Review Article Open Access
Amphetamines: Potent Recreational Drug of Abuse
Md. Sahab Uddin1*, Mohammad Abu Sufian1, Md. Tanvir Kabir2, Md. Farhad Hossain3, Md.Nasrullah1, Israt Islam4, Abdullah Al Mamun1, Md.Tanjir Islam1and Sayema Khanum1
1Department of Pharmacy, Southeast University, Dhaka, Bangladesh
2Department of Pharmacy, BRAC University, Dhaka, Bangladesh
3Department of Physical Therapy, Graduate School of Inje University, Gimhae, Korea
4Department of Pharmacy, State University of Bangladesh, Dhaka, Bangladesh
- *Corresponding Author:
- Md. Sahab Uddin
Department of Pharmacy, Southeast University
Dhaka, Bangladesh
Tel: +880 1710220110
E-mail: msu-neuropharma@hotmail.com
msu_neuropharma@hotmail.com
Received date: March 10, 2017; Accepted date: June 14, 2017; Published date: June 21, 2017
Citation: Uddin MS, Sufian MA, Kabir MT, Hossain MF, Nasrullah M, et al. (2017) Amphetamines: Potent Recreational Drug of Abuse. J Addict Res Ther 8:330. doi:10.4172/2155-6105.1000330
Copyright: © 2017 Uddin MS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Amphetamines are central nervous system (CNS) stimulants and belong to psychoactive drugs that affect chemicals in the brain, nerves and exert a constant contribution to hyperactivity and impulse control. The communal group of amphetamines comprises amphetamine, dextroamphetamine and methamphetamine. Amphetamines show its action on the mesolimbic dopaminergic reward system by inducing release of dopamine and to some extent norepinephrine, in the synaptic clefts of the nucleus accumbens and other terminal areas. They offer not only a sense of euphoric state, but also addiction. Amphetamines are frequently prescribed for the treatment of attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults, narcolepsy and obesity. At therapeutic doses, amphetamine causes emotional and cognitive effects such as euphoria, change in desire for sex, increased wakefulness, improved cognitive control, etc. The balance of benefit/risk is the main challenge for its clinical use. When overused these medications can be highly addictive, are often diverted from the user to be used as recreational drugs. Adverse effects include anxiety, aggression, headache, insomnia, hyperactivity, palpitations, increased breathing rate, increased blood pressure, tachycardia, arrhythmia, dilated pupils, paranoia, etc. However, at large doses, these drugs may impair cognitive function and induce rapid muscle breakdown. Even higher doses may give rise to hallucinations, paranoia, psychosis and potentially lifethreatening conditions such as convulsions, stroke, kidney failure, etc. The furthermost serious health implications of amphetamine resulting from chronic use are dependence, considered by compulsive drug-seeking and drug use and a phenomenon notorious as amphetamine psychosis. Therefore the objective of this study was to explore the functions of the amphetamines as recreation drug of abuse.
Keywords
Amphetamines; Psychoactive drug; Recreational drug; Abuse; Addiction
Abbreviations
CNS: Central nervous system; ADHD: Attention deficit hyperactivity disorder; US: United States; EU: European Union; 5-HT: Serotonin; MAO: Monoamine oxidase; VMAT: Vesicular monoamine transporter; DA: Dopamine; DAT: Dopamine transporter; CART: Cocaine and amphetamine regulated transcript; TAAR1: Trace amine-associated receptor 1; D: Dextrorotatory; L: Levorotary; PKA: Protein kinase A; PKC: Protein kinase C; ΔFosB: A member of the Fos family of transcription factors; FDA: Food and Drug Administration; DSM-IV-TR: Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision; DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th edition; APA: American Psychiatric Association; NF-κB: Nuclear factor kappa B; cAMP: Cyclic adenosine monophosphate; CREB: cAMP response element binding protein; G9a: A histone methyltransferase enzyme; ΔJunD: A transcription factor; c-Fos: A proto-oncogene; DDS: Dopamine dysregulation syndrome; PMA: p-Methoxyamphetamine; BDMPEA: 4-Bromo-2,5-dimethoxyphenethylamine; MDA: 3,4-Methylenedioxyamphetamine; MDMA: 3,4-Methylenedioxymethamphetamine; MDEA: 3,4-Methylenedioxy- N-ethylamphetamine; DOB: Dimethoxybromoamphetamine; DOM: 2,5-Dimethoxy-4-methylamphetamine; TMA: 3,4,5-Trimethoxyamphetamines; Cav1.2: Calcium channel, voltage-dependent, L type, alpha 1C subunit; NMDA: N-methyl-D-aspartate; AMPA: α-amino-3- hydroxy-5-methyl-4-isoxazolepropionic acid; DRD: Dopamine receptor D; CaM: Calmodulin; PP2B: Serine/threonine-protein phosphatase 2B; AC: Adenylyl cyclase; DARPP32: Dopamine- and cAMP-regulated neuronal phosphoprotein 32; PP1: Protein phosphatase 1; CAMKII: Calcium/calmodulin-dependent protein kinase II; GS: A G-protein; CREB: cAMP response element-binding protein; SIRT1: Sirtuin 1; HDAC1: Histone deacetylase 1; AADC: Aromatic L-amino acid decarboxylase.
Introduction
Amphetamines are potent CNS stimulant with sympathomimetic and adrenergic agonist activities [1]. This class of drugs was first synthesized in the late 19th century that includes amphetamine, dextroamphetamine and methamphetamine [2]. Although amphetamines had been available for research for many years, the first medical application of amphetamine was developed in the 1920s, when it’s CNS and respiratory stimulant properties were discovered [2]. Amphetamines have been used as a treatment for cold and sinus symptoms (the original inhalers contained Benzedrine, an amphetamine), obesity, narcolepsy (i.e., a disease in which the patient uncontrollably falls asleep) and paradoxically, ADHD. Amphetamines also have a high potential for abuse [3]. Soldiers on both sides during World War II used these drugs for their stimulant properties. After the war, amphetamine abuse reached epidemic proportions in Japan, Sweden and other parts of Europe, yet the drugs were not recognized as dangerous in the United States (US) until the 1960s [2]. Complications of amphetamine were first monitored by US physicians when they prescribed methamphetamine as a treatment for heroin addiction [2]. In case of 15 to 34 year old adults, lifetime prevalence of amphetamines use varies considerably between countries, from 0.1 to 12.4%, with a weighted European average of 5.5% [4]. The last year use of amphetamines in this age group ranges from 0 to 3.9%, with most countries reporting prevalence levels of 0.5 to 2.0%. It is estimated that approximately 1.7 million (i.e., 1.3%) young Europeans people have used amphetamine during the last year [5]. Study in the school going students aging between 15 to 16 years old, reported lifetime prevalence of amphetamine use ranged from 1 to 7% in the 24 European Union (EU) Member States and Norway. Countries like Belgium, Hungary also reported amphetamine prevalence levels of more than 4% [6].
It has been seen that single white men mainly addicted by amphetamine and its range high especially from 20 to 35 years [7]. Some research from rural populations showed that whites use amphetamine more than African Americans [8]. At present time women and other ethnic groups also addicted by amphetamine and this use become very common. Amphetamines stimulate the release of norepinephrine from central adrenergic receptors. It is reported that at high dose of amphetamine, dopamine can be secreted from the nigrostriatal and the mesocorticolimbic system [9]. Amphetamine may also act as a direct agonist on central 5-HT (i.e., serotonin) receptors and may inhibit monoamine oxidase (MAO) [10]. In the periphery, amphetamines are considered for the release of noradrenaline by acting on the adrenergic nerve terminals and α- and β-receptors [10]. Some pathways like serotonergic pathways may contribute to the calming effect. Amphetamine interacts with vesicular monoamine transporter (VMAT) enzymes to enhance release of non-exocytotic release of dopamine (DA) and 5-HT from vesicles [11,12].
Amphetamine is responsible for various complications like hypertension and tachycardia by its CNS stimulating action with feelings of increased confidence, sociability and energy [13]. It suppresses appetite and fatigue as well as leads to insomnia. Following oral use, the effects usually start within 30 min and last for many hours [13]. Amphetamine users may feel distressful conditions like irritable, restless, anxious and depression. This drug increases the activities of noradrenaline and dopamine neurotransmitter systems [14]. Amphetamine is less potent than methamphetamine, but in uncontrolled situations the effects are almost indistinguishable. After oral administration amphetamine is rapidly absorbed. Plasma levels of amphetamine may rise to maximum, 0.02 mg/L after a single oral dose of 10 mg [15]. The plasma half-life varies from 4 to 12 h and is dependent on the urinary pH (i.e., alkaline urine decreases the rate of elimination) [15].
