cancer Campaign (2 studies), Department of Health (2 studies), Cicely Saunders Foundation (2 studies), EORTC Quality of Life group (2 studies) and the NCRI Lung Cancer award scheme (2 studies).
Workforce mapping
71 potential research group leaders were identified and contacted. Hence, it is important to emphasize that the survey responses and findings presented below represent the opinions of the group leaders and are not necessarily representative of all researchers within each group. Responses were received from 53, leaving 18 that failed to respond, giving a response rate of 74.5%. 17 groups responded to say that they were not currently undertaking research in the field or felt unable to complete the questionnaire. 36 groups responded with specific data for their group. In total there were 112 academic posts held in the field. In addition to these, an additional 229 full-time equivalent posts were identified for research staff. In total the research workforce identified amounted to 341 posts. The mean group size was 9.5 researchers. The largest 10 groups are shown in Table 2. There were six groups in total with over 20 researchers. Three groups had between 10 and 20 researchers, leaving the significant proportion of groups with smaller numbers (10 groups with between 5 and 10 researchers, 16 with below 5). There were 2 questionnaires returned by researchers working independently.
Additional details were returned for 216 of the researchers (63%). The majority (151 researchers, 70%) worked full time in the field, the remainder working part time. A discipline was identified for 156 (72%) staff members. By far the most common discipline was nursing (81 staff, 52%), followed by medical (29, 19%) and psychology (23, 15%) disciplines. There were smaller numbers of administrators (5, 3%), sociologists (5, 3%), statisticians (4, 3%), health service researchers (4, 3%), physiotherapists (3, 2%) and dieticians (2, 1%). For those who were identified as medical, 9 were specialists in palliative medicine, 3 were primary care physicians, 2 were psychiatrists as well as a paediatrician, a surgeon and a specialist in rehabilitation medicine. It was not possible to identify a specialty in 12 people from the medical group.
Ages were submitted for 72 (33%) of the workforce, showing a large proportion of experienced/older researchers and a relatively small younger population. There were 13 members less than 40 years old, 9<30 years old, 19 being 40-50 years old and 19>50 years old. 22 (61%) of staff were based in a University. Ten groups were based in a university teaching hospital, and 2 in specialist cancer centres. There was one group from a hospice.
Total funding received for all groups over the past 5 years was £ 59,944,306. This averages £ 11,988,861 per year. The most common funder was Cancer Research UK, with 11 groups stating they received funding from them over the past 5 years. This was followed by the National Institute for Health Research (9 groups), Dimbleby Cancer Care (8 groups) and Macmillan Cancer Support (8 groups). The top 10 funders are shown in Table 3. Thirteen groups reported funding of over £ 1M in the past 5 years, with the most well funded places being King's College London, University of Manchester and University of Edinburgh (Table 4).
| Rank | Group Name | Location |
|---|---|---|
| 1 | Cicely Saunders Institute - Department of Palliative Care, Policy and Rehabilitation – Kings College London | London |
| 2 | SUPAC Research Group, University of Manchester | Manchester |
| 3 | Psychological Medicine Research - Edinburgh Cancer Research Centre/University of Edinburgh | Edinburgh |
| 4 | Academic Palliative and Supportive Care Studies Group- University of Liverpool | Liverpool |
| 5 | International Observatory on End of Life Care, Lancaster University | Lancaster |
| 6 | The Sue Ryder Care Centre for the Study of Supportive, Palliative and End of Life care: University of Nottingham | Nottingham |
| 7 | Cancer, Palliative and End of Life Care - University of Southampton | Southampton |
| 8 | Psychosocial Oncology and Clinical Practice Research Group, University of Leeds | Leeds |
| 9 | CRUK Psychosocial oncology group, University of Sussex | Brighton |
| 10 | Supportive Cancer Care Research (S-CARE) group, Kings College London | London |
| 11 | SuPac: Nottingham University Hospital | Nottingham |
| 12 | Cancer and Supportive Care Research - University of Surrey | Guildford |
| 13 | St George's Palliative Medicine Research Group, St George’s University | London |
Table 4: Groups with research funding of over £1M in supportive and palliative care over the past 5 years.
Content analysis on the open questions revealed some common trends in past changes and current challenges (Table 5). Key responses when asked how the field has changed over the past 5 years included more collaborative working after the formation of the two Collaboratives (although two respondents mentioned that this has been divisive for those not included), more active researchers in the field (although mostly contained within a small number of academic groupings), and higher recognition of palliative care research. When asked about current challenges facing the researchers, responses were dominated by funding concerns. This was represented by two-thirds of the respondents. The vast majority mentioned the reallocation of Cancer Research UK funding away from the field, and several stated there is less money available from other charities which is affecting the sustainability of research. While securing funding was a major challenge reported by most responders other challenges mentioned included increasing quality and methodological expertise, retaining staff, concerns over sustainable collaborative working and the lack of a career structure.
| How the field has changed over the past 5 years? | What are the current challenges facing the field? |
|---|---|
|
|
Table 5: Responses to the Open Questions.
