Research Article Open Access
An Analysis of a New Diagnostic Test for Children with Acute Appendicitis: Plasma Leptin Level
Harun Resit Ayangil1, Mustafa Erman Dorterler2* and Cuneyt Turan3
1Deparment of Pediatric Surgery, Ac├?┬▒badem Hospital, Kayseri, Turkey
2Deparment of Pediatric Surgery, Harran University Medical School, ├?┬?anl├?┬▒urfa, Turkey
2Deparment of Pediatric Surgery, Erciyes University Medical School, Kayseri, Turkey
- *Corresponding Author:
- Mustafa Erman Dorterler
Department of Pediatric Surgery
Harran University, ├?┬?anl├?┬▒urfa, Turkey
Tel: +90 (414) 318 30 30
Fax:+90 (414) 318 31 92
E-mail: m.e.dorterler@hotmail.com
Received date: March 16, 2016; Accepted date: August 25, 2016; Publication date: September 10, 2016
Citation: Ayangil HR, Dorterler ME, Turan C (2016) An Analysis of a New Diagnostic Test for Children with Acute Appendicitis: Plasma Leptin Level. J Gastrointest Dig Syst 6:470. doi: 10.4172/2161-069X.1000470
Copyright: ©2016 Ayangil HR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Aim: In the diagnosis of acute appendicitis, the most frequently-applied laboratory tests are blood leukocyte level (WBC) and serum C-reactive protein (CRP). In recent years, it has been thought that the leptin hormone level, which has been proven to be raised in acute inflammation, could be used diagnostically in patients with acute appendicitis. In this study, we aimed to determine the relationship between WBC, CRP, and leptin levels with inflammation in acute appendicitis and to define the role of leptin in the mechanism underlying loss of appetite, which is the most frequently observed symptom.
Materials and method: The study comprised 40 patients diagnosed with acute appendicitis (AA) in the Pediatric Surgery Department and a control group of 20 age-matched patients. Blood samples were taken from all subjects in both groups and the levels of WBC, CRP and leptin were measured. Body mass index was calculated and all findings were compared.
Results: In the AA group, the median leptin value was measured as 1.24 ng/ml preoperatively, 1.37 ng/ml perioperatively, and 0.81 ng/ml 2 days postoperatively. The leptin value in the control group was 1.90 ng/ml. No statistically significant difference was found between the two groups with respect to the preoperative and perioperative leptin values (p>0.05). The postoperative 2nd day leptin values of the AA group were statistically significantly lower than those of the control group (p<0.05).
Conclusions: In cases of suspected acute appendicitis, leptin can be a useful diagnostic parameter since its levels increase during the early stages of inflammation.
Keywords
Acute appendicitis; Inflammation; Leptin
Introduction
Acute appendicitis in childhood requires emergency surgery. Although the patient’s history, physical examination, and laboratory tests are used in diagnosis, it can be difficult to make a definitive diagnosis in every case [1]. In addition, assistive diagnostic methods are being developed and new research is ongoing to reduce the rates of negative appendectomy and perforation [2-4].
Laboratory tests are often used in the diagnosis of acute appendicitis. Currently, the most commonly-used of these tests are measurements of blood leukocyte (WBC) and serum C-reactive protein (CRP) levels. However, just as the results of these tests could also reach high levels in several similar diseases, normal values are insufficient to discount a diagnosis of acute appendicitis [5,6]. Another criteria for diagnosis is the symptomology of the patient. A loss of appetite is significant within this symptomology and is present in most acute appendicitis patients. The leptin hormone is known to have an effect on the development of loss of appetite by affecting the hypothalamus, which reduces appetite [7].
Leptin is a hormone expressed from fat tissue cells that plays an important role in natural and acquired immunity. In cases of infection and inflammation, the leptin levels of the host increase and show an anti-inflammatory effect. In addition to tumor necrotizing factor alpha (TNF-a), interleukin 1 (IL–1), and interleukin 6 (IL–6) in anorexia, the increasing leptin level observed during infections is believed to be influential [8].
The aim of this study was to determine the relationship between WBC, CRP, and leptin levels with inflammation in cases of acute appendicitis, and to define the role of leptin in the mechanism underlying loss of appetite, which is the most frequently-observed symptom.
