An Epithelioid Sarcoma of the Right Foot: Raising Awareness of a HighGrade Malignancy
Received: 30-Apr-2018 / Accepted Date: 14-May-2018 / Published Date: 21-May-2018 DOI: 10.4172/2161-0681.1000345
Abstract
An epithelioid sarcoma (ES) is an infrequent mesenchymal malignancy most commonly encountered in adolescents and young adults in the distal extremities. It has a proclivity for the flexor aspects of the hands and feet with male predilection observed at a ratio of 2:1. The indolent presentation, seemingly unremarkable histopathology, and low incidence of this disease can lead to misdiagnosis. We report a case of a twenty-year old female who presented to her primary care physician with chief complaint of a painful lump beneath her right second and third toes. The tumor was subsequently excised with diagnosis of epithelioid sarcoma.
Keywords: Epithelioid sarcoma; Foot; Malignancy; Tumor
Introduction
Soft tissue sarcoma is a rare neoplastic entity, comprising 1-2% of all malignancies. Currently, there are over 50 types of identified sarcomas. Among them, ES is an exceedingly rare type first described in 1961 by Polish pathologist J. Laskowski as “sarcoma aponeuroticum” [1,2]. This received little attention at the time and FM Enzinger would later coin the term “epithelioid sarcoma” in 1970 [3]. Enzinger went on to reclassify 148 previously misdiagnosed cases as ES. Misdiagnosis of an epithelioid sarcoma is a common topic in published literature spanning over the past four decades. Usually, cases of ES are erroneously diagnosed as inflammatory processes, skin ulcerations, necrotizing granulomata, and soft tissue tumors [2-7]. In this case, the patient received varying assessments of her disease process with apparently benign clinical and radiologic findings, but with a discordant pathological appearance of ES. There is an ongoing need for dissemination of the clinical and histological findings (or lack thereof) seen with ES. Continued vigilance for this somewhat esoteric but nevertheless high-grade malignancy can prevent misdiagnosis and improve quality of life outcomes for future patients.
Case Presentation
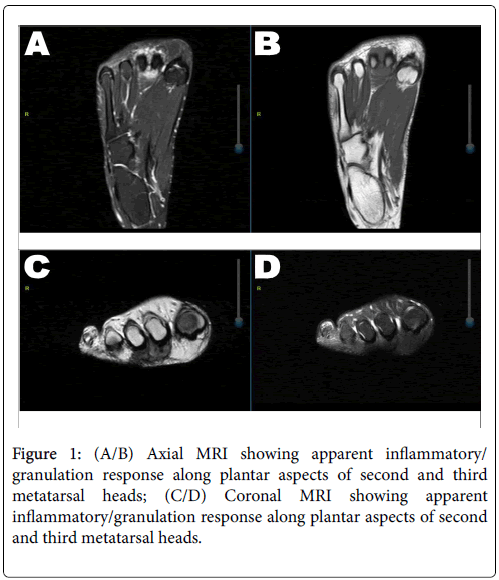
An otherwise healthy 20-year-old female initially presented to her primary care physician with a three-month history of a painful nodule on the plantar aspect of right foot between the 2nd and 3rd metatarsal heads. Apparently, this had been steadily growing from pea-sized to approximately the size of two quarters in this time period. The skin overlying the mass was described as white-tan without notable ulceration or signs of acute infection. MRI imaging was performed, which did identify the mass as likely prominent granulation tissue/ granulomata. Based on these results, a differential diagnosis of ganglion cyst, schwannoma, or neuroma was posited (Figure 1). The patient was referred to podiatry for further evaluation. Needle aspiration was attempted twice unsuccessfully. Subsequently, the decision was made to surgically excise the mass in a piecemeal fashion.