Discussion
While we comprehensively searched the literature, it is likely that some studies were not captured by our search terms. This may be because unusual keywords were applied to the studies, or the limit terms 'cancer' and 'UK' were not included. It is also likely that there are current studies not included in the UKCRN portfolio because they are not receiving funding from NCRN funding partners. Also, increasingly palliative care/end of life care is broader than cancer, which will underrepresent research effort and publications in this study that uses a more narrow focus into cancer. Hence, this report comes from the 'lens' of biomedicine and health services research and may under-represent the contribution of social science in the field; this may account for some of our findings. Furthermore, while we tried to closely replicate the methods used by the NCRI in their strategic analysis report in 2004,we were unable to follow them completely and as such much of our data is not directly comparable. Comparisons have been made to try and establish trends however complete accuracy cannot be guaranteed and should be interpreted with caution. The use of Potential Impact Categories in the NCRI report rather than traditional impact factor analysis used in this paper also makes direct comparisons difficult. It is also likely that data returned from groups for the workforce mapping also contained data from palliative and supportive care research not restricted to oncology. Nevertheless, the similarities between the analysis of publication output and current research registered in the NCRN portfolio of studies enhance the validity of the data.
Despite these limitations, the data suggests that there is a clear improvement in the supportive and palliative care research over the past five years although the fragile nature of funding in the field is of major concern for the sustainability of such improvements. Key NCRI targets from 2004 have been improving, although more work is clearly needed and gaps are still evident.
Assessment of publication output
While a limitation of this part of the study is that only one search engine was used for the literature search, it is clear that there is an upward trend in publication output over the course of the study. The trend is quite significant, with 51 more papers being published in 2009 than in 2006, representing a 57% increase in output. Measuring the quality of research is challenging, however analyzing impact factors of journals and the design of studies can give some indirect indication. The most popular journals were those primarily concerned with supportive and palliative care in cancer (as search terms include the word 'cancer'). These journals however are quite of low profile and command only a modest impact factor. A much smaller number of outputs have achieved publication in more prestigious journals. While there is little comparative past data, a study by Clark et al. [7] assessed the place of supportive, palliative and end of life care in the Research Assessment Exercise of 2001 and 2008 in the UK and showed that output from 2001 to 2008 only slightly improved or remained stable.
There is a clear observational focus to the study designs included, with just 7% of the output being randomized controlled trials. Randomized controlled trials reflect research questions related to efficacy and effectiveness, and an increasing focus on such designs was a priority. This low number of trials is perhaps not surprising as much of palliative and supportive care has to do with providing service and care, and there is much less focus on interventions than in other areas of oncology perhaps as there may be formidable challenges and ethical issues in designing particularly end of life trials [8,9]. This is reflected in the high proportion of studies where qualitative methods are used (27%), often for data on patient experiences and perceptions, confirming past bibliometric analyses [9]. Many studies used standardized validated measures, which allows some degree of comparisons to be made, although the descriptive nature of the studies are less likely to influence significant changes in practice.
The data on geographic locations suggests that research is being carried out at a large number of institutions around the country and this was regarded as a problem in the NCRI 2002 review. A large proportion of studies are conducted in a relatively small number of centres, for example London and Manchester. The domination of seven 'high intensity' research institutes in the country has also been shown elsewhere [7]. There was some evidence to suggest that London (all research groups assessed) is becoming less dominant however, with its output proportion falling from 34% in 2004, to 25.3% in this analysis.
Research into symptoms was flagged as an area for focus in the NICE systematic review, and our analysis shows it to be the most popular area for studies conducted. There were a large number of interventional studies looking at relieving symptoms and most of the randomized controlled trials were conducted in this area. This is reassuring as it represents a move towards looking at interventions and treatments, however focusing more work on neglected symptoms such as nutritional symptoms, weight loss and symptoms of advanced disease, is required. This was followed by research looking into quality of life, mainly using quality of life questionnaires to look into both the impact of cancer and cancer treatments on quality of life. Research into patient experiences and complementary therapies was also common, which were also flagged as an area for focus in the NCRI report. Several other areas that were identified for further research work however proved disappointing. There was just one study looking specifically at bereavement support and just three looking at spiritual support, although it is acknowledged this may be an artifact of our search strategy, as most of research into bereavement or spiritual support may not be linked to a disease (cancer). Other neglected areas include communication, which with 9 studies appears a little sparse considering its large scope and importance, and research into the role of primary care with just 4 studies. Clark et al. [7] have also highlighted that there was a clear shift from 2001 to 2008 in 'Clinical care: supportive care, palliative care and quality of life' which emerged as the second most common theme of research, while areas such as communication and needs assessment had <10 outputs. Furthermore, Bennett et al. [8] also highlight that neglected areas of research include ways to support psychological, social and spiritual components of care, and therapeutic approaches for the management of a range of challenging symptoms.
