An Assessment of Epidemiological Trends of Malaria in Lusaka Province of Zambia, 2009-2013
Received: 01-Aug-2015 / Accepted Date: 19-Aug-2015 / Published Date: 25-Aug-2015 DOI: 10.4172/2161-1165.1000198
Abstract
Background: Malaria is endemic in Zambia, with seasonal and geographical variations. It has over a decade been the leading cause of morbidity and mortality in the country. Malaria accounts for up to 50% of all infant mortality and 20% of all maternal mortality in Zambia and presents severe social and economic burdens on communities living in endemic areas.
Methods: A retrospective, observational study was performed at each of the four original districts in Lusaka Province of Zambia. Annual reported, district-level, aggregated malaria surveillance data were collected from all the four original districts of Lusaka Province from 2009 to 2013 using the Zambian District Health Information System (DHIS) through structured questionnaires. Data on annual provincial population were collected from Central Statistics Office (CSO) of the Republic of Zambia. District aggregated malaria data were analyzed using Microsoft Excel to show the trends of malaria morbidity and mortality in Lusaka Province by district.
Results: Lusaka Province malaria morbidity was 80 per 1000 in 2009, 90 per 1000 in 2010, 92 per 1000 in 2011, 40 per 1000 in 2012 and 60 per 1000 population in 2013. Malaria mortality rate was 0.13 per 1000 in 2009, 0.15 per 1000 in 2010, 0.06 per 1000 in 2011, 0.02 per 1000 in 2012 and 0.01 per 1000 population in 2013.
Conclusion: There was a significant reduction in the burden of malaria in Lusaka province from 2009 to 2013. However, malaria remains a major cause of morbidity and mortality in the Province with Luangwa District as the most affected. Although malaria affected everyone, children below five years of age were the most affected. Malaria control interventions should be intensified in the province more especially in the rural districts where malaria badly hit the province.
Keywords: Malaria; Epidemiology; Trends; Lusaka province
163732Introduction
For centuries, malaria has outranked warfare as a source of human suffering. It affects more than 489 million people worldwide every year and more than 1 million people die of malaria annually [1], thus making it a threat to human life.
Africa is the most affected continent with more than 90% of all malaria cases worldwide because of the combination of factors such as climate, mosquito vector, malaria parasite and poverty which combine to bear a negative impact on human health and retards development. Malaria disease slows economic growth by 1.3% per year translating into US $ 12 billion annual GDP loss across sub-Saharan Africa [2].
In Zambia, malaria is endemic with seasonal and geographical variations. It has for a long time remained the leading cause of morbidity and mortality in both the children and adults. Although malaria affects the whole population, the most vulnerable are children under the age of 5 years and pregnant women. Malaria accounts for up to 50% of all infant mortality and 20% of all maternal mortality in Zambia and presents severe social and economic burdens on communities living in endemic areas [3,4].