The study showed that at normal therapeutic doses, the physical side effects of amphetamine vary by age and from people to people [16]. Some cardiovascular side effects include hypertension, Raynaud’s phenomenon (i.e., reduced blood flow to extremities) and tachycardia (i.e., increased heart rate) [17]. Men may affected by sexual side effects including erectile dysfunction, frequent erections, or prolonged erections. Abdominal side effects may include abdominal pain, loss of appetite, weight loss, nausea, etc. [18]. Blurred vision, dry mouth, excessive grinding of the teeth, rhinitis medicamentosa (i.e., druginduced nasal congestion), reduced seizure threshold, etc. are some other potential side effects [19]. Dangerous physical side effects are rare at typical pharmaceutical doses [20]. The therapeutic doses of amphetamine can include following psychological effects: increased alertness, apprehension, concentration, decreased sense of fatigue, mood swings (i.e., elated mood followed by mildly depressed mood), increased initiative, insomnia or wakefulness, self-confidence and sociability [20]. Other than these patients also suffer some other less common effects such as, anxiety, change in libido, grandiosity, irritability, repetitive or obsessive behaviors and restlessness [21]. Amphetamine psychosis can occur if patients use heavy doses of amphetamine [22]. Even though very rare, this psychosis may occur in case of long-term uses of therapeutic doses [23,24].
Amphetamine overdose can lead to a number of symptoms [25]. Overdose symptoms increase with dosage of amphetamine and decreases with tolerance to amphetamine [25,26]. Patient who is tolerant can consume approximately 5 g of amphetamine per day, which may lead to state like coma [24]. A research data showed that due to overdose of amphetamine, [18] more than 3,788 patients died worldwide in 2003 (i.e., 3,425-4,145 deaths, 95% confidence) [27]. Therefore, the purpose of this study was to show the potentiality of the amphetamines as drug of abuse.
History of Amphetamine
Amphetamine was synthesized at first in Germany in 1887 by Romanian chemist Laz?r Edeleanu who named it phenylisopropylamine; the excitatory effect of its remained unknown until 1927, when it was independently resynthesized by Gordon Alles and claimed it’s sympathomimetic properties [28]. In the early 1930s, when amphetamine’s CNS and respiratory stimulant effects were discovered, it was commercialized as an inhaler for nasal congestion (i.e., Benzedrine©) [29]. Meanwhile, it was also suggested by the health practitioners as a cure for a range of ailments like alcohol hangover, narcolepsy, depression, weight reduction, hyperactivity in children and vomiting associated with pregnancy. Furthermore, the use of amphetamine grew rapidly because of its easy abundance, cheap price, long lasting effects and good appreciation from the physicians as an addiction risk medicament [29]. Whilst, amphetamine and its methamphetamine derivatives were also introduced and became available as oral and intravenous formulations for therapeutic purposes. At the time of World War II to boost up alertness and endurance and to improve mood amphetamine was hugely utilized by the military of the US Great Britain, Germany and Japan [10,30]. But during the 1960s and 1970s abuse began with the discovery of its euphoric effects upon intravenous injection of methamphetamine with a more rapid onset than oral administration. Being structurally similar, methamphetamine has more prominence action on the CNS compared to amphetamine [31].
In the early 1970s according to the Controlled Substances Act of the US, amphetamine was claimed as a schedule II controlled substance owing to aforementioned health hazard effects [32]. But despite strict government controls, amphetamine has been frequently used legally or illicitly by people, mainly musicians, mathematicians, authors and athletes [33-35].
Chemistry of Amphetamine
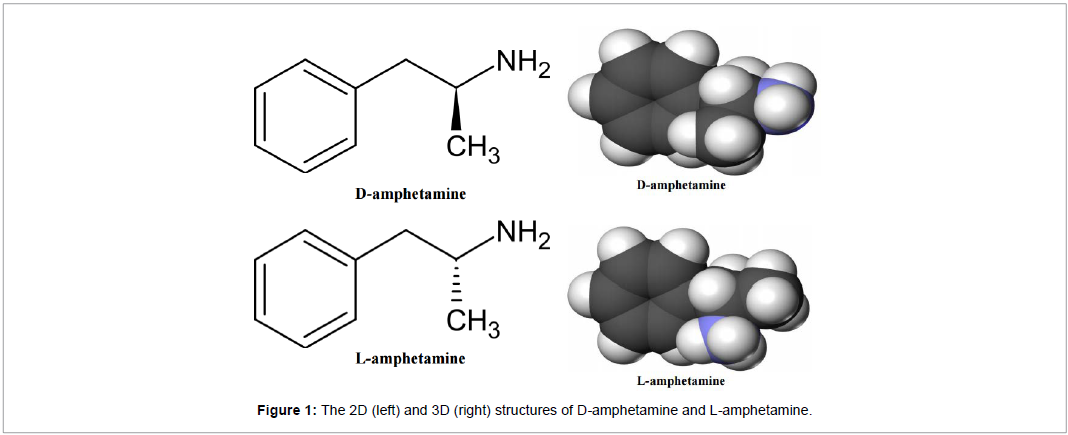
The 2D and 3D structure of D-amphetamine and L-amphetamine are presented in Figure 1. The chemical formula of amphetamine is C9H13N. It is a methyl homolog of the mammalian neurotransmitter phenethylamine. The carbon atom adjacent to the primary amine has a stereogenic center and actually it is composed of a racemic mixture (1:1) of two enantiomeric mirror images. This racemic mixture can be separated into its optical isomers: D-amphetamine and L-amphetamine [10]. The pure free base of amphetamine is volatile, colorless with a characteristically strong amine odor and acrid burning taste at room temperature [36]. The salts form of amphetamine comprises amphetamine aspartate, hydrochloride, phosphate, saccharate, sulfate, etc. [15]. Amphetamine is also the parent compound of its own structural class, which contains various psychoactive derivatives as well as admirable chiral ligand for the stereo-selective synthesis [37,38].
Mechanism of action of amphetamine
Amphetamine mainly works by increasing the action of the neurotransmitters dopamine and norepinephrine in the brain [39,40]. It also initiates the release of various other hormones (e.g. epinephrine) and neurotransmitters (e.g. serotonin and histamine) as well as the biosynthesis of particular neuropeptides (e.g. cocaine and amphetamine regulated transcript [CART] peptides) [36]. In case of Adderall both active ingredients such as D-amphetamine and L-amphetamine, bind to the same receptor, their binding affinities might vary. D-amphetamine and L-amphetamine are both potent agonists of trace amine-associated receptor 1 (TAAR1) and react with VMAT2, with D-amphetamine being the more effective agonist of TAAR1 [20,41]. Whereas, D-amphetamine generates more CNS stimulation than L-amphetamine; however, L-amphetamine has merely greater cardiovascular and peripheral action [42]. It has been noticed that certain children have a better clinical response to L-amphetamine [43].
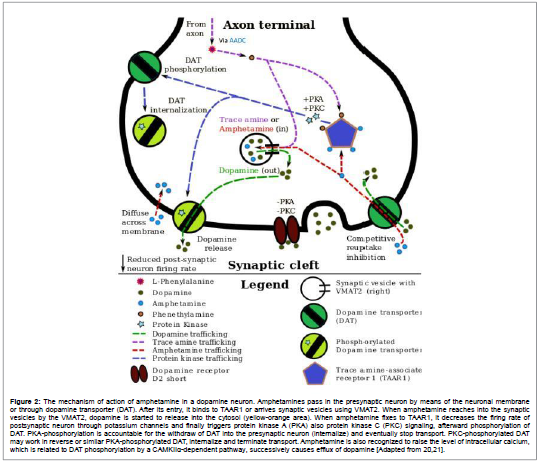
Usually VMAT2 do the task of transporting the monoamine (e.g. dopamine, histamine, serotonin, norepinephrine, etc.) from the intracellular fluid to the synaptic vesicles (i.e., chemical storage units inside a neuron) of neuron in the absence of amphetamine [44]. Upon entry of amphetamine into neuron and interaction with VMAT2, the transporter reverses its approach of transport, which intern release stored monoamines inside synaptic vesicles back into the neuron’s intracellular fluid (Figure 2) [44]. At that time activation of TAAR1 by amphetamine, the receptor induces the neuron’s cell membranebound monoamine transporters (like the dopamine transporter, norepinephrine transporter, or serotonin transporter) to either stop transporting monoamines altogether via transporter internalization or transport monoamines out of the neuron [45]. In other words, the reversed membrane transporter will expel dopamine, norepinephrine and serotonin out of the neuron’s intracellular fluid and into the synaptic cleft [45]. At the end, upon interaction with VMAT2 and TAAR1, amphetamine initiates neurotransmitter release from the synaptic vesicles initiated by VMAT2 into the intracellular fluid where they subsequently eliminate the neuron with the help of membranebound, reversed monoamine transporters initiated by TAAR1 [45].