Most studies were not cancer-diagnosis specific and included patients with different/mixed cancers. This measure can be used to give an indication of tailored research within the field, and while we were not able to establish any changes since the 2004 analysis, it will be interesting to see how this figure changes in the future. Out of those with a diagnostic focus, breast cancer dominates as it did in 2004. It is widely recognized that research spending for specific cancers is often disproportionate to their mortality and burden [1] and this is reflected somewhat in our analysis, with breast cancer being the most popular focus of those studies which were site specific. More telling perhaps is the proportionately few studies focused on the common cancers encountered in palliative care, especially lung and GI cancers.
Overall, over the past 5 years it appears the research output has been encouraging. There is more research being produced and there is some evidence to suggest that there has been investment in terms of improving methodology and some neglected areas identified previously are being addressed. There are still some areas of concern where NCRI recommendations do not appear to have translated into research output. There is still a lack of research into bereavement, spiritual support and communication, which may need to be addressed in the near future. Stronger patient involvement in developing research questions and priority areas for research would be useful to set the agenda and the funders with the NCRI could take the lead to do so in a more formal and strategic way.
Assessment of current research
A limited amount of information can be gained from the proportion of studies in the UKCRN portfolio with a supportive and palliative care focus. In the NCRI strategic review in 2002, a review of the portfolio at the time found that 6% of research was on cancer control, survival and outcomes research. This encompassed a range of topics including palliative and supportive care, health surveillance and health care delivery. Our figure of 8.4% based on more stringent criteria compares favorably and certainly reflects an increased share of the portfolio proportionately. This data corroborates the increased trend in research output documented in the bibliometric analysis of past research output, and is encouraging as it suggests a more successful and expanding environment.
There is a much higher proportion of intervention trials, in particular randomized controlled trials, registered on the portfolio compared to that identified in the review of past research output (19% vs 7%). It is important to note however that this figure is likely to be offset due to the decreased relative likelihood of observational trials being included in the portfolio than interventional trials. Systematic reviews and smaller observational studies may be published having not appeared on the database, however it is unlikely to account for the 12% difference in results. It therefore seems likely that the proportion of randomized controlled trials has increased over the past few years. This is reassuring as it represents a move towards one of the goals of more interventional trials and better methodology. The diagnostic focus of studies reported on the portfolio is broadly similar to that reported in the five year publication analysis. Most trials were of substantive size, most having a sample size of over 100. This is reassuring as a high proportion of large scale trials increases data validity and quality.
An area that does seem to have added focus in the portfolio analysis is complementary therapies. The studies listed command a greater proportion than in the 5 year analysis (12% vs 8.5%) and certainly reflect an increased focus on the area. Research into methodology used is another area that appears to be showing an increasing trend (9.2% of the portfolio vs 3.2% over the last 5 years). Many of these studies relate to the validation of outcome measures. This is reassuring as methodology was a specific target area for improvement. Neglected areas identified in the five year analysis are also reflected in this analysis, with no research at all focused on spiritual and bereavement support, although, as stated earlier, researchers in these fields may not see their work through the 'lens' of a disease label (cancer). Interestingly, there is only one study registered looking at service delivery (1.3% vs 5.6% in the five year analysis), which is further evidence that the recommendation of shifting the research focus from looking at service delivery to interventions is being acted upon.
Charitable organisations make up the large majority of funding partners. While this is supplemented with a considerable amount of input from public organisations such the Department of Health, there is a need to find more sustainable funding which smaller charities cannot necessarily provide. The NCRI strategic analysis of 2002 revealed Cancer Research UK (CRUK) was the dominant funding partner at the time over the whole of the NCRI, and this is definitely still the case during the period of our assessment with respect to palliative and supportive care (although currently CRUK does not fund such research any longer). The announcement that CRUK is to remove their funding commitment for palliative and supportive care research [10] is therefore likely to have a large impact on funding available in the field, particularly as some 40% of the current funding were awarded from CRUK. It will be very difficult for other charities to make up the funding difference of 40% that CRUK's decision will create in the future, and this is an area that necessitates significant and coordinated action from other funders in the country. Funding directly to Universities does come from the Higher Education Funding Council for England (HEFCE) both in terms of academic positions and funding as a result of the national Research Assessment Exercise, but isolating the specific funding for any research group is almost impossible.