Materials and Method
Approval for this study was granted by the Local Ethics Committee (Decision no: 01/30) and support was provided by the Research Fund of Erciyes University (Project No: TT-06-23). The study comprised 40 patients diagnosed with acute appendicitis in the Pediatric Surgery Department - the acute appendicitis group (AA) - and 20 age-matched children as a control group.
The AA group had a mean age of 7.3 years (range: 2-10 years) and included patients considered to have acute appendicitis according to their medical history, as well as to clinical and ultrasonography (USG) examinations, and whose diagnosis was confirmed macroscopically during surgery. Patients were excluded from this group if they were considered to have acute appendicitis clinically and on USG, but were not confirmed by surgery, or if they were found to have another inflammatory disease as well as appendicitis.
The control group had a mean age of 5.6 years (range: 2-10 years) and included patients who presented at the Pediatric Surgery Polyclinic complaining of constipation but who displayed no inflammatory disease on physical examination, or clinically at the time of enrollment into the study, or in the anamnesis.
Method
Patients in the AA group who presented at the Pediatric Emergency Polyclinic complaining of abdominal pain and who were considered to have acute appendicitis clinically and from their medical history, had a 10 cc venous blood sample withdrawn into a sterile biochemistry tube to allow the serum leptin and CRP levels to be examined and a 1 ml sample withdrawn into an ethylenediaminetetraacetic acid (EDTA) tube to examine the WBC level at the time of presentation. Then, a standing direct radiograph and abdominal USG were performed.
Findings supporting a diagnosis of acute appendicitis were defined as an appendix of diameter>6 mm, target sign, distension or obstruction in the appendix lumen, thickening of the appendix wall>2 mm, loss of peristalsis in the appendix, free fluid in the surroundings, or fecalith in the appendix, and surgery was subsequently planned for these patients [9]. For the subjects in the control group, a blood sample was taken only once for the measurement of WBC, leptin, and CRP and these were stored in the same manner as before.
Body mass index (BMI) was calculated for all patients in the AA and control groups, and the BMI values were compared with those of healthy children aged 2-10 years.
Statistical Analysis
Statistical analysis was performed using SPSS for Windows software (ver. 13.0; SPSS Inc., Chicago, IL, USA). A value of p<0.05 was accepted as statistically significant. Conformity to a normal distribution of continuous quantitative variables was examined with the Kolmogorov-Smirnov test. Data with a normal distribution were provided as means ± standard deviation (SD). To determine differences between the two groups, Student’s t-test was applied. To assess differences between time periods (preoperative, perioperative, postoperative), a repeated variance analysis was used.
Quantitative data not conforming to a normal distribution, such as CRP and leptin, were provided as median values (min-max). The Mann-Whitney U test was applied to determine the difference between the two groups. The Friedman test was used to assess differences according to time period; to determine from which time period the difference originated, the Mann Whitney U-test was used with Bonferroni correction applied.The relationship between variables was examined by calculating the Spearman correlation coefficient, and a regression curve was plotted. Qualitative data were provided as percentages. The Chi-square test was applied to assess differences between the two groups. When calculating the sensitivity and specificity of the CRP and leukocyte values in the diagnosis of acute appendicitis, the standard formulae below were used:
Sensitivity=real positive/(real positive+false negative) × 100
Specificity=real positive/(real negative+false positive) × 100
Results
The patients in the AA group comprised 27 (67.5%) males and 13 (32.5%) females, with a mean age of 7.3 ± 2.5 years, a mean body weight of 25.9 ± 9.1 kg, and a BMI of 17.1 ± 2.5 kg/m2.
The patients in the control group comprised 15 (75%) males and 5 (25%) females, with a mean age of 5.6 ± 2.1 years, mean body weight of 20.2 ± 6.2 kg and a BMI of 16 ± 1.5 kg/m2.
No statistically significant difference was determined between the two groups in respect of BMI (p>0.05) (Table 1). The mean duration of a loss of appetite was determined as 37.6 ± 33.8 hours.
| Group I (AA) n = 40 (x ± sd) | Group II (Control) n = 20 (x ± sd) | t | p | |
|---|---|---|---|---|
| Age (yr) | 7.3 ± 2.5 | 5.6 ± 2.1 | 2.4 | 0.01 |
| Weight (kg) | 25.9 ± 9.1 | 20.2 ± 6.2 | 2.4 | 0.01 |
| Height (cm) | 121.4 ± 17.9 | 110.9 ± 12.7 | 2.3 | 0.02 |
| BMI (kg/m2) | 17.1 ± 2.5 | 16 ± 1.5 | 1.6 | 0.1 |
Table 1: Age, weight, height, and BMI variables of the groups.
