Research Article Open Access
Amebic Liver Abscess is Associated with Malnutrition and Low Serum Leptin Level
Faisal Alam1*, Abdus Salam2, Iftekhar Mahmood3, Mamun Kabir1, Sharif Chowdhury4 and Rashidul Haque41Rajshahi Medical College, Bangladesh
2King Saud bin Abdulaziz University for Health Sciences, Jeddah, KSA
3Kushtia Medical College, Bangladesh
4Parasitology Laboratory, ICDDR.B, Dhaka, Bangladesh
- *Corresponding Author:
- Faisal Alam
Rajshahi Medical College, Bangladesh
E-mail: faisal_imm@yahoo.com
Received date: July 09, 2016; Accepted date: October 21, 2016; Published date: October 24, 2016
Citation: Alam F, Salam A, Mahmood I, Kabir M, Chowdhury S, et al. (2016) Amebic Liver Abscess is Associated with Malnutrition and Low Serum Leptin Level . J Infect Dis Ther 4:298. doi:10.4172/2332-0877.1000298
Copyright: © 2016 Alam F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Infectious Diseases & Therapy
Abstract
Background and Objective: Amebic liver abscess (ALA), the most common form of extra-intestinal amebiasis is caused by the protozoan parasite E. histolytica. It is a prevalent parasitic infection in the northern region of Bangladesh for which hospital admission is required. The aim of this investigation was to explore the clinical spectrum of amebic liver abscess and its relationship with malnutrition and serum biomarker leptin.
Methods: The study population included 90 hospitalized ALA patients and 90 healthy controls during the period of July 2012 to June 2015. Liver abscess was diagnosed initially by ultrasound imaging and amebic liver abscess was confirmed by detection of E. histolytica DNA in abscess aspirates using a Real Time PCR. Body Mass Index (BMI) was measured conventionally for nutritional status and serum leptin was estimated by ELISA.
Results: Among the ALA cases (N=90), 37% had low BMI against only 3% of controls (N=90) [p<0.0001 at 95% CI]. About69 (76%) of low BMI patients had large or multiple liver abscess in comparison to 29% of standard BMI (p<0.0001 at 95% CI). Likewise, body fluid derangements such as edema, pleural effusion and ascites, either solitary or in combination were significantly higher (87% vs. 37%) among ALA with low BMI than standard BMI. Overwhelming majority of ALA patients 81(90%) was hypoleptinaemic.
Conclusion: Malnutrition and low serum leptin are important associations in amebic liver abscess patients with significance in disease outcomes.
Keywords
Amebic liver abscess; Malnutrition; Leptin
Introduction
Amebiasis caused by Entamoeba histolytica is the third leading cause of parasitic infections associated mortality worldwide [1]. Two major clinical syndromes of amebiasis are intestinal amebiasis and amebic liver abscess; together they are estimated to result in 50 million infections and 100,000 deaths worldwide each year. Amebic liver abscess (ALA) is considered to be the principal cause of mortality from this protozoan infection [2]. In Indian subcontinent, overall prevalence rate of amebiasis was 13.7% [3] and in Bangladesh no concrete data are available but one study of ICDDR,B shows children of urban Bangladesh had a 4.2% prevalence of E. histolytica infection [4]. Incidences and prevalence of amebic liver abscess in Rajshahi are not recorded officially by government authority till date but number of admitted cases is recorded 279 and 196 in the year of 2005 and 2007 respectively.
It has long been hypothesized that malnutrition and infectious disease are interacting causes for ill health in developing countries. It has now been scientifically established that many infectious diseases like tuberculosis, childhood diarrhea, measles, childhood respiratory infections, helminthiasis are associated with malnutrition [5-7]. Recent studies have also shown the link between childhood malnutrition and susceptibility to amebiasis. There are reports that being well-nourished limits the susceptibility of children to symptomatic intestinal amebiasis, while children with E. histolytica associated diarrheal illness are almost three times as likely to be malnourished and about five times more likely to be stunted [8,9]. However, it is not yet known whether there is any relationship between nutritional status and susceptibility to amebic liver abscess. Studies on amebic liver abscess carried out in Vietnam, Mexico, India and Bangladesh demonstrated a strong association between ALA and poor socioeconomic status indirectly suggesting that malnutrition is associated with ALA cases [10-12]. However, the lack of anthropometric data limited the ability of these studies to draw conclusive causal association of ALA patients with poor nutritional status.