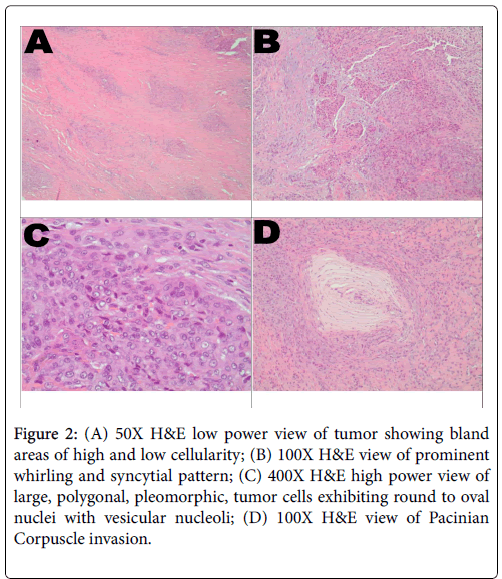
Gross examination revealed three fragments of soft tissue with variegated hue from white-tan to pink-tan. The largest fragment measured 3.5 cm × 3 cm × 1.3 cm. Microscopically, the lower power field delineated both low cellular and high cellular areas (Figure 2A). The low cellular areas comprised mainly of spindled cells punctuated with highly cellular islands. The cellular islands were comprised of more epithelioid appearing cells. These cells had a whirling and syncytial pattern (Figure 2B). The individual tumor cells were large, pleomorphic, and polygonal, harboring copious amounts of amphophilic cytoplasm. The cell borders were not well delineated by cell membranes. Nuclei were round to oval and primarily located concentrically with conspicuous vesicular nucleoli (Figures 2C and 2D). The mitotic rate was readily estimated at 12% and confirmed with Ki-67 stain. Invariably, the large tumor cell islands outgrew their blood supply and central necrosis was observable with speckled, dystrophic calcifications. There was also evidence of angiolymphatic and Pacinian corpuscle invasion, the latter of which being likely responsible for the patient’s pain. The surgical margins were positive for malignancy.
Figure 2: (A) 50X H&E low power view of tumor showing bland areas of high and low cellularity; (B) 100X H&E view of prominent whirling and syncytial pattern; (C) 400X H&E high power view of large, polygonal, pleomorphic, tumor cells exhibiting round to oval nuclei with vesicular nucleoli; (D) 100X H&E view of Pacinian Corpuscle invasion.
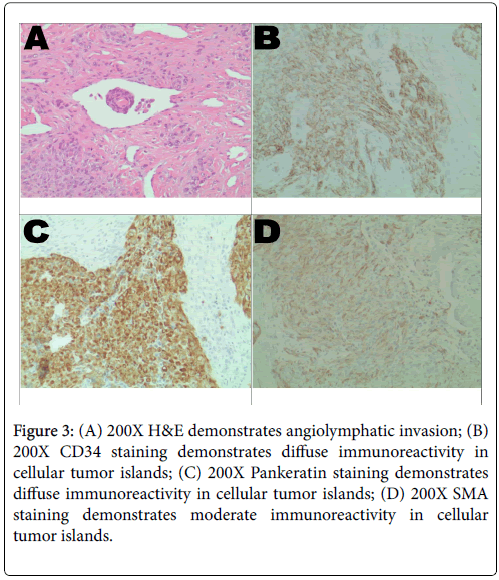
A limited armamentarium of immunohistochemistry was performed for confirmation. The positively staining antibodies for ES include CD34, SMA and AE1/AE3 (Figure 3A). The more cellular tumor islands stained diffusely with AE1/AE3 and CD34 (Figures 3B and 3C). The SMA delineated a moderate immunoreactivity (Figure 3D). The novel INI-1 (Tumor Suppressor Gene), which identifies normally nucleated cells but excludes ES and rhabdoid tumor cells, was not available in-house. INI-1 staining was performed at Cleveland Clinic (CCF) after referral for sarcoma treatment and was negative, essentially confirming the ES diagnosis.
Figure 3: (A) 200X H&E demonstrates angiolymphatic invasion; (B) 200X CD34 staining demonstrates diffuse immunoreactivity in cellular tumor islands; (C) 200X Pankeratin staining demonstrates diffuse immunoreactivity in cellular tumor islands; (D) 200X SMA staining demonstrates moderate immunoreactivity in cellular tumor islands.
The current gold standard treatment of ES is surgical resection of residual tumor utilizing wide margins [8]. Best outcomes are achieved at tertiary care centers where a multidisciplinary sarcoma team is present. The patient underwent preoperative chest X-ray and CT, which did not reveal presence of metastatic disease. Repeat MRI of the right foot showed extensive residual tumor and the patient subsequently underwent right groin sentinel lymph node biopsy, which was also negative for metastatic spread. Surgical treatment was comprised of right transmetatarsal amputation with anchoring of the tibialis anterior tendon and peroneus brevis tendon into deep soft tissue. The surgical margins extended 3 cm from the tumor. A clean surgical margin was obtained and the patient was deemed to not require follow-up radiotherapy.