Figure 2: The mechanism of action of amphetamine in a dopamine neuron. Amphetamines pass in the presynaptic neuron by means of the neuronal membrane or through dopamine transporter (DAT). After its entry, it binds to TAAR1 or arrives synaptic vesicles using VMAT2. When amphetamine reaches into the synaptic vesicles by the VMAT2, dopamine is started to release into the cytosol (yellow-orange area). When amphetamine fixes to TAAR1, it decreases the firing rate of postsynaptic neuron through potassium channels and finally triggers protein kinase A (PKA) also protein kinase C (PKC) signaling, afterward phosphorylation of DAT. PKA-phosphorylation is accountable for the withdraw of DAT into the presynaptic neuron (internalize) and eventually stop transport. PKC-phosphorylated DAT may work in reverse or similar PKA-phosphorylated DAT, internalize and terminate transport. Amphetamine is also recognized to raise the level of intracellular calcium, which is related to DAT phosphorylation by a CAMKIIa-dependent pathway, successively causes efflux of dopamine [Adapted from 20,21].
Side effects of amphetamine
The side effects of amphetamine are diverse and the amount of amphetamine used is the primary factor in determining the likelihood and severity of side effects [20]. Amphetamine products such as Adderall, Dexedrine, and their generic equivalents are currently approved by the Food and Drug Administration (FDA) for long-term therapeutic use [24,46]. Recreational use of amphetamine generally involves much larger doses, which have a greater risk of serious side effects than the dosages used for therapeutic reasons [20]. The physical and psychological side effects of amphetamine are:
Physical side effects: Amphetamine stimulates the medullary respiratory centers, producing faster and deeper breaths (Table 1) [20]. In a normal person at therapeutic doses, this effect is usually not noticeable, but when respiration is already compromised, it may be evident [20]. Amphetamine also induces contraction in the urinary bladder sphincter, the muscle which controls urination, which can result in difficulty urinating [20]. This effect can be useful in treating bed wetting and loss of bladder control [20]. The effects of amphetamine on the gastrointestinal tract are unpredictable [20]. If intestinal activity is high, amphetamine may reduce gastrointestinal motility (i.e., the rate at which content moves through the digestive system); [20] however, amphetamine may increase motility when the smooth muscle of the tract is relaxed [20]. Amphetamine also has a slight analgesic effect and can enhance the pain relieving effects of opioids [20].
| Short-Term Side Effects | Long-Term Side Effects |
|---|---|
| High body temperature | Toxic psychosis |
| Cardiovascular system failure | Physiological and behavioral disorders |
| Hostility or paranoia | Dizziness |
| Irregular or increased heart rate/heart beat | Pounding heartbeat |
| Increased diastolic/systolic blood pressure | Difficulty breathing |
| Increased activity/talkativeness | Mood or mental changes |
| Euphoria | Unusual tiredness or weakness |
| Heightened sense of well-being | Cardiac arrhythmias |
| Decreased fatigue/drowsiness | Repetitive motor activity |
| Decreased appetite | Convulsions, coma and death |
| Dry mouth | Ulcers |
| Dilated pupils | Malnutrition |
| Increased respiration | Mental illness |
| Heightened alertness/energy | Skin disorders |
| Nausea | Vitamin deficiency |
| Headache | Flush or pale skin |
| Palpitations | Loss of coordination and physical collapse |
| Altered sexual behavior | |
| Tremor/twitching of small muscles | |
| Release of social inhibitions | |
| Unrealistic feelings of cleverness, great competence and power |
Table 1: Short-term and long-term side effects of amphetamine [51].
FDA-commissioned studies from 2011 indicate that in children, young adults and adults, there is no association between serious adverse cardiovascular events (i.e., sudden death, heart attack and stroke) and the medical use of amphetamine or other ADHD stimulants [47,48]. However, amphetamine pharmaceuticals are contraindicated in individuals with cardiovascular disease [49].
Psychological side effects: At normal therapeutic doses, the most common and less common psychological side effects of amphetamine are stated earlier (Table 1) [20]. Amphetamine psychosis (e.g. delusions and paranoia) can occur in heavy users [22]. Although very rare, this psychosis can also occur at therapeutic doses during long-term therapy [23]. According to the FDA, “there is no systematic evidence” that stimulants produce aggressive behavior or hostility [24]. Amphetamine has also been shown to produce a conditioned place preference in humans taking therapeutic doses, [50] meaning that individuals acquire a preference for spending time in places where they have previously used amphetamine [39].
Amphetamine overdose
As the doses of amphetamine increases, there is risk of developing impaired cognitive function and induce rhabdomyolysis (Table 2). Although there is a perceived risk of drug addiction along with amphetamine use, however, it is unlikely to happen for typical longterm medical uses at therapeutic doses [51]. Recreational amphetamine use often involves much higher doses than therapeutic doses, which involves risk of adverse drug reactions, including psychosis (e.g. hallucinations and neurosis) [52,53].
| Body System | Minor or Moderate Overdose | Severe Overdose |
|---|---|---|
| Central nervous | • Confusion | • Acute amphetamine psychosis (e.g., delusions and paranoia) |
| • Abnormally fast reflexes | • Compulsive and repetitive movement | |
| • Severe agitation | • Serotonin syndrome (i.e., excessive serotonergic nerve activity) | |
| • Tremor (involuntary muscle twitching) | • Sympathomimetic toxidrome (i.e., excessive adrenergic nerve activity) | |
| Cardiovascular | • Abnormal heartbeat | • Cardiogenic shock (i.e., heart not pumping enough blood) |
| • High or low blood pressure | • Cerebral hemorrhage (i.e., bleeding in the brain) | |
| • Circulatory collapse (i.e., partial or complete failure of the circulatory system) | ||
| Respiratory | • Rapid breathing | • Pulmonary edema (i.e., fluid accumulation in the lungs) |
| • Pulmonary hypertension (i.e., high blood pressure in the arteries of the lung) | ||
| • Respiratory alkalosis (i.e., reduced blood carbondioxide) | ||
| Musculoskeletal | • Muscle pain | • Rhabdomyolysis (i.e., rapid muscle breakdown) |
| Urinary | • Painful urination | • No urine production |
| • Urinary retention | • Kidney failure | |
| Other | • Elevated body temperature | • Elevated or low blood potassium |
| • Mydriasis (i.e., dilated pupils) | • Hyperpyrexia (i.e., extremely elevated core body temperature) | |
| • Metabolic acidosis (i.e., excessively acidic bodily fluids) |
Table 2: Clinical manifestations of amphetamine overdose [20,24,26,62,63].
In amphetamine addiction, an excessive pathological activation of the mesolimbic pathway (a dopamine pathway that connects the ventral tegmental area to the nucleus accumbens) is found to play critical role [54,55]. Accumbal ΔFosB is recognized as “molecular switch” and considered as the “master control protein” for addiction. Regular recreational users often overdose themselves with amphetamines, as a result accumbal ΔFosB level slowly increases [56,57]. Consequently, induction of nucleus accumbens ΔFosB takes place which in turn trigger addictive behaviors like compulsive desire to take the drug. Still there is no effective therapeutic agent available which can treat addiction of amphetamine [58,59]. However, regular involvement with sustained aerobic exercises are found to not only lessen the development of amphetamine addiction, but also effective in the treatment of amphetamine addiction [60]. It has also been found that clinical treatment outcomes can be enhanced by exercise therapy and can also be incorporated with cognitive behavioral therapy, currently this combination therapy is considered as the best clinical treatment [39,61].