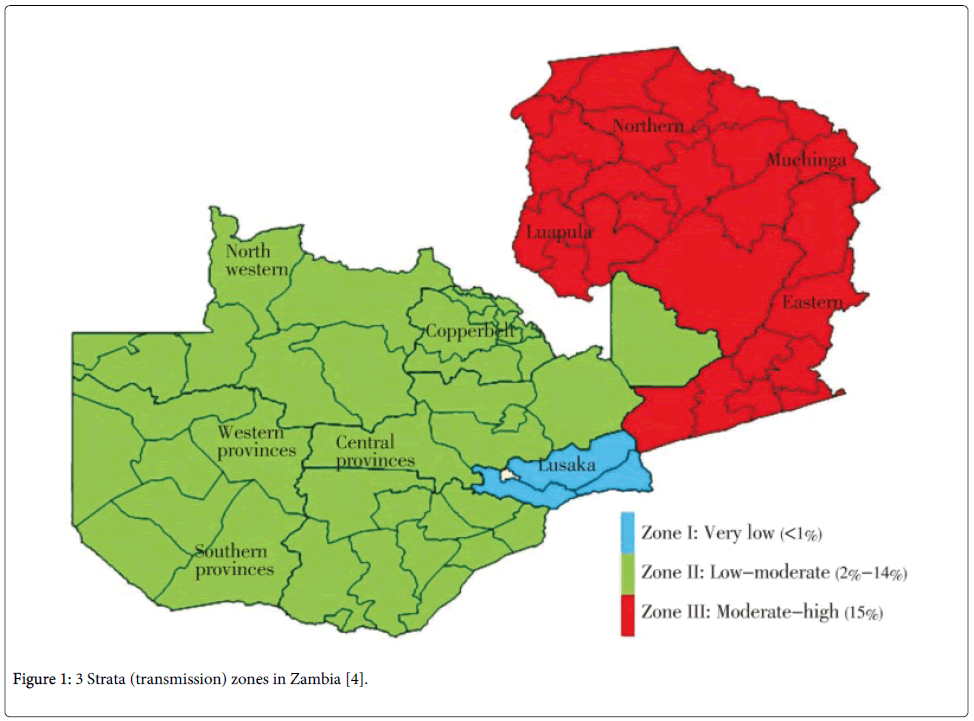
Epidemiologically, Zambia is categorized into three malaria zones namely, a low-transmission zone with parasite prevalence <1% located in south-eastern Zambia; a low stable-transmission region with a parasite prevalence of 10% located in north-western/south-central Zambia; and a high-transmission zone with a parasite prevalence of >20% located in northern and eastern Zambia [5]. Figure 1 shows malaria stratification in Zambia.
The country has three distinct seasons; a rainy season which starts from November and ending in May during which malaria transmission is highest, a cool dry season from late May to August, and a hot dry season from September to November. Malaria transmission is experienced in focal locations across the country throughout the year [5].
Plasmodium falciparum causes approximately 98% of malaria infection in Zambia while low frequency infections due to Plasmodium malariae and Plasmodium ovale also occur, and little or no transmission of Plasmodium vivax [6]. The main malaria vectors in Zambia are Anopheles arabiensis, Anopheles gambiae s.s. and Anopheles funestus s.s [7,8].
This study aimed at assessing epidemiological trends of malaria among various age groups in Lusaka Province of Zambia from 2009 to 2013 using malaria surveillance data from 2009 to 2013 through the Zambian District Health Information System (DHIS). The objective was to examine morbidity and mortality rates of malaria by district in Lusaka province from 2009 to 2013. Therefore, using malaria surveillance data collected from 2009 to 2013 through the Zambian District Health Information System, the burden of malaria in Lusaka Province of Zambia were evaluated.
Materials and Methods
Study location and population
Lusaka Province is located in the south-central part of Zambia and is the smallest province in the country with a surface area of 21,896 square kilometres. The province shares internal borders with Central, Eastern and Southern provinces, and international borders with Mozambique and Zimbabwe in Luangwa district. Lusaka province had an estimated population of 2,580,419 accounting for 17% of the country’s total population in the year 2013. Although it is the smallest province, Lusaka is the most populated province in the country [9,10].
Administratively, the province is divided into eight districts namely, Chilanga, Chirundu, Chongwe, Kafue, Luangwa, Lusaka, Rufunsa and Shibuyunji. However, only the four original districts were considered in the study as new districts were still part of the four original districts at the beginning of the study. Lusaka district, the capital city, is the smallest in terms of surface area (360 square kilometres), but had the largest population of 2,046,272 in 2013, thus accounting for 80% of total provincial population while Chongwe and Kafue districts had a population of 219,336 and 283,846 respectively. The border towns of the capital city have a mix of peri-urban and rural zones. Luangwa district had the smallest provincial population of 30,965 inhabitants and is entirely rural [9].
Study design
A retrospective, observational study was performed at each of the four original districts in Lusaka Province of Zambia from 2009 to 2013. Republic of Zambia Central Statistics Office (CSO) demographic data for Lusaka Province was used to determine the study population as follows:
•Annual district population to determine annual district malaria prevalence and annual provincial population to determine annual provincial malaria prevalence.