Of the patients diagnosed with acute appendicitis, the appendix was found to be perforated in 26 (65%) cases and not perforated in 14 (35%). The mean body weight of the patients with a perforated appendix was determined as 23.5 ± 8.3 kg, the mean BMI as 16.6 ± 2.0 kg/m2, and the mean duration of the loss of appetite as 48.9 ± 36.7 hours. In patients with a non-perforated appendix, the mean body weight was determined to be 30.4 ± 9.2 kg, the mean BMI as 18.0 ± 3.3 kg/m2, and the mean duration of loss of appetite as 16.9 ± 11.7 hours.
The body weight of the children with perforated appendices was lower than those with non-perforated appendices and the duration of the loss of appetite was longer. These differences were determined to be statistically significant (p<0.05). No significant difference was determined BMI between those with a perforated appendix and those without (p>0.05) (Table 2).
| Perforated appendix n = 26 (x ± sd) | Non-perforated appendix n = 14 (x ± sd) | t | p | |
|---|---|---|---|---|
| Age (yr) | 6.9 ± 2.6 | 8.0 ± 2.3 | 1.2 | 0.2 |
| Weight (kg) | 23.5 ± 8.3 | 30.4 ± 9.2 | 2.4 | 0.02 |
| Height (cm) | 117.4 ± 19.2 | 128.9 ± 12.8 | 1.9 | 0.06 |
| BMI (kg/m2) | 16.6 ± 2.0 | 18.0 ± 3.3 | 1.7 | 0.1 |
| Loss of appetite (h) | 48.9 ± 36.7 | 16.9 ± 11.7 | 3.1 | 0 |
Table 2: Distribution of variables between the two groups according to the appendix perforation status.
The WBC values of the patients were measured as 17,280 ± 5,009 mm3 preoperatively, 162,09 ± 4,258 mm3 perioperatively, and 11,362 ± 2,876 mm3 on the 2nd day postoperatively.
In the control group, the WBC value was measured as 7,697 ± 1,559 mm3. The WBC values of the patient group were significantly higher than those of the control group and the difference was determined to be statistically significant (p<0.05) (Table 3).
| Group I (AA) n = 40 (x ± sd) | Group II (Control) n = 20 (x ± sd) | t | p | |
|---|---|---|---|---|
| Preoperative WBC | 17,280 ± 5009 | 7,697 ± 1559 | 8.3 | 0 |
| Perioperative WBC | 16,209 ± 4258 | 7,697 ± 1559 | 8.6 | 0 |
| Postoperative Day 2 WBC | 11,362 ± 2876 | 7,697 ± 1559 | 5.3 | 0 |
Table 3: Distribution of WBC values.
The WBC values of the patients with a perforated appendix were measured as 17,290 ± 5,284 mm3 preoperatively, 16,425 ± 4,311 mm3 perioperatively, and 11,839 ± 3,023 mm3 on the 2nd day postoperatively.
The WBC values of the patients with a non-perforated appendix were measured as 17,262 ± 4,645 mm3 preoperatively, 15,807 ± 4,288 mm3 perioperatively, and 10,476 ± 2,435 mm3 on the 2nd day postoperatively.
No statistically significant difference was found in WBC values between the patients with a perforated appendix and those without (p>0.05) (Table 4).
| Perforated appendix n = 26 (x ± sd) | Non-perforated appendix n = 14 (x ± sd) | t | p | |
|---|---|---|---|---|
| Preoperative WBC | 17,290 ± 5,284 | 17,262 ± 4,645 | 0.1 | 0.98 |
| Perioperative WBC | 16,425 ± 4,311 | 15,807 ± 4,288 | 0.4 | 0.66 |
| Postoperative Day 2 WBC | 11,839 ± 3,023 | 10,476 ± 2,435 | 1.4 | 0.15 |
Table 4: Distribution of WBC values in patients with and without a perforated appendix.
The median CRP value of the patients in the AA group was determined as 96.3 mg/L preoperatively, 107 mg/L perioperatively, and 111 mg/L on the 2nd day postoperatively.