Amphetamine addiction and dependence
The acute reinforcing effects of amphetamine lead to patterns of drug use that, in epigenetically vulnerable individuals, result eventually in addiction, a state hypothesized to be the result of plastic changes in multiple neural circuits [64]. The types of plasticity that underlie addiction can be divided conceptually into three groups: compensatory adaptations in neural systems that regulate autonomic and other somatic functions leading to physical dependence and withdrawal; adaptations in the mesoaccumbens brain reward circuitry itself resulting in the emotional and motivational aspects of dependence and withdrawal; plasticity involving both the mesoaccumbens circuitry and other limbic circuits yielding sensitization and cue-dependent, positively biased emotional memories of drug use that may predispose to relapse. Unlike the opiates and ethanol, amphetamine does not produce physical dependence; they are nonetheless among the most reinforcing and addictive drugs known, underscoring the importance of plasticity in emotional circuits [64].
It may not possible to recognize the signs of amphetamine addiction at first, but as the addiction progresses and the effects of amphetamine use set in, the signs of addiction become more and more evident [65]. Some of the early signs of addiction are tolerance and physical dependence or an urge to use amphetamines (Table 3) [65].
| Signs of Amphetamine Addiction |
|---|
| •Compulsive use of amphetamines |
| •Using amphetamines to feel good |
| •Lack of personal appearance or ill desire to take care of one’s self |
| •Taking amphetamines to cope with everyday activities |
| •Using amphetamines to socially interact |
| •Lack of pleasure when not taking amphetamines |
| •Taking amphetamines despite problems in a relationship or with loved ones |
| •Taking amphetamines despite the known consequences of taking the drugs |
| •Withdrawal symptoms when not taking amphetamines |
Table 3: The signs of amphetamine addiction [65].
As mentioned previously that amphetamines are used to medically treat such disorders as narcolepsy and ADHD [66]. Amphetamines may be illegally obtained and abused for the euphoric effects. When abused there are a number of side effects that can occur. The side effects experienced depend upon the individual and the amount of time the substance has been used. Some of the symptoms of amphetamine abuse are presented in Tables 4 and 5 [67,68].
| Most Common Symptoms | Less Desirable Symptoms |
|---|---|
| •Increased body temperature | •Hostility |
| •Euphoria | •Paranoia |
| •Increased blood pressure | •Aggressiveness |
| •Dry mouth | •Cardiovascular system failure |
| •Faster breathing | •Irregular heart beat |
| •Dilated pupils | •Nausea |
| •Increased energy and alertness | •Headache |
| •Decreased fatigue | •Reduction of social inhibitions |
| •Decreased appetite | •Altered sexual behavior |
| •Blurred vision | |
| •Chest pain | |
| •Hallucinations | |
| •Unrealistic ideas of personal ability and power | |
| •Convulsions | |
| •Malnutrition | |
| •Skin disorders | |
| •Amphetamine-induced psychosis |
Table 4: Symptoms of amphetamine abuse [67].
| Mood Symptoms | Behavioral Symptoms | Physical Symptoms | Psychological Symptoms |
|---|---|---|---|
| •Euphoria | •Hostility | •Increased body temperature | •Paranoia |
| •Increased alertness | •Aggressiveness | •Increased blood pressure | •Psychosis |
| •Irritability | •Altered sexual behavior | •Dilated pupils | •Hallucinations |
| •Mood swings | •Not sleeping for prolonged period of time | •Faster breathing | •Clear and focused feeling |
| •Depression | •Not eating for prolonged period of time | •Decreased fatigue | |
| •Anxiety | •Unrealistic ideas of personal ability and power | •Dry mouth | |
| •Fast and excessive talking | •Decreased appetite | ||
| •Grinding of teeth | •Nausea | ||
| •Increased confidence | •Headache | ||
| •Irregular heart beat | |||
| •Malnutrition | |||
| •Blurred vision |
Table 5: Mood, behavioral, physical and psychological symptoms of amphetamine abuse [68].
According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, text revision (DSM-IV-TR) and Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5); manual of the American Psychiatric Association (APA) diagnostic features of amphetamine use disorder is listed in Table 6 [69,70]. Consistent with DSM-5, it is necessary to specify the current severity: mild (presence of 2-3 symptoms), moderate (4-5 symptoms) or severe (6 or more symptoms) [70].
| DSM-IV-TR and DSM-5 Diagnosis Scheme of Amphetamine Use Disorder |
|---|
| A problematic pattern of amphetamine use leading to clinically significant impairment or distress, as manifested by 2 or more (as specified in DSM-5) or at least 3 (as specified in the DSM-IV-TR) of the following, occurring within a 12 month period: |
| 1.Amphetamine is often taken in larger amounts or over a longer period than was intended. |
| 2.A persistent desire or failed efforts to reduce or control amphetamine use. |
| 3.A great deal of time is spent in activities necessary to obtain the amphetamine, use the amphetamine, or recover from its effects. |
| 4.Craving or a strong desire or urge to use the amphetamine. |
| 5.Recurrent amphetamine use that results in a failure to fulfill major role obligations at work, school, or home. |
| 6.Continued amphetamine use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of amphetamine. |
| 7.Important social, occupational, or recreational activities are given up or reduced because of amphetamine use. |
| 8.Recurrent amphetamine use when it is physically hazardous. |
| 9.Amphetamine use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the amphetamine. |
| 10.Amphetamine tolerance, as defined by either of the following: |
| -A need for markedly increased amounts of the amphetamine to achieve intoxication or desired effect. |
| -A markedly diminished effect with continued use of the same amount of the amphetamine. |
| 11 The characteristic withdrawal syndrome for the amphetamine as manifested by the following: |
| •Cessation of (or reduction in) prolonged amphetamine-type substance, cocaine, or other stimulant use. |
| •Dysphoric mood and two or more of the following physiological changes, developing within a few hours to several days after the cessation of (or reduction in) amphetamine use: |
| -Fatigue; |
| -Vivid, unpleasant dreams; |
| -Insomnia or hypersomnia; |
| -Increased appetite; |
| •Psychomotor retardation or agitation. |
| •The amphetamine or closely related substance is taken to relieve or avoid withdrawal symptoms. |
Table 6: DSM-IV-TR and DSM-5 diagnosis criteria of amphetamine use disorder [69,70].
Although there is a substantial risk of developing addiction with larger doses of amphetamine, however this is unlikely to happen with typical long-term therapeutic uses [71]. On the other hand, drug tolerance is likely to take place with regular abuse of amphetamine, henceforth eventually larger doses of amphetamine will be needed to get the same effect [72] (Table 7).
| DSM-IV-TR Diagnosis Scheme of Amphetamine Dependence |
|---|
| 1.Amphetamine dependence is defined as a maladaptive pattern of use that results in significant impairment or distress, as shown by the following features occurring within a 12 month period: |
| Tolerance for the amphetamine, as shown by either |
| The need for increased amounts of the amphetamine to achieve the desired effect or intoxication, or |
| Marked reduction in the effects of continuing to ingest the same amounts. |
| 2.Withdrawal symptoms, as shown by either |
| The withdrawal syndrome that is considered characteristic for the amphetamine , or |
| The taking of the same substance (or a closely related substance, as when methadone is substituted for heroin) to relieve or to prevent withdrawal symptoms. |
| 3.Taking larger amounts of the amphetamine or for longer periods of time than the individual intended (e.g., person had desired to take only one drink, but after taking the first, continues drinking until severely intoxicated). |
| 4.Persistent desire to cut down or control intake of amphetamine or lack of success in trying to exercise self-control. |
| 5.Spending a good deal of time in activities directed toward obtaining the amphetamine (e.g., visiting several physicians to obtain prescriptions or engaging in theft), in actually ingesting the amphetamine, or in recovering from its use. In severe cases, the individual’s daily life revolves around amphetamine use. |
| 6.The individual has reduced or given up important social, occupational, or recreational activities due to amphetamine use (e.g., person withdraws from family events in order to indulge in drug use). |
| 7.Amphetamine use is continued despite evidence of persistent or recurrent psychological or physical problems either caused or exacerbated by its use (e.g., repeated arrests for driving while intoxicated). |
Table 7: DSM-IV-TR diagnosis criteria of amphetamine dependence [69].