•Annual district population of under 5 years to determine annual district malaria prevalence in under 5 years of age and annual provincial population of under 5 years to determine annual provincial malaria prevalence in under 5 years of age.
•Annual district population of above 5 years to determine annual district malaria prevalence in above 5 years of age and annual provincial population of above 5 years to determine annual provincial malaria prevalence in above 5 years of age.
•Annual district population of expected pregnancies to determine annual district malaria prevalence in pregnant women and annual provincial population of expected pregnancies to determine annual provincial malaria prevalence in pregnant women, (where prevalence=cases/population x 1000). Central Statistics Office has National Census data and projections by district and province annually.
Furthermore, annual district malaria deaths per age group were used to determine annual district mortality rate for that particular age group and; annual provincial malaria deaths per age group were used to determine annual provincial mortality rate for that particular age group. Total annual district malaria deaths were used to determine annual district mortality rate and total annual provincial malaria deaths were used to determine annual provincial mortality rate, [where mortality rate=(number of deaths/population) x 1000].
Data collection and analysis
Annual reported, district-level, aggregated malaria surveillance data were collected from all the four original districts of Lusaka Province from 2009 to 2013 using the Zambian District Health Information System (DHIS) through structured questionnaires. 5 questionnaires were used per district to capture data for a 5 year period. DHIS data are collected at health centers and district hospitals in paper form and are sent to the District Health Office (DHO) for data entry and validation in the DHIS. The DHO sends the district-level data to the provincial office for further processing and aggregation. The consolidated provincial data are then sent to the National Malaria Control Centre (NMCC) and Ministry of Health Headquarters, which in turn provide feedback and technical support to the provinces, districts and health facilities. Data on annual provincial population were collected from Central Statistics Office (CSO) of the Republic of Zambia. District aggregated malaria surveillance data were analyzed using Microsoft Excel to show the trends of malaria morbidity and mortality in Lusaka Province by district.
Results
Changes in the burden of malaria in Lusaka province
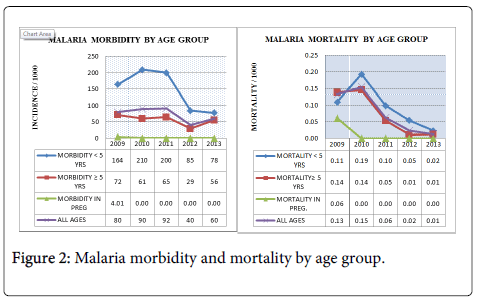
This retrospective study assessed epidemiological trends of malaria morbidity and mortality in Lusaka Province from 2009 to 2013. Malaria morbidity in the province was 80 per 1000 population in 2009. Morbidity increased to 90 and 92 per 1000 population in 2010 and 2011 respectively. The year 2012 reported 40 per 1000, which was half the baseline morbidity while the year 2013 reported 60 per 1000 population. In 2009 the baseline year, malaria mortality was 0.13 per 1000 population, which slightly increased to 0.15 per 1000 in 2010 and then decreased to 0.06 per 1000 in 2011, 0.02 per 1000 in 2012 and 0.01 per 1000 in 2013. Figure 2 shows malaria morbidity and mortality trends in Lusaka Province from 2009 to 2013.
Provincial malaria burden in under five years children
In 2009, Lusaka Province malaria morbidity in children under five years was 164 per 1000 population. Malaria morbidity increased to 210 per 1000 in 2010 before decreasing gradually to 78 per 1000 in 2013. A similar trend was observed in malaria mortality. In 2009, malaria mortality was 0.11 per 1000 population but increased to 0.19 per 1000 population in 2010 before showing a gradual decrease to 0.02 per 1000 in 2013 (Figure 2).
Provincial malaria burden in above five years
In 2009, Lusaka Province malaria morbidity in above five years was 72 per 1000 population. Malaria morbidity decreased from 2010 to 2013 with fluctuations; morbidity was 61 per 1000 population in 2010 and 56 per 1000 population in 2013. Malaria mortality in above five years showed a steady decline from 2009 to 2013. In 2009 and 2010, mortality was 0.14 per 1000, 0.05 per 1000 in 2011and 0.01 per 1000 in 2012 and 2013. Figure 2 shows these malaria morbidity and mortality trends.