The median value of the patients in the control group was 3.17 mg/L, which was within normal limits. The CRP values of the patients were significantly higher than those of the control group and the difference was determined to be statistically significant (p<0.05) (Table 5).
| Group I (AA) n = 40median (min-max) | Group II (Control) n = 20 median (min-max) | p | ||
|---|---|---|---|---|
| CRP | Preoperative | 96.3 (5.6-618) | 3.17 (3.17-4.49) | 0 |
| Perioperative | 107 (2.9-331) | 3.17 (3.17-4.49) | 0 | |
| Postoperative Day 2 | 111 (7.6-288) | 3.17 (3.17-4.49) | 0 | |
| Leptin | Preoperative | 1.24 (0.01-21.23) | 1.90 (0.35-4.52) | 0.52 |
| Perioperative | 1.37 (0.01-20.05) | 1.90 (0.35-4.52) | 0.94 | |
| Postoperative Day 2 | 0.81 (0.01-9.30) | 1.90 (0.35-4.52) | 0.01 |
Table 5: Distribution of CRP and leptin values.
The median CRP value of the patients with a perforated appendix was determined as 149.5 mg/L preoperatively, 133 mg/L perioperatively, and 132 mg/L on the 2nd day postoperatively.
The median CRP value of the patients with a non-perforated appendix was determined as 32.3 mg/L preoperatively, 37.4 mg/L perioperatively, and 55.75 mg/L on the 2nd day postoperatively.
The CRP values of the patients with a perforated appendix were found to be significantly higher than those of the patients with a nonperforated appendix (p<0.05) (Table 6).
| Perforated appendix n = 26 median (min-max) | Non-perforated appendix n = 14 median (min-max) | p | ||
|---|---|---|---|---|
| CRP | Preoperative | 149.5 (30–618) | 32.3 (5.64–138) | 0 |
| Perioperative | 133 (4.13–331) | 37.4 (2.98–142) | 0 | |
| Postoperative Day 2 | 132 (57.3–288) | 55.75 (7.63–160) | 0 | |
| Leptin | Preoperative | 0.79 (0.01–13.0) | 3.32 (0.01–21.23) | 0 |
| Perioperative | 0.97 (0.01–9.07) | 3.18 (0.01–20.05) | 0.04 | |
| Postoperative Day 2 | 0.51 (0.01–3.42) | 2.02 (0.21–9.30) | 0 |
Table 6: CRP and leptin values in patients with and without a perforated appendix.
The median leptin value of the patients in the AA group was determined as 1.24 ng/l preoperatively, 1.37ng/l perioperatively, and 0.811 ng/l on the 2nd day postoperatively. The median leptin value of the patients in the control group was 1.9 ng/l. No statistically significant difference was determined between the two groups in respect of the preoperative and perioperative leptin values (p>0.05). The postoperative 2nd day leptin value of the patients was found to be lower than that of the control group and the difference was determined to be statistically significant (p<0.05) (Table 5).
The leptin value of the patients with a perforated appendix was determined as 0.79 ng/l preoperatively, 0.97 ng/l perioperatively, and 0.51 ng/l on the 2nd day postoperatively.
The leptin values of the patients with a non-perforated appendix were determined as 3.32 ng/l preoperatively, 3.18 ng/l perioperatively, and 2.02 ng/l on the 2nd day postoperatively.
The leptin values of the patients with a non-perforated appendix were significantly higher than those of the patients with a perforated appendix (p<0.05) (Table 6).
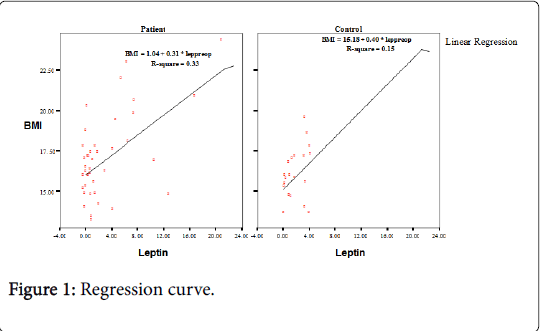
A statistically significant positive correlation was determined between BMI and leptin in both the patient and the control groups (r: 0.35, p: 0.02) (Figure 1).