Recently leptin, a product of the obese (ob) gene secreted from fat cells was discovered and found that mice deficient in leptin had profound immune deficiencies and were malnourished. Several recent studies have also found a relation between serum leptin and malnutrition along with susceptibility to infection [13]. The aim of this study was to investigate relationship of amebic liver abscess with malnourishment and serum leptin level and to translate the association of these factors in disease outcomes.
Methods
The study population included 90 amebic liver abscess patients who were admitted into Rajshahi Medical College Hospital (a tertiary level public hospital in northern Bangladesh) during the period from July 2012 to June 2015 and 90 healthy volunteers of comparable age, sex and ethnicity as controls. Five milliliters of liver abscess pus was collected from ALA patients and 6 milliliters of blood were drawn from both patients and controls. Informed written consent was obtained from both patients and controls. The study was reviewed and approved by the Institutional Review Board (IRB) of the Institute of Biological sciences, University of Rajshahi, Bangladesh.
Diagnosis of ALA patients
Clinically, liver abscess was suspected in patients presenting with high fever and right upper quadrant pain with subsequent findings of space occupying lesions in the liver, suggestive of abscess by ultrasonography. ALA was confirmed by detection of E. histolytica specific DNA by Real Time PCR.
Anthropometric measurement
Anthropometric measurements of the study population were taken at the time of enrollment. Each case and control was weighed in kilograms in light clothes with an electronic weighing scale; standing heights were measured up to the nearest 0.1 cm using a standard height scale. Nutritional status was assessed by measuring Body Mass Index (BMI), taking height and weight into consideration using BMI calculator. Each measurement was checked by standard metric formula, stated as BMI= weight in kilograms/height in m². According to the 1998 NIH recommendation [14], a BMI below 18.5 for adult males or 18.0 for adult females is considered low; while BMI above 27.8 for males or 27.3 for females is considered over weight or high. BMI in between these mentioned values is considered as standard).
Real Time PCR
Liver abscess pus of 1 μl was used as sample for PCR following standard procedure as described by Petri et al. [15]. The oligonucleotide primers and Taqman probes were designed to specifically amplify a 135-bp fragment inside the 16S-like smallsubunit rRNA gene of E. histolytica (Gene Bank accession number X64142). Primers and probe were purchased from Eurogentec, United Kingdom. Amplification reactions were performed in a volume of 25 μl with Qiagen super mix. Amplification results were analyzed using i- Cycler software, version 3.0 for Windows.
Serum leptin assay
Serum leptin was estimated using a commercially available kit from Alpha Diagnostic International, Texas, USA. It is based on binding human leptin from samples to two antibodies, one immobilized on the micro titer plates and the other bound to the enhancing protein biotin, which then binds to streptavidin horseradish peroxidase conjugate. Adding a chromogenic substrate develops color. The enzymatic reaction is directly proportional to the amount of leptin present in the sample. (Serum leptin value is expressed in nanogram/ml. Normal range of leptin is between 1.2-8 ng/ml for males and 3.7 -11.2 ng/ml for females.)
Statistical analysis
Arithmetic mean was calculated for BMI. Degree of hepatic injury by measuring number & size of abscesses, morbidity and duration of hospital stay of patients with standard BMI and low BMI was compared by Fisher’s exact test. Pearson’s correlation between serum leptin and BMI of patients and controls was done.
Results
Body Mass Index and serum leptin levels were correlated for ALA patients and healthy controls.