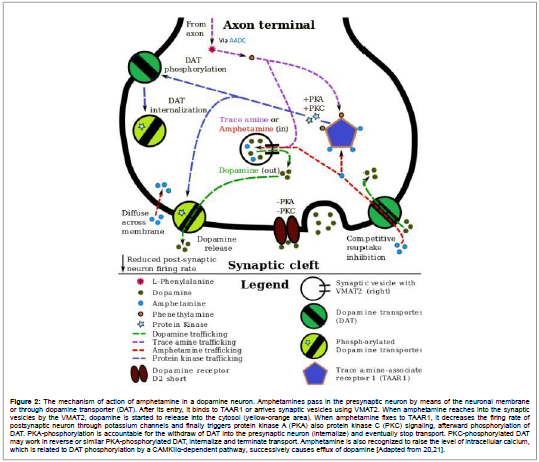
Nucleus accumbens is the particular portion of the brain where altered gene expression takes place due to long-term use of amphetamine [73]. Nuclear factor kappa B (NF-κB), ΔFosB and cAMP response element binding protein (CREB) are the noteworthy transcription factors which are found to induce these alterations (Figure 3) [57]. Among these transcription factors, ΔFosB plays critical role in the development of drug addiction. The reason behind this pivotal role is due to the neural and behavioral adaptations that takes place due to the involvement of adequate ΔFosB overexpression in D1-type medium spiny neurons in the nucleus accumbens. An increment in the ΔFosB expression is found to be associated with the ΔFosB induced addictive state which is primarily due to the adequate ΔFosB overexpression. Similar conditions are seen in addictions like methylphenidate, substituted amphetamines, alcohol, cocaine, propofol, nicotine, cannabinoids, phencyclidine, etc. [74].
Figure 3: Signaling cascade in the nucleus accumbens of brain’s reward center that lead to amphetamine addiction. Co-release of presynaptic dopamine and glutamate through psychostimulants (i.e., amphetamine), post-synaptic receptors for these neurotransmitters cause internal signaling events by a cAMP pathway then calciumdependent path that finally increased the phosphorylation of CREB. Phosphorylated CREB raises the level of ΔFosB that represses the c-Fos gene by means of co-repressors, c-Fos repression that serves as a molecular switch which enables the accumulation of ΔFosB in the neuron. Phosphorylated ΔFosB once persists in neurons for the period of one or two months, gradually accumulates following repeated high-dose exposure to stimulants through this process. ΔFosB operates is liable for addiction-related structural changes in the brain and afterward sufficient accrual, using its downstream targets (e.g. NF-κB), it encourages an addictive state [Adapted from 20,21].
A transcription factor, ΔJunD and a histone methyltransferase enzyme, G9a are seen to be directly opposing the inductions of ΔFosB in the nucleus accumbens (i.e., they confine increases in its expression) [75]. Sufficient overexpression of ΔJunD in the nucleus accumbens with viral vectors can entirely block many of the chronic drug abuse associated with behavioral and neural alterations (i.e., the alterations mediated by ΔFosB). ΔFosB also have significant functions in the regulation of behavioral responses to natural rewards including exercise, sex and palatable food. As these addictive drugs and natural rewards can induce expression of ΔFosB (i.e., they cause the brain to produce more of it), thus, long-term acquisition of these natural rewards can lead to similar pathological state of addiction. Therefore, ΔFosB is considered as one of the most significant factors found to be involved in both addiction of amphetamine and compulsive sex addictions induced by amphetamine [76,77]. These sex addictions are linked with a dopamine dysregulation syndrome (DDS) which arises in some patients who are taking dopaminergic drugs [78].
| Time Since Last Amphetamine Use | Amphetamine Withdrawal Symptoms |
|---|---|
| 1-3 Days | Comedown: |
| Exhaustion | |
| Increased Sleep | |
| Depression | |
| 2-10 Days | Withdrawal: |
| Strong urges (i.e., cravings) to use amphetamines | |
| Mood swings (i.e., feeling anxious, irritable or agitated or feeling flat and lacking energy) | |
| Poor sleep | |
| Poor concentration | |
| General aches and pains, headaches | |
| Increased appetite (very hungry) | |
| Strange thoughts | |
| Misunderstanding things around surrounding (e.g., seeing things that aren’t there) | |
| 7-28 Days | Most symptoms start to settle down, although common symptoms include: |
| Mood swings (i.e., feeling anxious, irritable or agitated or feeling flat and lacking energy) | |
| Poor sleep | |
| Cravings | |
| 1-3 Months | Return of normal sleep and levels of activity and mood |
| Major improvements in general health and mood |
Table 8: Common symptoms associated with amphetamine withdrawal [81].
Dose and route of administration largely determine the amphetamine effects on the regulation of gene. Most of the studies on addiction and gene regulation are based on intravenous administration of large doses of amphetamine in animal models. These studies confirmed that therapeutic uses of amphetamine do not significantly alter gene regulation [73].
Amphetamine dependence generally indicates that addiction has occurred and the user does not feel “normal” without the drug [79]. This dependence is associated with a range of physical and mental health problems. As stated by the DSM-IV-TR, in the diagnostic features of amphetamine dependence are presented [69].
Amphetamine withdrawal
Withdrawal is this period of readjustment [80]. Amphetamine dependence is also characterized by withdrawal symptoms, once the drug usage is stopped. Some of the common withdrawal symptoms are offered in Table 8 [81].
A previous study on people who used amphetamine and methamphetamine compulsively, reported that abrupt cessation of amphetamine use in the chronic heavy users may lead to time-limited withdrawal syndrome that may take place as early as 24 h of their last dose [82]. This study also concluded that as high as 87.6% of the cases withdrawal symptoms are most commonly seen amongst the chronic users who use amphetamine in larger doses on regular basis [82]. Symptoms of amphetamine withdrawal may include drowsiness, lack of motivation, anxiety, depression, craving for amphetamine, increased appetite, fatigue, hypoactivity or hyperactivity and lucid dreams [82]. This study also indicated that the extents of withdrawal symptoms are directly related to the degree of dependence and these symptoms are less likely to take place along with the therapeutic doses and uses [82]. Unfortunately, often manufacturer prescribing information does not indicate the risk of developing withdrawal symptoms following discontinuation of amphetamine use even after an extended period at therapeutic doses [46].
Amphetamine tolerance
The first signs of amphetamine addiction tend to be tolerance. Tolerance is the reaction that the body has been given a drug repeatedly [65]. Over time, sometimes faster if taken with other drugs, the body will have less of a reaction to the drug and the user will have to take more of the drug in order to feel the same effects [83]. As tolerance builds, the user will no longer feel the same effects of amphetamines and may resort to using more or to using the drugs more often [65].
Regular amphetamine use can quickly lead to tolerance of the drug. Though tolerance does build rapidly, taking a break from the drug use can quickly cause the tolerance to diminish [65,84]. Unfortunately, this is one of the greatest dangers associated with amphetamine addiction treatment; users who stop taking amphetamines for a period of time have a lowered tolerance and when they relapse are more likely to overdose because they think that they can return to previous patterns of drug abuse which could prove to be too much for their newly reduced levels of tolerance [65].
Tolerance is also expected to develop with regular substituted amphetamine use [85]. When substituted amphetamines are abused, drug tolerance develops rapidly [72].
Toxicity of amphetamine and associated psychosis
Toxic central effects of amphetamine use include psychosis, hyperthermia, seizures and rhabdomyolysis, while cardiovascular toxicity includes ventricular arrhythmias, acute myocardial infarction and cardiomyopathies [86]. Neurotoxicity refers to neurological changes that persist after cessation of use and evidence suggests that chronic methamphetamine use leads to dopamine depletion and possibly also changes in serotonergic function [87]. Amphetamine toxicity produces a wide range of clinical effects displayed in Table 9 [62].
| Clinical Signs Indicating Amphetamine Toxicity |
|---|
| •Seizure |
| •Focal neurological deficit |
| •Reduced level of consciousness |
| •Abnormal motor movements |
| •Hyperthermia |
| •Dysrhythmias |
| •Hypotension |
| •Hypertension |
| •Coronary artery spasm and related sequelae |
| •Autonomic instability and other major disturbance of homeostasis |
Table 9: Clinical signs representative significant amphetamine toxicity[62].