The WBC values were observed to decrease through the timed measurements preoperatively, perioperatively, and 2 days postoperatively (17,280 mm3, 16,209 mm3 and 11,362 mm3 respectively) and the difference between the values was found to be statistically significant (p<0.05). When the CRP preoperative values were compared with those measured on the 2nd day postoperatively, no evident decrease was observed and the difference in the values was not statistically significant (p>0.05). The leptin values measured on the 2nd day postoperatively were seen to be lower than the preoperative values (preoperative 1.24 ng/ml, postoperative 2nd day 0.81 ng/ml) and the difference was determined to be statistically significant (p<0.05) (Table 7).
| Preoperative | Perioperative | Postoperative Day 2 | p | |
|---|---|---|---|---|
| n = 40 | n = 40 | n = 40 | ||
| WBC (x ± sd) | 17,280 ± 5,000*bc | 16,209 ± 4,258*ac | 11,362 ± 2,876*ab | 0 |
| CRP median (min-max) | 96.3 (5.64–618) | 107 (2.98–331) | 111 (7.63–288) | 0.72 |
| Leptin median (min-max) | 1.24 (0.01–21.23)c | 1.37 (0.01–20.05)c | 0.81 (0.01–9.30)ab | 0 |
Table 7: WBC, CRP, and leptin values measured at different times in the patient group. a: indicates a difference compared to the preoperative value, b: indicates a difference compared to the perioperative value, c: indicates a difference compared to the postoperative day 2 value, *: 0.05 was accepted as the level of statistical significance.
In the diagnosis of acute appendicitis, the sensitivity of WBC was calculated as 90% and the specificity was 100%. Of these patients, the CRP levels were high in 39 cases and normal in 1. The sensitivity of CRP was calculated as 97.5% and the specificity as 100%.
Discussion
WBC and CRP are laboratory tests that are frequently applied to children suspected of having acute appendicitis. WBC, which increases in the early stages of the disease and before perforation occurs, has not been reported to show any statistically significant difference between patients with perforated appendices and those without. However, the CRP level can reach a more significant height, especially in acute appendicitis cases, which have a tendency to perforate or develop abscesses, and the measurement of CRP has been shown to provide more valuable data for patients with suspected acute appendicitis [9-13]. The data obtained in the current study indicate a similar situation. Although no statistically significant difference was determined between patients with a perforated appendix and those with a non-perforated appendix in respect of the WBC values, the CRP values of patients with a perforated appendix were found to be higher than those of patients with a non-perforated appendix.
Serum leptin, which has been found in increased levels in experimental inflammation models, is another laboratory parameter that we investigated in the current study. Leptin is a hormone with a protein-like structure that contains 167 amino acids and resembles a cytokine. The primary role of leptin in the body is to reduce appetite via negative feedback to the hypothalamus region of the brain, to control food intake and, by regulating energy metabolism, to prevent the development of obesity [14]. Leptin is known to play a significant role in natural and acquired immunity. It has been suggested that leptin is an important factor in the response to inflammation since the leptin level increases during inflammation and infection. Host anorexia is believed to be the acute phase response observed during the course of infections [15,16].
In the current study, no statistically significant difference was determined in preoperative and perioperative leptin values between the patients diagnosed with acute appendicitis and the control group. However, in the evaluation conducted within the patient group, the leptin values of the patients with a perforated appendix were observed to be higher than those of patients with a non-perforated appendix. When the data of postoperative 2nd day were examined, the leptin values of the patient group were determined to be significantly lower than those of the control group.
There is known to be a positive correlation between BMI and leptin expression [17,18]. In the current study, no statistically significant difference was determined between the patient and control groups in BMI, nor between those patients with and without a perforated appendix. However, in both the patient and control groups a significant positive correlation between BMI and leptin was determined with a regression curve (Figure 1). Of the 40 patients in the AA group, 3 had a BMI>95th percentile and were thus classified as obese.
In two of these three patients, the leptin values were determined to be high and the appendix was not perforated, and in the other patient the leptin value was high and the appendix was perforated. In 12 of the 14 patients with a non-perforated appendix, a high leptin value was determined independently of BMI. In 20 of the 26 patients with a perforated appendix, leptin values were found to be low. From these findings it can be concluded that, in acute appendicitis patients with a non-perforated appendix, the leptin level increased, and in those patients with a perforated appendix it decreased. These results conform with previous reports in the literature [14,15].
A loss of appetite in patients, which causes weight loss by reducing food intake, is thought to be associated with both the severity and duration of inflammation and the level of leptin at onset. In addition, in patients with a perforated appendix who are subjected to the stress of undergoing surgery, a delayed start to nutrition causes a drop in leptin levels making weight loss more evident. Leptin is known to exert an inhibitory effect on hunger and weight loss. The decrease seen in leptin levels on the 2nd postoperative day in this study is consistent with previous reports in the literature [19-22].