BMI of patients and controls: Out of 90 ALA cases, 37(41.1%) had low BMI against only 3.3% of controls (Table 1). The BMI value of ALA patients was significantly lower (p<0.0001) than the controls.
| Standard BMI | Low BMI | Total | P value | |
|---|---|---|---|---|
| Patient | 53 (58.9%) | 37 (41.1%) | 90 | |
| Control | 87 (96.7%) | 03 (3.3%) | 90 | <0.0001 |
| Out of 90 ALA cases, 37 (41.1%) had low BMI against only 3.3% of controls. The BMI value of ALA patients was significantly lower (p<0.0001) than the controls. | ||||
Table 1: BMI value of patients and controls.
BMI and hepatic injury: Seventy six percent (76%) of low BMI patients had large (>15 cm diameter) or multiple liver abscess in comparison to 29% of standard BMI (Table 2). Low BMI was significantly (p<0.0001 at 95% CI) associated with more liver damage in ALA patients.
| Multiple and/or Large abscess | Single and/or Small abscess | P value | ||
|---|---|---|---|---|
| Patient with standard BMI (n=53) | 15 (29%) | 38 (71%) | 53 | <0.0001 |
| Patient with low BMI (n=37) | 28 (76%) | 09 (24%) | 37 | |
| Total | 43 | 47 | 90 | |
| Seventy six percent (76%) of low BMI patients had large (>15 cm diameter) or multiple liver abscess in comparison to 29% of standard BMI. Low BMI was significantly (p<0.0001 at 95% CI) associated with more liver damage in ALA patients. | ||||
Table 2: Effect of BMI on degree of hepatic injury.
BMI and duration of hospital stay: Patients with low BMI had more duration (>3 weeks) of hospital stay for recovery than patients of standard BMI (p<0.0001) (Table 3).
| <2 weeks | >3 weeks | P value | ||
|---|---|---|---|---|
| Patients with standard BMI | 48 (53.3%) | 05 (5.5%) | 53 (58.8%) | |
| Patients with Low BMI | 04 (4.4%) | 33 (36.7%) | 37 (41.2%) | |
| Total | 52 (57.7%) | 38 (42.2%) | 90 (100%) | <0.0001 |
| Patients with low BMI had more duration (>3 weeks) of hospital stay for recovery than patients of standard BMI (p<0.0001) (Table 3). | ||||
Table 3: Correlation of BMI and duration of hospital stay.
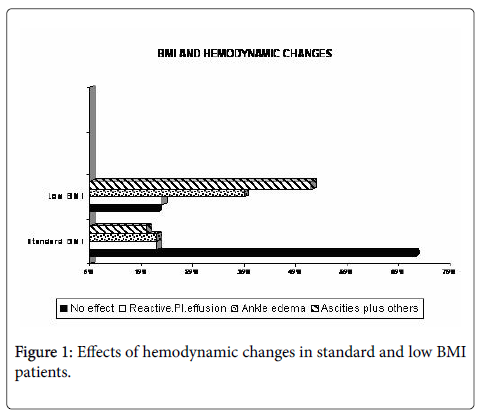
BMI and hemodynamic derangement: The relationship between BMI values and clinical effects related to interstitial fluid imbalance in amebic liver abscess patients was observed. Figure 1 shows the spectra of hemodynamic derangements of ALA patients. We categorized hemodynamic derangement of ALA on the basis of imbalance between hydrostatic and osmotic pressure into four grades; 0= no effects observed, 1= reactive pleural effusion, 2 = ankle edema and 3 = generalized edema along with ascites. Signs of these effects were more pronounced among low BMI patients. The majority of ALA patients with low BMI have had grade 3 derangements, while the other two grades were equivocal between normal and subnormal BMI of ALA patients.
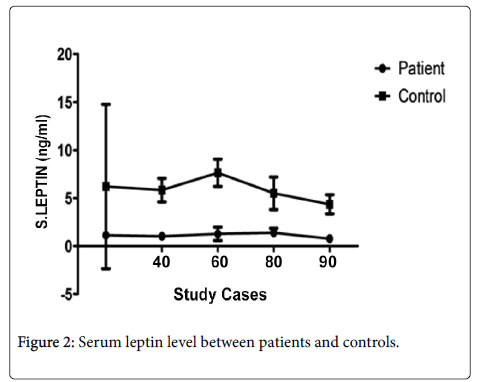
Serum leptin level: Out of 90 ALA patients, 82 (90%) had low serum leptin levels compared to 12% (11/90) in healthy controls (Figure 2). The mean serum leptin level in ALA patients and healthy controls was 1.12 ng/ml and 6.67 ng/ml respectively and Pearson’s correlation between serum leptin and BMI of patients and controls was 0.8233 and 0.6974, respectively, and (p<0.0001).