Provincial malaria burden in pregnancy
Provincial malaria morbidity in pregnancy was 4.01 per 1000 population in 2009. Malaria prevalence decreased to 0 per 1000 from 2010 through to 2013. This trend was similar in malaria mortality where 0.06 deaths were reported per 1000 population in 2009 and then death rate decreased to 0 per 1000 from 2010 through to 2013 in pregnant women (Figure 2).
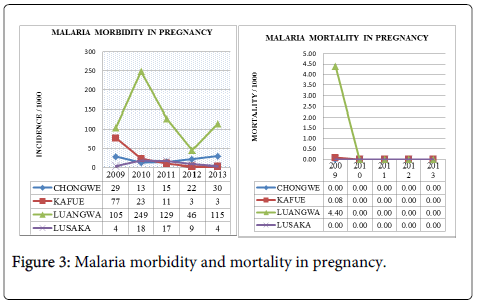
District malaria burden in pregnancy
Luangwa District reported the highest malaria morbidity in pregnancy with a maximum of 249 and minimum of 46 per 1000 population during the study period. Kafue District was second with a maximum of 77 and minimum of 3 per 1000 followed by Chongwe with a maximum of 30 and minimum of 13 per 1000 and lastly Lusaka District with maximum of 18 and minimum of 4 per 1000 population of pregnant women. Figure 3 shows these trends.
Luangwa District also reported the highest malaria mortality of 4.4 per 1000 population while Kafue District reported 0.08 deaths per 1000 population during the baseline year 2009 in pregnant women. Lusaka and Chongwe Districts reported no death in 2009. All the four districts in Lusaka Province reported no malaria death in pregnancy from 2010 to 2013 (Figure 3).
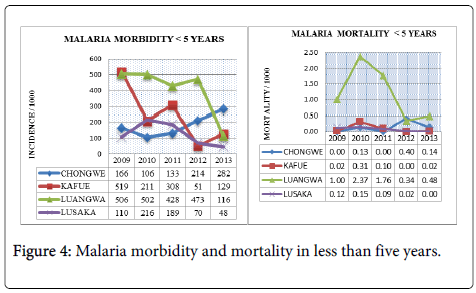
District malaria burden in under five years children
Kafue District reported the highest malaria morbidity of 519 per 1000 population in children aged below five years during the baseline year 2009. Kafue District reported a sharp decline in malaria morbidity from the year 2010 through to 2013. Luangwa District reported malaria morbidity of 506 per 1000 in 2009 and 116 per 1000 in 2013 presenting the overall highest malaria morbidity in under five year children in Lusaka Province. In 2009, Lusaka District reported malaria morbidity of 110 per 1000 population in under five year children which increased to 216 per 1000 in 2010 before steadily declining to 48 per 1000 in 2013. Malaria morbidity in children below five years for Chongwe District increased from 166 per 1000 in 2009 to 282 per 1000 in 2013 (Figure 4).
Luangwa District reported the highest malaria mortality in the province from 2009 to 2013 in children less than five years of age. Luangwa reported maximum death rate of 2.37 and minimum of 0.34 per 1000 population during the study period. Chongwe, Kafue and Lusaka Districts reported malaria mortality of less than 0.41 per 1000 population from 2009 to 2013 in children less than five years of age. Figure 4 shows these trends.
District malaria burden in above five years
Luangwa District reported the highest malaria morbidity in Lusaka province from 2009 to 2013 in above five years. Luangwa District reported maximum malaria morbidity of 1,511 per 1000 in 2010 and minimum of 689 per 1000 population in 2013. Three other districts namely Chongwe, Kafue and Lusaka reported malaria morbidity of less than 172 per 1000 population from 2009 to 2013 in the above five years category. Figure 5 shows these trends.
Luangwa District reported the highest malaria mortality in the above five years category in the province. Luangwa District reported maximum death rate of 1 per 1000 and minimum of 0 per 1000 populations from 2009 to 2013. Chongwe, Kafue and Lusaka Districts reported malaria mortality of less than 0.17 per 1000 populations in above five years category during the study period. Figure 5 shows these trends.