There is overwhelming evidence that patients with psychotic disorders have an increased vulnerability to compulsive use of drugs of abuse [88], including psycho stimulants like amphetamines [89]. The DSM-5 describes the following amphetamine-related psychiatric disorders represented in Table 10 [70]. The symptoms of psychosis induced by amphetamines are very similar to those of acute schizophrenia spectrum psychosis and include: lack of concentration, delusions of persecution, increased motor activity, disorganization of thoughts, lack of insight, anxiety, suspicion and auditory hallucinations [90,91]. Some studies have suggested differences with more pronounced grandiosity and visual hallucinations [92].
| Amphetamine-Related Psychiatric Disorders |
|---|
| •Amphetamine-induced anxiety disorder |
| •Amphetamine-induced bipolar disorder |
| •Amphetamine-induced psychotic disorder with delusions |
| •Amphetamine-induced psychotic disorder with hallucinations |
| •Amphetamine-induced sexual dysfunction |
| •Amphetamine-induced sleep disorder |
| •Amphetamine intoxication |
| •Amphetamine intoxication delirium |
| •Amphetamine withdrawal |
| •Amphetamine-induced obsessive-compulsive and related disorders |
| •Unspecified amphetamine -related disorder |
Table 10: Psychiatric disorders associated with amphetamine [70].
There may be several explanations for this increased comorbidity, but there is convincing evidence from animal studies that this may be due to shared vulnerabilities for both psychosis and drug use disorders [93]. These animal studies also point to possible neural mechanisms explaining the increased comorbidity [94]. In rodents and primates, sufficiently high doses of amphetamine cause dopaminergic neurotoxicity, or damage to dopamine neurons, this is characterized by dopamine terminal degeneration and reduced transporter and receptor function [20,95]. There is no evidence that amphetamine is directly neurotoxic in humans [39]. However, large doses of amphetamine may indirectly cause dopaminergic neurotoxicity as a result of hyperpyrexia, the excessive formation of reactive oxygen species and increased autoxidation of dopamine [20,96]. Animal models of neurotoxicity from high-dose amphetamine exposure indicate that the occurrence of hyperpyrexia (i.e., core body temperature ≥ 40°C) is necessary for the development of amphetamine-induced neurotoxicity [97]. Prolonged elevations of brain temperature above 40°C likely promote the development of amphetamine-induced neurotoxicity in laboratory animals by facilitating the production of reactive oxygen species, disrupting cellular protein function and transiently increasing blood-brain barrier permeability [20,97].
A severe amphetamine overdose can result in a stimulant psychosis that may involve a variety of symptoms, such as delusions and paranoia [20,22]. A previous report on treatment for amphetamine, dextroamphetamine and methamphetamine psychosis states that about 5 to 15% of users fail to recover completely [20,98]. According to the same review, there is at least one trial that shows antipsychotic medications effectively resolve the symptoms of acute amphetamine psychosis [20,22]. Psychosis very rarely arises from therapeutic use [24].
Pharmaceutical products of amphetamine
Commonly prescribed amphetamine preparations like Adderall, Evekeo, Dyanavel XR, contain both the enantiomers. Among them Evekeo is the racemic amphetamine sulfate [99]. Amphetamine is also available in the form of enantiopure and prodrug as dextroamphetamine and lisdexamfetamine correspondingly [46,100]. The prodrug form, lisdexamfetamine is structurally different from amphetamine and remains inactive until it is metabolized into dextroamphetamine [101]. Benzedrine, Sympatedrine and Psychedrine are the previously available free base of racemic amphetamine. On the other hand, Cydril is the previously available form of levoamphetamine. Most of the current amphetamine preparations are available in the salt form rather than the free base form, due to the high volatility of the free bases [1]. Nevertheless, dosage forms like oral suspension and orally disintegrating tablet were introduced in the market in 2015 and 2016, respectively [102]. Some of the current brands and their generic equivalents are listed in Table 11 [102-104].
|
Brand Name |
United States Adopted Name |
(D:L) Ratio |
Dosage Form |
Marketing Start Date |
|---|---|---|---|---|
| Adderall | - | 3:1 (Salts) | Tablet | 1996 |
| Adderall XR | - | 3:1 (Salts) | Capsule | 2001 |
| Adzenys XR | Amphetamine | 3:1 (Base) | Orodispersible tablet | 2016 |
| Dyanavel XR | Amphetamine | 3.2:1 (Base) | Suspension | 2015 |
| Evekeo | Amphetamine sulfate | 1:1 (Salts) | Tablet | 2012 |
| Dexedrine | Dextroamphetamine sulfate | 1:0 (Salts) | Capsule | 1976 |
| ProCentra | Dextroamphetamine sulfate | 1:0 (Salts) | Liquid | 2010 |
| Zenzedi | Dextroamphetamine sulfate | 1:0 (Salts) | Tablet | 2013 |
| Vyvanse | Lisdexamfetamine dimesylate | 1:0 (Prodrug) | Capsule/Tablet | 2007 |
Table 11: Commercially available pharmaceutical products of amphetamines [1,20,100].
Regulatory status of amphetamine in society and culture
From the 1960s onward, amphetamine has been popular with many youth cultures in Britain and other parts of the world as a recreational drug [103]. It has been commonly used by novelists, mathematicians, film procurer and punks, gangsters and casuals in all night soul and ska dances, punk concerts, basement shows, etc. In Table 12, slang names of frequently abused amphetamines and substituted amphetamines are presented [62]. As a consequence of potential abuse, distribution of amphetamines and their analogues are controlled by the respective authorities.
| Amphetamines and Substituted Amphetamines | Slang Names |
|---|---|
| Amphetamine | Amp, Bennies, Black beauties, Browns, Cranks, Fives, Goey, Hearts, Louee, Speed, Uppers, Whiz |
| Methamphetamine | Solid: Meth, Speed, Whiz, Fast, Base, Pure, Point, P, Rabbit, Tail, Wax |
| Liquid: Red Speed, Liquid red, Leopard’s blood, Ox blood | |
| Crystal: Ice, d-meth, Glass, Crystal, Batu, Shabu | |
| 3,4-Methylenedioxymethamphetamine (MDA) | Adam, Bart Simpson, Clarity, Disco biscuits Essence, E, Ecstasy, Love drug, Red and black, White dove, X, XTC |
| 2,5-Dimethoxy-4-methylamphetamine (DOM) | Peace, Serenity, Tranquillity |
| 4-Bromo-2,5-dimethoxyphenethylamine (BDMPEA) | Nexus |
Table 12: Slang names of commonly abused amphetamines and substituted amphetamines [62].
According to United Nations 1971 Convention on Psychotropic Substances, amphetamine has been classified into schedule II controlled substance (Table 13) [104,105]. Therefore, use of amphetamine is comprehensively controlled in most countries. Countries like South Korea and Japan have even banned the therapeutic uses of substituted amphetamines [106,107]. In contrast, some countries, including the Netherlands (list I drug), the US (schedule II drug), Canada (schedule I drug), Australia (schedule 8), United Kingdom (class B drug) and Thailand (category 1 narcotic) allow medical uses of amphetamine [108].
| Amphetamines and Substituted Amphetamines | Legal Status of Amphetamines and Substituted Amphetamines by 2009 | |||
|---|---|---|---|---|
| UN+ | US | Russia | Australia | |
| Amphetamine (racemic) | Schedule II | Schedule II | Schedule II | Schedule VIII |
| D-amphetamine | Schedule II | Schedule II | Schedule I | Schedule VIII |
| L-amphetamine) | Schedule II | Schedule II | Schedule III | Schedule VIII |
| Methamphetamine | Schedule II | Schedule II | Schedule I | Schedule VIII |
| β-keto-amphetamine (Cathinone), a-methylamino-propiophenone (Methcathinone) | Schedule I | Schedule I | Schedule I | Schedule IX |
| 3,4-Methylenedioxyamphetamine (MDA), 3,4-Methylenedioxymethamphetamine (MDMA), 3,4-Methylenedioxy-N-ethylamphetamine (MDEA) | Schedule I | Schedule I | Schedule I | Schedule IX |
| p-Methoxyamphetamine (PMA) | Schedule I | Schedule I | Schedule I | Schedule IX |
| Dimethoxybromoamphetamine (DOB), 2,5-Dimethoxy-4-methylamphetamine (DOM), 3,4,5-Trimethoxyamphetamines (TMA) | Schedule I | Schedule I | Schedule I | Schedule IX |
| +United Nations Convention on Psychotropic Substances of 1971 | ||||
Table 13: Legal status of amphetamines and substituted amphetamines by 2009 in UN, US, Russia and Australia [20,105].
However, in these countries the medical uses of amphetamine are on a restrictive national drug schedule. Unfortunately, the illegal synthesis of amphetamine is still taking place in underground labs and is sold illegally, predominantly in European countries [108]. In 2013, about 1.2 million young adults of European countries used amphetamine or methamphetamine illegally. Whereas, the midst of 2012 around 5.9 metric tons of illegal amphetamine were detained within EU member countries. However, outside Europe, illegal market for amphetamine is much lesser as compared to MDMA and methamphetamine [109].