The patient’s postoperative course included regular follow-up at the CCF sarcoma center every 3-4 months with follow-up chest X-ray and right foot X-ray for one year. For 18 months thereafter, the follow-up interval was elongated to 6 months. At the 2.5-year mark, the interval was extended to 9 months. At 4 years, the interval was reduced to every 6 months. At 4.5 years, a chest CT demonstrated multiple bilateral subcentimeter, partially calcified airspace nodules of unknown etiology. Repeat CT in 3 months did not show significant interval findings. At time of writing, the patient has had no known recurrence.
Discussion
ES is a rare and ominous entity with an incidence established at 0.041 per 100,000. Prototypical presentation is in young adults and afflicts the hands and feet. Toes are rarely affected and to our knowledge this is the ninth published case of toes as the primary site [9]. ES exhibits an indolent growth pattern and is potentially painful when neural invasion is present. Local recurrence rate is 60-70% with half of tumors metastasizing. Like most sarcomas, typical sites of metastasis are lung, regional lymph nodes, and bone. In a retrospective study, it was found that the five year survival rate was 34% and the ten year survival rate 17% [10]. Relative rarity and innocuous presentation predispose ES to misdiagnosis, which is a frequently described occurrence in the literature. Enzinger et al. detailed 148 cases of pathological misinterpretation [11]. The malignancy is most often mistaken as a benign process such as innocuous fibromatosis. In our institution, clinical and radiologic assessment suggested probable ganglion cyst, neuroma/schwannoma or exuberant granulomata. However, meticulous histopathological examination revealed a diagnosis of ES and allowed for more conservative limb sparing surgery. The literature suggests that delay of correct diagnosis is the raison d'être of below the knee amputation in treatment of ES.
Sarcomas are complex and uncommon malignancies which pose a diagnostic challenge for a general pathologist. Over 50 types of sarcomas are reported in current literature. Microscopically, the low power field was deceptively bland, resembling plantar fibromatosis with the exception of punctuations of necrosis and dystrophic calcifications. Likewise, clinical and radiologic findings were also deceptively benign.
Awareness of ES is crucial to early recognition and diagnosis. Its aggressive nature and high impact on quality of life-particularly with its predilection for developing in young adults-should prompt consideration in the minds of clinicians when approaching seemingly benign lesions. As this case demonstrates, good outcomes are quite attainable if a prompt diagnosis is made.
References
- Sobanko JF, Meijer L, Nigra TP (2009) Epithelioid Sarcoma: A Review and Update. J Clin Aesthet Dermatol. 2: 49-54.
- Enzinger FM (1970) Epithelioid Sarcoma. A sarcoma simulating a granuloma or a carcinoma. Cancer. 26: 1029-1041.
- Fisher C (1988) Epithelioid Sarcoma: the spectrum of ultrastructural differentiation in seven immunohistochemically defined cases. Hum Pathol. 19: 265-275.
- Balighi K.,Farsinejad K.,Barzegar M, Naraghi Z, Mortazavizadeh SM (2001) A young Man With an Ulcerated Lesion on the Right Ankle. Acta Med Iran. 48: 72-4.
- Nishimura Y, Yamaguchi Y, Tomita Y (2010) Epithelioid sarcoma on the foot masquerading as an intractable wound for > 18 years. Clin Exp Dermatol. 35: 263-8.
- Toepfer A, Harrasser N, Dreyer F, Mogler C, Walther M, Eisenhart R (2017) Epithelioid Sarcoma of the Plantar Fascia. Mimicking Morbus Ledderhose –A. Severe pitfall for clinical and histopathological misinterpretation. Foot Ankle Surg. 23: e25-e30.
- Mascard E., Gaspar N., Brugieres L, Glorion C, Pannier S, et al. (2017) Malignant tumours of the foot and ankle. EFORT Open Rev. 2: 5.
- Hwang J, Fitzhugh VA, Kushal N, Beebe KS (2012) Epithelioid sarcoma: an unusual presentation in the distal phalanx of the toe. Am J Orthop. 41: 223-227.
- Visscher SA, Ginkel RJ, Wobbes T, Veth RP, Heuvel SE (2006) Epithelioid sarcoma: Still an only surgically curable disease. Cancer. 107: 606–612.
- Chase DR, Enzinger FM (1985) Epitheloid Sarcoma. Diagnosis, prognostic indicators and treatment. Am J. Surg Path. 9: 241-263.
Citation: Tynski Z, Barrett AJ, Chiang W (2018) An Epithelioid Sarcoma of the Right Foot: Raising Awareness of a High-Grade Malignancy. J Clin Exp Pathol 8:345. DOI: 10.4172/2161-0681.1000345
Copyright: © 2018 Tynski Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6414
- [From(publication date): 0-2018 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 5591
- PDF downloads: 823