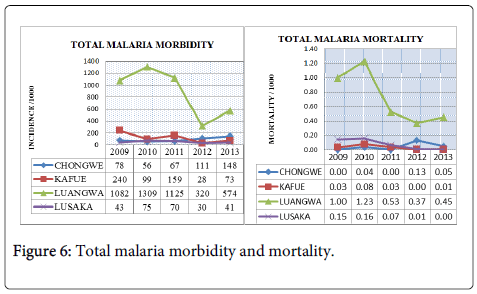
Total malaria burden by district
Luangwa District reported the highest malaria morbidity from 2009 to 2013. In 2009, the baseline year, Luangwa District reported 1,082 per 1000 populations which increased to 1,309 per 1000 populations in 2010. In 2011, malaria morbidity was 1,125 per 1000 and reduced to 320 per 1000 in 2012 before showing a slight increase in 2013 where morbidity was 574 per 1000 populations. From 2009 to 2013, Chongwe, Kafue and Lusaka Districts reported malaria morbidity of less than 250 per 1000 populations (Figure 6).
Luangwa District reported the highest malaria mortality in Lusaka Province. Luangwa reported the maximum of 1.23 and minimum of 0.37 deaths per 1000 population from 2009 to 2013. Chongwe, Kafue and Lusaka Districts reported malaria mortality of less than 0.17 per 1000 from 2009 to 2013. Figure 6 shows these trends.
Discussion
Findings of the assessment of epidemiological trends of malaria in Lusaka Province have shown a general decrease in both morbidity and mortality of malaria from 2009 to 2013. By age category, children under five years were the most affected by malaria followed by the adult category and then pregnant women. Although, there was a general reduction in the malaria trend from 2009 to 2013, this study showed that malaria morbidity in under five years old children was more than double that of the above five years category in Lusaka province from 2009 to 2013. These results are similar to a study conducted in Papua New Guinea where malaria morbidity has been found highest among children less than five years of age [11,12]. A similar study has been conducted in Ethiopia and findings were that children below five years of age were more susceptible and affected by malaria scourge [13].
Malaria mortality showed a similar trend to that of morbidity from 2009 to 2013 in Lusaka Province. Children below five years were the most affected as compared with the above five years and the general trend decreased steadily from 2009 to 2013. Results of this study are similar to studies that have been conducted to assess the prevalence of malaria in children below five years and above five years [14]. Studies conducted to assess the prevalence of malaria in children below five years and above five years have all shown that children below five years of age were more affected by malaria compared with adults. According to these studies [14], children below two months old have passive immunity offered by maternal antibodies but this temporal immunity is lost after two months leaving babies vulnerable not only to malaria but also other infections. The naturally acquired immunity in children below the age of five is very low hence their vulnerability to malaria infections compared with above five years category [14].
At district level, Luangwa has been the most affected district in Lusaka Province from 2009 to 2013. During the same period, Chongwe, Kafue and Lusaka Districts reported malaria morbidity of less than 250 per 1000 populations. Luangwa District also reported the highest malaria mortality in all age categories compared with the other three districts.
This study revealed that malaria prevalence and transmission intensity was significantly higher in the rural areas, followed by peri-urban and then urban areas. Luangwa District was the most affected followed by Kafue, Chongwe and Lusaka Districts in that order. Luangwa is an entirely rural district of Lusaka Province and its geographical location in the valley as well as at the confluence of two big rivers, the Luangwa and Zambezi has so much influence in the mosquito development hence the persistence and high prevalence of malaria in the district. These results are similar with a study conducted in Ethiopia where malaria prevalence and transmission intensity was significantly higher in the villages as compared to the non-resettlement villages (peri-urban areas). Individuals living in typical villages were three times more likely to have P. falciparum infection as compared with individuals living in peri urban areas [15,16].