In conclusion, leptin, which is initially defined as a satiety factor, is involved in the regulation of endocrine and immune functions in addition to energy regulation, and its acute increase as a result of stimuli, similar to other cytokines, shows that leptin is part of the acute phase inflammation response. The expression of leptin is increased due to the process of developing acute appendicitis. Due to the increase in leptin in the early phase of inflammation, it can be recommended as a useful diagnostic parameter in cases of suspected acute appendicitis. In addition, as the high level of leptin in a non-perforated acute appendicitis decreases together with perforation, it can be useful in terms of identifying the course of the perforation.
References
- Shakhatreh HS (2000) The accuracy of C-reactive protein in the diagnosis of acute appendicitis compared with that of clinical diagnosis. Med Arh 54: 109-110.
- Hallan S, Asberg A (1997) The accuracy of C-reactive protein in diagnosing acute appendicitis--a meta-analysis. Scand J Clin Lab Invest 57: 373-380.
- Meisner M, Reinhart K (2001) Diagnosis of sepsis: the role of parameters of the inflammatory response. NVCI 5:41-45.
- Chen SC, Wang SM (1996) C-reactive protein in the diagnosis of acute appendicitis. Am J Emerg Med 14: 101-103.
- Thimsen DA, Tong GK, Gruenberg JC (1989) Prospective evaluation of C-reactive protein in patients suspected to have acute appendicitis. Am Surg 55: 466-468.
- Bergeron E, Richer B, Gharib R, Giard A (1999) Appendicitis is a place for clinical judgement. Am J Surg 177: 460-462.
- Considine RV, Sinha MK, Heiman ML, Kriauciunas A, Stephens TW, et al. (1996) Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N Engl J Med 334: 292-295.
- Yegen B (2003) Infeksiyon ve inflamasyonda leptin. Genel Tip Dergisi 13:179-181.
- Kwok MY, Kim MK, Gorelick MH (2004) Evidence-based approach to the diagnosis of appendicitis in children. Pediatr Emerg Care 20: 690-698.
- Bundak R, Furman A, Gunoz H, Darendeliler F, Bas F, et al. (2006) Body mass index references for Turkish children. Acta Paediatr 95: 194-198.
- Stefanutti G, Ghirardo V, Gamba P (2007) Inflammatory markers for acute appendicitis in children: are they helpful? J Pediatr Surg 42: 773-776.
- Amalesh T, Shankar M, Shankar R (2004) CRP in acute appendicitis--is it a necessary investigation? Int J Surg 2: 88-89.
- Wu HP, Lin CY, Chang CF, Chang YJ, Huang CY (2005) Predictive value of C-reactive protein at different cutoff levels in acute appendicitis. Am J Emerg Med 23: 449-453.
- Porte D, Baskin DG, Schwartz MW (2002) Leptin and insulin action in the central nervous system. Nutr Rev 60: S20-S29.
- Fantuzzi G, Faggioni R (2000) Leptin in the regulation of immunity, inflammation, and hematopoiesis. J Leukoc Biol 68: 437-446.
- Faggioni R, Feingold KR, Grunfeld C (2001) Leptin regulation of the immune response and the immunodeficiency of malnutrition. FASEB J 15: 2565-2571.
- Means RT (1995) Pathogenesis of the anemia of chronic disease: a cytokine-mediated anemia. Stem Cells 13: 32-37.
- Clyne B, Olshaker JS (1999) The C-reactive protein. J Emerg Med 17: 1019-1025.
- Baumann H, Gauldie J (1994) The acute phase response. Immunology Today 15:81–88.
- Rosalki SB (2001) C-reactive protein. Int J Clin Pract 55: 269-270.
- Gualillo O, Eiras S, Lago F, Diéguez C, Casanueva FF (2000) Elevated serum leptin concentrations induced by experimental acute inflammation. Life Sciences 67: 2433-2341.
- Yavuz N, Unal E, Memisoglu K, Krand O, Kiziler AR, et al. (2004) Plasma leptin levels in rats with pancreatitis. Tohoku J Exp Med 204: 243-248.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11173
- [From(publication date):
October-2016 - Apr 17, 2025] - Breakdown by view type
- HTML page views : 10350
- PDF downloads : 823