Discussion
Important finding of this study is that nutritional status is an important contributing factor for amebic liver abscess. Malnourished populations are more vulnerable to infection with this parasite and significantly low BMI (p<0.0001) among ALA patients than that of controls demonstrated in this study has substantiated this correlation. Furthermore, ALA patients had significant association of malnutrition with the extent of liver injury presenting with very large and/or multiple abscesses and more hemodynamic derangements like edema or effusion leading to more hospital stay in comparison to ALA with standard BMI.
Many previous studies found that malnourished individuals were more likely to acquire E. histolytica - associated diarrheal illness where serum leptin level played a critical role [9,16]. In this study, we found over 90% (82/90) of acute ALA cases had low serum leptin compared to healthy controls (12%). Pearson’s correlation between serum leptin and BMI of patients and controls was 0.8233 and 0.6974, respectively, which indicates that serum leptin is proportional to BMI of ALA patients and controls. A few healthy controls 11(12%) from rural populations also showed poor serum leptin level in comparison to none from urban controls, possibly reflecting the poor nutritional status of the rural population. Lower leptin level among patients indicates that their malnourished status is directly proportional to disease status, as described in a previous paper [11].
We can assume from these results that the majority of ALA patients are hypo-leptinaemic with a concomitant greater chance of infection with E. histolytica and other infectious agents. Malnourished and hypo-leptinaemic rural populations are more vulnerable than their urban counterparts.
An important paradox of amebic liver abscess is that most patients suffering from this disease do not have coexisting amebic colitis nor a history of dysentery at the time of enrollment and similar report was made by Haque et al. [17]. We can conclude from our findings that low serum leptin level and poor nutritional status might play a role for the invasion of E. histolytica into the liver, but how these two factors play role in pathogenesis is still a question to be explored by us and others [18].
It has been shown in a few studies that conditions of reduced leptin production are also associated with increased infection susceptibility [19,20]. However, our study observed that amebic liver infection is associated with hypo-leptinaemia, but whether a hypoleptinaemic state is responsible for the development of amebic liver abscess or amebic liver infection reduces the leptin level could not be ascertained through the present study.
Conclusion
The most remarkable finding of this study is the association between malnutrition and amebic liver abscess and this association is directly proportional with disease progression and extent of liver injury. Hypoleptinaemia is another important factor related to amebic liver infection. However, more extensive studies are required to find out the causal or consequent role of leptin in amebic liver abscess and its complications.
Acknowledgements
Authors are thankful to Nadakavukaren, Professor Emeritus, Department of Biology from Illinois State University, Illinois, USA for his contribution in language correction of this manuscript.
Competing Interests
The authors have no conflict of interest.
Authors Contributions
FA & RH conceived, designed and wrote the manuscript, AS analyzed data and helped in revising and editing the manuscript, IM selected and attended the patients, SC detected liver abscess by ultrasonography, MK performed experiments. All authors read and approved the final manuscript.
References
- World Health Organization (1997) Amoebiasis. WHO Wkly Epidemiol.
- Haque R, Huston CD, Hughes M, Houpt E, Petri WA (2003) Current concepts: amebiasis. N Engl J Med 348: 1565-1573.
- Nath J, Ghosh SK, Singha B, Paul J (2015) Molecular Epidemiology of Amoebiasis: A Cross-Sectional Study among North East Indian Population. PLoS Negl Trop Dis 9: e0004225.
- Haque R, Faruque AS, Hahn P, Lyerly DM, Petri WA Jr (1997) Entamoeba histolytica and Entamoeba dispar infection in children in Bangladesh. J Infect Dis 175: 374-376.