Conclusion
Even though amphetamine can be abused, these substances are additionally utilized for therapeutic purposes. Nevertheless, addiction to amphetamine particularly develops when prescription amphetamines are taken at much higher doses as compared to the doses used for therapeutic purposes. Consumption of gradually higher dosages due to “binge and crash” cycle and due to tolerance, physical dependence and psychological dependence are the possible phenomena with the abuse of amphetamines. In binge-crash cycle, following binge episodes, the amphetamine abuser crashes and faces anxiety, extreme fatigue, severe depression and a desire for more drugs. So, for the benefit of the nation, especially younger generation, caution must be taken to ensure rational use of amphetamines.
Authors’ Contributions
This work was carried out in collaboration between all authors. Author MSU designed the study, wrote the protocol, managed the analyses of the study and prepared the draft of the manuscript. Authors MAS, MTK, MFH, MN, II, AAM and MTI managed the literature searches and also participated in manuscript preparation. Author SK reviewed the scientific contents of the manuscript. All the authors read and approved the final manuscript.
Acknowledgement
The authors wish to thank the anonymous reviewer(s)/editor(s) of this article for their constructive reviews. The authors are also grateful to the Department of Pharmacy, Southeast University, Dhaka, Bangladesh.
Competing Interests
The authors proclaim that they have no competing interests.
References
- Heal DJ, Smith SL, Gosden J, Nutt DJ (2013) Amphetamine, past and present-A pharmacological and clinical perspective. J Psychopharmacol 27: 479-496.
- Maisto SA, Galizio M, Connors GJ (2011) Drug use and abuse. 6th Edition. United States: Wadsworth Publishing.
- Sinha A, Lewis O, Kumar R, Yeruva SL, Curry BH (2016) Amphetamine abuse related acute myocardial infarction. Case Rep Cardiol: 7967851.
- European monitoring centre for drugs and drug addiction (2016) Table GPS-1: Lifetime prevalence of drug use by age and country, most recent national general population survey available since 2000.
- European monitoring centre for drugs and drug addiction (2016) Table GPS-2: Last 12 months prevalence of drug use by age and country, most recent national general population survey available since 2000.
- European monitoring centre for drugs and drug addiction (2016) Table EYE-20: ESPAD 2011 school surveys: Lifetime prevalence (percentages) of psychoactive substance use among students 15-16 years.
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, et al. (2006) Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 67: 1062-1073.
- Borders TF, Booth BM, Han X, Wright P, Leukefeld C, et al. (2008) Longitudinal changes in methamphetamine and cocaine use in untreated rural stimulant users: Racial differences and the impact of methamphetamine legislation. Addiction 103: 800-808.
- Krcobic M (2016) Drugs details. Metadate vs. Adderall.
- Drug bank (2016) Amphetamine.
- Wimalasena K (2011) Vesicular monoamine transporters: Structure-function, pharmacology, and medicinal chemistry. Medicinal Rese Rev 31: 483-519.
- Sitte HH, Freissmuth M (2010) The reverse operation of Na(+)/C(l-)-coupled neurotransmitter transporters-why amphetamines take two to tango. J Neuroche 112: 340-355.
- Drug-rehabs.org (2016) Find alcohol treatment and drug rehab centers in bethesda.
- Study.Com (2016) How amphetamines work in the brain & body.
- European monitoring centre for drugs and drug addiction (2016) Amphetamine drug profile.
- Wikipedia (2016) Lisdexamfetamine.
- Vitiello B (2008) Understanding the risk of using medications for attention deficit hyperactivity disorder with respect to physical growth and cardiovascular function. Child Adolesc Psychiatr Clin N Am 17: 459-474.
- Skarner A, Svensson B (2013) Amphetamine use and sexual practices. Nordic Stu Alcohol Drugs 30: 403-23.
- Ramey JT, Bailen E, Lockey RF (2006) Rhinitis medicamentosa. J Investig Allergol Clin Immunol 16: 148-155.
- Wikipedia (2016) Amphetamine.
- Wikipedia (2016) Adderall.
- Shoptaw SJ, Kao U, Ling W (2009) Treatment for amphetamine psychosis. Cochrane Database Syst Rev: CD003026.
- Greydanus DE (2006) Stimulant misuse: Strategies to manage a growing problem.
- US food and drug administration (2016) Adderall XR®.
- Spiller HA, Hays HL, Aleguas A (2013) Overdose of drugs for attention-deficit hyperactivity disorder: clinical presentation, mechanisms of toxicity, and management. CNS Drugs 27: 531-543.
- INCHEM-International programme on chemical safety (2016) Amphetamine (PIM 934).
- Naghavi M, Wang H, Lozano R, Davis A, Liang X, et al. (2015) Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: A systematic analysis for the global burden of disease study 2013. Lancet 385: 117-171.
- Sulzer D, Sonders MS, Poulsen NW, Galli A (2005) Mechanisms of neurotransmitter release by amphetamines: a review. Prog Neurobiol 75: 406-433.
- Goldstein A (2001) Addiction: From biology to drug policy. 2nd Edition. New York: Oxford University Press.
- Carson-DeWitt R (2001) Encyclopedia of drugs alcohol & addictive behavior. 2nd Edition. Farmington Hills: Macmillan Reference USA.
- National institute on drug abuse (2016) Methamphetamine abuse and addiction.
- Morgan JP, Kagan D (1978) Street amphetamine quality and the controlled substances act of 1970. J Psychedelic Drugs 10: 303-317.
- Hill J (2016) Paul Erdos, mathematical genius, human (In That Order).
- Wilson A (2008) Mixing the medicine: The unintended consequence of amphetamine control on the Northern Soul Scene. Internet J Crimino: 1-22.
- Gyenis A (2016) Forty years of on the road 1957-1997.
- PubChem (2016) Amphetamine.
- Lemke TL, Williams DA, Roche VF, Zito W (2008) Foye's principles of medicinal chemistry. 6th Edition. Philadelphia, USA: Lippincott Williams & Wilkins.
- Brussee J, Jansen AC (May 1983) A highly stereoselective synthesis of s(-)-[1,1'-binaphthalene]-2,2'-diol. Tetrahedron Lett 24: 3261-3262.
- Malenka RC, Nestler EJ, Hyman SE (2009) Reinforcement and addictive disorders. In: Molecular neuropharmacology: A foundation for clinical neuroscience. 2nd Edition. New York: McGraw-Hill Medical.
- Bidwell LC, McClernon FJ, Kollins SH (2011) Cognitive enhancers for the treatment of ADHD. Pharmacol Biochem Behav 99: 262-274.
- Lewin AH, Miller GM, Gilmour B (2011) Trace amine-associated receptor 1 is a stereoselective binding site for compounds in the amphetamine class. Bioorg Med Chem 19: 7044-7048.
- Smith RC, Davis JM (1977) Comparative effects of d-amphetamine, l-amphetamine, and methylphenidate on mood in man. Psychopharmacology (Berl) 53: 1-12.
- Arnold LE (2000) Methyiphenidate vs. amphetamine: Comparative review. J Attention Disorders 3: 200-211.
- Eiden LE, Weihe E (2011) VMAT2: A dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse. Ann NY Acad Sci 1216: 86-98.
- Miller GM (2011) The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity. J Neurochem 116: 164-176.
- US food and drug administration (2016) DEXEDRINE® (Mixed salts of a single-entity amphetamine product) dextroamphetamine sulfate, dextroamphetamine saccharate, amphetamine aspartate monohydrate, amphetamine sulfate capsules, CII.
- Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, et al. (2011) ADHD drugs and serious cardiovascular events in children and young adults. N Engl J Med 365: 1896-1904.
- Habel LA, Cooper WO, Sox CM, Chan KA, Fireman BH, et al. (2011) ADHD medications and risk of serious cardiovascular events in young and middle-aged adults. JAMA 306: 2673-2683.
- US food and drug administration (2016) FDA drug safety communication: Safety review update of medications used to treat attention-deficit/hyperactivity disorder (ADHD) in children and young adults.
- Childs E, de Wit H (2009) Amphetamine-induced place preference in humans. Biol Psychiatry 65: 900-904.
- Berman SM, Kuczenski R, McCracken JT, London ED (2009) Potential adverse effects of amphetamine treatment on brain and behavior: A review. Molecular Psychi 14: 123-142.