Overall, the current portfolio has been comprehensively analysed and some interesting trends in the current research environment identified. There appears to have been a concerted move towards implementing many of the recommendations made, with the proportional number of studies increasing, an increased focus on methodology and complementary therapies and a move towards more interventional research.
Workforce mapping
The level of response from the workforce survey was satisfactory, with all major groups responding. While there were non-responders, it is thought that these are likely to be mostly small groups working independently or not undertaking work in the field. This is reassuring as it gives the data, especially the workforce data, a high level of credibility. We were unable to dedicate the required time and resources to achieve the response rate of the NCRI workforce analysis in 2004, however much of their extra data appears to have been collected from smaller groups and individuals (indicated by questionnaires returned by single researchers, 2 in our analysis vs 10 in 2004). In our study the majority of non-respondents were individual researchers and this may be partly explained by the limited administrative resources in places with few dedicated researchers, being too busy or feeling this survey does not apply to them as they are temporarily in the field. The total research workforce of 341 posts is a borderline improvement on the 2004 figure of 330. This is almost certainly an underestimate as the 2004 analysis was more sensitive, and we would expect the true figure to be higher to account for the increased research output. The proportion of permanent academic contracts has remained similar (32.8% vs 33% in 2004).
There appears to have been a move towards working in larger research groups. In 2004 there were 3 groups identified with over 20 researchers, our analysis shows that 6 groups are now over this size, although this should be interpreted with caution, as the 2004 figures were Full Time Equivalents. Perhaps a more significant indicator is that 50% of the research workforce work within these 6 larger groups. Reasons for this may be the shift towards collaborative working leading to merging of groups and skills, or that funding is easier to attract being part of a larger group, leading to a tendency to work as part of a larger team. The significant investment from the relevant institutions in supportive and palliative care research infrastructure should also not be underestimated, although this may be threatened by reduction in university budgets in the future.
With respect to professions, the domination by nurses is clear and this was also the case in the 2004 analysis as well as the work by Payne & Turner [9] who stated that this is perhaps attributable to the growth of nursing scholarship in the past decade. Our results suggest a higher proportion of researchers that come from a nursing background to date (52% vs 36% in 2004) and may reflect a better career integration strategy for nursing. The proportion of medical staff is relatively similar (19% vs 21% in 2004), with a similar breakdown over the medical specialties. The age range of researchers suggests a skew towards the older range of the spectrum. The relatively few younger researchers may be a cause for concern as a significant proportion (26%) is due to retire over the next 10-15 years (assuming a retirement age of 65). This appears to have got much worse since the 2004 analysis, just 12% were aged over 50 in 2004 and only 31% of researchers are aged under 40 in our study, compared to 58% in 2004. While the proportion of researchers for which ages were reported was significantly lower in our study (33% vs 76% in 2004), it is still thought our cohort is a good representative sample. Reasons for this could be that there are still problems in gaining post-doctoral appointments, limited PhD opportunities, poor career structure and progression or supportive and palliative care not seen as a good option by young researchers due to limited funding. Future workforce analysis should look into this in more detail. A high proportion of groups are based at universities rather than in the clinical environment (in hospitals, primary care or hospices). This may be due to the emergence of palliative and supportive care as a dedicated research area in its own right, however the small number of studies taking place in hospices or the community may represent a large potential patient research population currently untapped.
The average funding per year for all respondents of approx £12 million does not reflect an improvement from the £11.4 million received in 2002, and represents a decrease in real terms. This however needs to be placed in context of severe UK and global financial market constraints from 2008 onwards that had a significant impact on the availability of funding for research. Using the UKCRN database we are confident our analysis includes data from the institutions receiving the vast majority of NCRI partner funding, however while our questionnaire clearly asked for figures over 5 years, some responses appear to reflect annual research income and as such this figure may be an underestimate. The recent CRUK withdrawal of funding in supportive and palliative care, accounting for over 40% of the funding may well account for the lack of an increase in the overall funding, despite other (often one-off) pump priming funding opportunities provided over the past few years. Hence, the higher focus in supportive and palliative care research has not necessarily translated in significant increases in funding over the past few years.