Limitations
This study has several limitations; analyses were based on routinely collected data with the possibilities of both over and under reporting malaria cases. Data accuracy and completeness were not systematically assessed as only aggregated annual figures were collected. Both RDT and microscopy have limited sensitivity and specificity, and are particularly likely to misclassify individuals with low levels of parasitaemia. However, the use of all positive malaria cases and total population by age category gives a good result as the sample representation is large.
Conclusion
There was a significant reduction in the burden of malaria in Lusaka province from 2009 to 2013. During this period, malaria morbidity decreased from 80 per 1000 to 60 per 1000 population. However, malaria remains a major cause of morbidity and mortality in Lusaka Province especially in Luangwa District where both morbidity and mortality has been very high during the study period. Although malaria affected everyone, children younger than five years of age were the most affected. Malaria control interventions should be intensified strategically in the province more especially in the rural districts where malaria badly hit the province.
Acknowledgements
Compliments go to the Ministry of Health of the Republic of Zambia for allowing us to conduct the study in Lusaka Province. Credit has been given to the original author of Figure 1 [4] for granting us permission to use the map for the purpose of this study. The principle author is supported by Qigui Liu, Gui Rong Song and Xiaofeng Li from the Department of Epidemiology and Biostatistics, School of Public Health, Dalian Medical University, Dalian 116044, Liaoning, PR China.
Authors’ Contributions
Maybin Kalubula designed the study, developed and drafted the manuscript. Qigui Liu and Gui Rong Song conceived the study and participated in the analysis. Xiaofeng Li conceived the study, participated in the programming and review of the manuscript. All authors read and approved the final manuscript.
References
- (2012) World Health Organization Zambia Country Office Annual Report 2012. World Health Organization Country Office, Lusaka.
- (2011) NMCC: Zambia national malaria control program performance review. Lusaka, Zambia: National Malaria Control Centre, Ministry of Health.
- Masaninga F, Chanda E, Chanda-Kapata P,Hamainza B,Masendu HT, et al. (2013)Review of the malaria epidemiology and trends in Zambia. Asian Pac J Trop Biomed 3: 89-94.
- Chanda E, Hemingway J, Kleinschmidt I, Rehman AM, Ramdeen V, et al. (2011) Insecticide resistance and the future of malaria control in Zambia. PLoS One 6:e24336.
- Norris LC, Norris DE (2011) Efficacy of long-lasting insecticidal nets in use in Macha, Zambia, against the local Anopheles arabiensis population. Malar J 10:254.
- Central Statistics Office (2013) Population and Housing. Central Statistics Office, Lusaka.
- Lusaka provincial Health Office (2012) Lusaka province Annual Statistical Bulletin 2011. Provincial Health Office, Lusaka. p.9.
- Lin E, Kiniboro B, Gray L, Dobbie S, Robinson L, et al. (2010) Differential patterns of infection and disease with P. falciparum and P. vivax in young Papua New Guinean children. PLoS One 5:e9047.
- Marsh K, Kinyanjui S (2006) Immune effector mechanisms in malaria. Parasite Immunol 28:51-60.
- Yeshiwondim AK, Gopal S, Hailemariam AT, Dengela DO, Patel HP (2009) Spatial analysis of malaria incidence at the village level in areas with unstable transmission in Ethiopia. Int J Health Geogr 8:5.
- Deressa W, Hailemariam D, Ali A (2007) Economic costs of epidemic malaria to households in rural Ethiopia. Trop Med Int Health 12:1148-56.
- Moormann AM (2009) How might infant and paediatric immune responses influence malaria vaccine efficacy? Parasite Immunol, Sep; 31: 547-559.
- Cox JSH, Mouchet J, Bradley DJ (2002) Determinants of malaria in Sub-Saharan Africa. InThe Contextual Determinants of Malaria. Edited by Casman EA, Dowlatabadi H. Resources for future press, Washington DC, 167-186.
Citation: Kalubula M, Li XF, Liu Q, Song GR (2015) An Assessment of Epidemiological Trends of Malaria in Lusaka Province of Zambia, 2009-2013. Epidemiology (sunnyvale) 5:198. DOI: 10.4172/2161-1165.1000198
Copyright: © 2015 Kalubula M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.