- US food and drug administration (2016) Adderall® CII (Dextroamphetamine saccharate, amphetamine aspartate, dextroamphetamine sulfate and amphetamine sulfate tablets).
- Malenka RC, Nestler EJ, Hyman SE (2009) Higher Cognitive Function and Behavioral Control. In: Molecular neuropharmacology: A foundation for clinical neuroscience. 2nd Edition. New York: McGraw-Hill Medical
- Kanehisa laboratories (2016) Amphetamine -Homo sapiens (Human).
- Nechifor M (2008) Magnesium in drug dependences. Magnes Res 21: 5-15.
- Nestler EJ (2013) Cellular basis of memory for addiction. Dialogues Clin Neurosci 15: 431-443.
- Robison AJ, Nestler EJ (2011) Transcriptional and epigenetic mechanisms of addiction. Nat Rev Neurosci 12: 623-637.
- Ruffle JK (2014) Molecular neurobiology of addiction: what's all the (Δ)FosB about? Am J Drug Alcohol Abuse 40: 428-437.
- Olsen CM (2011) Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology 61: 1109-1122.
- Lynch WJ, Peterson AB, Sanchez V, Abel J, Smith MA (2013) Exercise as a novel treatment for drug addiction: A neurobiological and stage-dependent hypothesis. Neurosci Biobehav Rev 37: 1622-1644.
- Linke SE, Ussher M (2015) Exercise-based treatments for substance use disorders: Evidence, theory, and practicality. Am J Drug Alcohol Abuse 41: 7-15.
- Greene SL, Kerr F, Braitberg G (2008) Review article: Amphetamines and related drugs of abuse. Emerg Med Australas 20: 391-402.
- Albertson TE (2011) Amphetamines In: Poisoning & drug overdose. 6th Edition. New York: McGraw-Hill Medical.
- Hyman SE (1996) Addiction to cocaine and amphetamine. Neuron 16: 901-904.
- Amphetamines.com (2016) Amphetamine addiction.
- State government of victoria, Australia (2016) Amphetamines.
- Narconon (2016) Signs and symptoms of amphetamine abuse.
- Blue ridge mountain recovery center (2016) Your path to life-changing amphetamines addiction treatment.
- American psychiatric association (2010) Diagnostic and statistical manual of mental disorders. fourth edition text revision (DSM-IV-TR). American psychiatric association, Washington, DC.
- American psychiatric association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American psychiatric publishing, Washington, DC.
- Kollins SH (2008) A qualitative review of issues arising in the use of psycho-stimulant medications in patients with ADHD and co-morbid substance use disorders. Curr Med Res Opin 24: 1345-1357.
- Pérez-Mañá C, Castells X, Torrens M, Capellà D, Farre M (2013) Efficacy of psychostimulant drugs for amphetamine abuse or dependence. Cochrane Database Syst Rev : CD009695.
- Steiner H, Van Waes V (2013) Addiction-related gene regulation: Risks of exposure to cognitive enhancers vs. other psychostimulants. Prog Neurobiol 100: 60-80.
- Kanehisa Laboratories (2016) Alcoholism - Homo sapiens (human).
- Nestler EJ (2014) Epigenetic mechanisms of drug addiction. Neuropharmacology 76 Pt B: 259-268.
- Pitchers KK, Vialou V, Nestler EJ, Laviolette SR, Lehman MN, et al. (2013) Natural and drug rewards act on common neural plasticity mechanisms with ?FosB as a key mediator. J Neurosci 33: 3434-3442.
- Beloate LN, Weems PW, Casey GR, Webb IC, Coolen LM (2016) Nucleus accumbens NMDA receptor activation regulates amphetamine cross-sensitization and deltaFosB expression following sexual experience in male rats. Neuropharmacology 101: 154-164.
- Blum K, Werner T, Carnes S, Carnes P, Bowirrat A, et al. (2012) Sex, drugs, and rock 'n' roll: hypothesizing common mesolimbic activation as a function of reward gene polymorphisms. J Psychoactive Drugs 44: 38-55.
- DoveMed (2016) Facts about amphetamine dependence.
- Uddin MS, Sufian MA, Hossain MF, Kabir MT, Islam MT, et al. (2017) Neuropsychological effects of caffeine: Is caffeine addictive?. J Psychol Psychother 7: 1-12.
- Lintzeris N, Dunlop A, Lintzeris N (1996) Getting through amphetamine withdrawal: A guide for people trying to stop amphetamine use. Fitzroy, Vic: Turning point alcohol and drug centre.
- Shoptaw SJ, Kao U, Heinzerling K, Ling W (2009) Treatment for amphetamine withdrawal. Cochrane Database Syst Rev : CD003021.
- Rawson RA (2002) Treatment for stimulant use disorders. New York: US department of health and human services.
- Mental health daily (2016) Adderall tolerance: Causes & how to prevent it.
- Porter R (2009) The merck manual home health handbook. 3rd Edition. New York: Wiley.
- Australian government department of health and ageing (2007) National amphetamine-type stimulant strategy background paper (National drug strategy series no. 69) Australia: National drug research institute Australian institute of criminology.
- Dassonville P, Lewis SM, Zhu XH, Ugurbil K, Kim SG, et al. (2001) The effect of stimulus-response compatibility on cortical motor activation. Neuroimage 13: 1-4.
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, et al. (1990) Comorbidity of mental disorders with alcohol and other drug abuse. Results from the epidemiologic catchment area (ECA) Study. JAMA 264: 2511-2518.
- Ringen PA, Melle I, Birkenaes AB, Engh JA, Faerden A, et al., (2008) The level of illicit drug use is related to symptoms and premorbid functioning in severe mental illness. Acta Psychiatr Scand 118: 297-304.
- Bell DS (1973) The experimental reproduction of amphetamine psychosis. Arch Gen Psychiatry 29: 35-40.
- Griffith JJ, Oates J, Cavanaugh J (1968) Paranoid episodes induced by drugs. JAMA 205:155-69.
- Harris D, Batki SL (2000) Stimulant psychosis: Symptom profile and acute clinical course. Am J Addict 9: 28-37.
- Chambers RA, Krystal JH, Self DW (2001) A neurobiological basis for substance abuse comorbidity in schizophrenia. Biol Psychiatry 50: 71-83.
- Chambers RA, Sentir AM, Engleman EA (2010) Ventral and dorsal striatal dopamine efflux and behavior in rats with simple vs. co-morbid histories of cocaine sensitization and neonatal ventral hippocampal lesions. Psychopharmacology (Berl) 212: 73-83.
- Advokat C (2007) Update on amphetamine neurotoxicity and its relevance to the treatment of ADHD. J Atten Disord 11: 8-16.
- Carvalho M, Carmo H, Costa VM, Capela JP, Pontes H, et al. (2012) Toxicity of amphetamines: an update. Arch Toxicol 86: 1167-1231.
- Bowyer JF, Hanig JP (2014) Amphetamine- and methamphetamine-induced hyperthermia: Implications of the effects produced in brain vasculature and peripheral organs to forebrain neurotoxicity. Temperature (Austin) 1: 172-182.
- Hofmann FG (1983) A Handbook on drug and alcohol abuse: The biomedical aspects. 2nd Edition. New York, USA: Oxford university press.
- Arbor pharmaceuticals LLC (2016) EVEKEO® (amphetamine sulfate tablets, USP).
- US food and drug administration (2016) VyvanseTM (lisdexamfetamine dimesylate).
- Drug bank (2016) Lisdexamfetamine.
- US food and drug administration (2016) ADZENYS XR-ODT (Amphetamine extended-release orally disintegrating tablets), CII.
- DoctorsHangout.com (2016) Amphetamine: In society and culture.
- Transnational institute (2016) The UN drug control conventions.
- Wikipedia (2016) Substituted amphetamine.
- The korean times (2016) Moving to korea brings medical, social changes.
- Japanese ministry of health, labour and welfare (2016) Importing or bringing medication into Japan for personal use.
- United Nations office on drugs and crime (2014) World drug report 2014. New York: United Nations publication.
- European monitoring centre for drugs and drug addiction (2014) European drug report 2014: Trends and developments. Lisbon, Portugal: European monitoring centre for drugs and drug addiction.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 14617
- [From(publication date):
August-2017 - Apr 06, 2025] - Breakdown by view type
- HTML page views : 13487
- PDF downloads : 1130