The proportion of groups receiving funding from CRUK is less than the proportion of studies registered on the UKCRN portfolio funded by CRUK (31% vs 41%), however this can be explained by the fact that CRUK have tended to fund a small number of larger research groups through CRUK units. The portfolio data is therefore a better representation of CRUK's domination of funding, however the workforce data suggests that it will be the largest groups that will be hit hardest by the reduction in CRUK funding. Also, the benefits of 'critical mass' might be under threat by the withdrawal of this major funder.
The responses to the open questions tend to suggest that the formation of the two research collaboratives have gone some way to increasing the amount of collaboration within the field. A few mentioned the increased challenges faced by not being part of a collaborative, which may go some way to explain the trend of working in larger groups. The fact that a number of respondents mentioned expansion of the workforce was limited to larger groups also suggests that investment has been more targeted at larger institutions. These responses are not surprising as this environment might be expected given the targeting of the extra funding. There was a general feeling that the research environment has improved over the last 5 years, with collaboration together with increased awareness of the field, better funding opportunities and increased user involvement mentioned.
Securing funding was by far the most common challenge mentioned and the change in direction of CRUK funding was the major trend mentioned by a large proportion of respondents. This will inevitably have a major impact on the field given the high percentage of total funding CRUK contributed to supportive and palliative care research. One of the main problems mentioned is the uncertainty around other possible funding sources, and the sustainability of funding for long term trials and the two national Collaboratives. In an area that has traditionally had difficulty attracting funding, it is likely this may have a large detrimental effect on research output and the workforce in the future and put at risk the achievements demonstrated over the last 5 years.
Overall, the measures put in place to improve the research environment appear to have had a positive impact on the field, although this may be negated by the CRUK withdrawal of funding in the field and the economic downturn effect on charities. Also, it is probably too early to expect any real impact of the supportive and palliative care initiative in essentially less than five years from its start, as the impact in most cases is indirect and long-term. The increased focus on collaborative working appears to have translated into an improvement in conditions and may go some way to explaining the improved research output. There is uncertainty over funding however as our data suggests there has been little or no extra overall investment in palliative and supportive care research since 2002, and this is likely to get worse given the uncertainty of future funding due to the reallocation of CRUK resources. This accords with Clark et al. [7] analysis of Research Assessment Exercise (RAE) returns.
This study gives a snapshot of the state of palliative and supportive care research in the UK in 2010. It is likely that with the current funding challenges and uncertainty, the makeup may change significantly over the short term, however the results have provided some evidence of mainly positive changes that have taken place. Clearly securing future funding is essential to sustain current and future projects and this should be the main short term concern of funders and research groups. Specific areas requiring further research are spiritual support, bereavement support, less common but complex symptoms, symptoms in advanced disease and communication. Further analysis on the ageing workforce and analysis of accurate data on funding would also be prudent. We also feel there is a need to focus on the impact of research on service delivery and patient outcomes, an area that has had little focus to date. There is no focus in assessing the impact of research in practice, and this should be a priority both within projects and from the funders. Funding for programmes of research in supportive and palliative care should address some of the concerns raised, but currently no team in the UK holds such funding. International funding were limited in our analysis, and a stronger focus should be directed both in attracting international funding and developing internationallylinked programmes of research. However, there is evidence of more development in gaining EU funding for international research specifically in palliative care (e.g. see the EAPC Research Network, http://www.eapcrn.org, for list of current grants).
Acknowledgements
We would like to thank Prof. Sheila Payne, Lancaster University and Prof. Chris Todd, University of Manchester for their invaluable comments in earlier drafts of the paper.
References
- National Cancer Research Institute (2002) Strategic Analysis: An overview of Cancer Research in the UK directly funded by the NCRI Partner Organisations.
- National Institute for Health and Clinical Excellence (2004) Supportive and Palliative care guidance.
- NCRI: Supportive and Palliative Care (SuPac) collaboratives.
- Cancer Experiences Collaborative (CECo).
- Compass Collaborative Homepage.
- Marie Curie Cancer Care: NCRI SuPaC Research Collaboratives.
- Clark D, Clark J, Greenwood A (2010) The place of supportive, palliative and end of life care research in the United Kingdom Research Assessment Exercise, 2001 and 2008. Palliat Med 24: 533-543.
- Bennett MI, Davies EA, Higginson IJ (2010) Delivering research in end-of-life care: problems, pitfalls and future priorities. Palliat Med 24: 456-461.
- Payne SA, Turner JM (2008) Research methodologies in palliative care: a bibliometric analysis. Palliat Med 22: 336-342.
- Cancer Research UK Research Focus News
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13964
- [From(publication date):
July-2012 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 9433
- PDF downloads : 4531