- el Samani EF, Willett WC, Ware JH (1988) Association of malnutrition and diarrhea in children aged under five years a prospective follow-up study in a rural Sudanese community. Am J Epidemiol 128: 93-105.
- Macallan DC (1999) Malnutrition in tuberculosis. Diagn Microbiol Infect Dis 34: 153-157.
- Bhaskaram P (1995) Measles & malnutrition. Indian J Med Res 102: 195-199.
- Haque R, Mondal D, Shu J, Roy S, Kabir M, et al. (2007) Correlation of interferon gamma production by peripheral blood mononuclear cells with child hood malnutrition and susceptibility to amebiasis. Am J trop Hyg 76: 340-344.
- Mondal D, Petri WA, Sack RB, Kirkpatrick BD, Haque R (2006) Entamoeba histolytica- associated diarrheal illness is negatively associated with the growth of preschool children: evidence from a prospective study. Trans R Soc Trop Med Hyg 100: 1032-1038.
- Blessman J, Van LP, Tanich E (2002) Epidemiology of amebiasis in a region of high incidence of amebic liver abscess in central Vietnam. Am J Trop Med Hyg 66: 578-583.
- Shamsuzzaman SM, Haque R, Petri WA (2000) Socioeconomic status, Clinical features, laboratory and parasitological findings of hepatic amebiasis patients - a hospital based prospective study in Bangladesh. Southeast Asian J Trop Med Public Health 31: 399-404.
- Siddiqui MA, Ekram ARSM, Islam QT, Hoque MA, Masum QAAI (2008) Clinico-Pathological Profile of Liver Abscess in a Teaching Hospital. Teachers Assoc J Rajshahi 21: 46-48.
- Moore SE, Morgan G, Collinson AC, Swain JA, O’Connell MA, et al. (2002) Leptin, malnutrition, and immune response in rural Gambian children. Arch Dis Child 87: 192-197.
- http://www.nhlbi.nih.gov/health/health-topics/topics/obe/diagnosis
- Petri WA, Roy S, Kabir M, Mondal D, Ali IKM, et al. (2005) Real Time PCR assay for diagnosis of Entamoeba histolytica infection. J Clin Microbiol 43: 2168-2172.
- Mondal D, Haque R, Sack RB, Kirkpatrick BD, Petri WA (2009) Attribution of malnutrition to cause-specific diarrheal illness: evidence from a prospective study of preschool children in Mirpur, Dhaka, Bangladesh. Am J Trop Med Hyg 80: 824-826.
- Haque R, Mollah NU, Ali IKM, Alam K, Eubanks A, et al. (2000) Diagnosis of Amebic Liver Abscess and Intestinal Infection with the TechLab Entamoeba histolytica II Antigen Detection and Antibody Tests. J Clin Microbiol 38: 3235-3239.
- Katzenstein D, Rickerson V, Braude A (1982) New concepts of amebic liver abscess derived from hepatic imaging, serodiagnosis, and hepatic enzymes in 67 consecutive cases in San Diego. Medicine (Baltimore) 68: 237-246.
- Petri WA, Mondal D, Peterson KM, Duggal P, Haque R (2009)Association of malnutrition with amebiasis. Nutr Rev 67: 207-215.
- Cava LA, Matarese G (2004) The weight of leptin in immunity. Nature Rev Immunol 4: 371-379.
Relevant Topics
- Advanced Therapies
- Chicken Pox
- Ciprofloxacin
- Colon Infection
- Conjunctivitis
- Herpes Virus
- HIV and AIDS Research
- Human Papilloma Virus
- Infection
- Infection in Blood
- Infections Prevention
- Infectious Diseases in Children
- Influenza
- Liver Diseases
- Respiratory Tract Infections
- T Cell Lymphomatic Virus
- Treatment for Infectious Diseases
- Viral Encephalitis
- Yeast Infection
Recommended Journals
Article Tools
Article Usage
- Total views: 12249
- [From(publication date):
October-2016 - Nov 21, 2024] - Breakdown by view type
- HTML page views : 11504
- PDF downloads : 745