Alcohol Use Disorder and its Correlates among Health Professionals
Received: 01-Jan-1970 / Accepted Date: 01-Jan-1970 / Published Date: 30-Jun-2018 DOI: 10.4172/1522-4821.1000393
Abstract
Background: Alcohol is commonly used psychoactive drug particularly among adults. Harmful use of alcohol leads to occupational, social and physical impairment. However, studies on Alcohol Use Disorder (AUD) among Health Professionals (HPs) remains limited in Ethiopia.
Objective: This study aimed to determine prevalence of AUD and to identify its risk factors among HPs working in tertiary teaching hospital, Southwest Ethiopia.
Methods: In this study, facility based cross-sectional study design was employed. Pretested, structured, self-administered questionnaire was utilized to collect data. The CAGE instrument was used to screen HPs for AUD. The data were coded, cleaned and analyzed by using SPSS version 16 software program. Variables with p-value <0.05 at multivariate logistic regression were identified to know the risk factors for AUD.
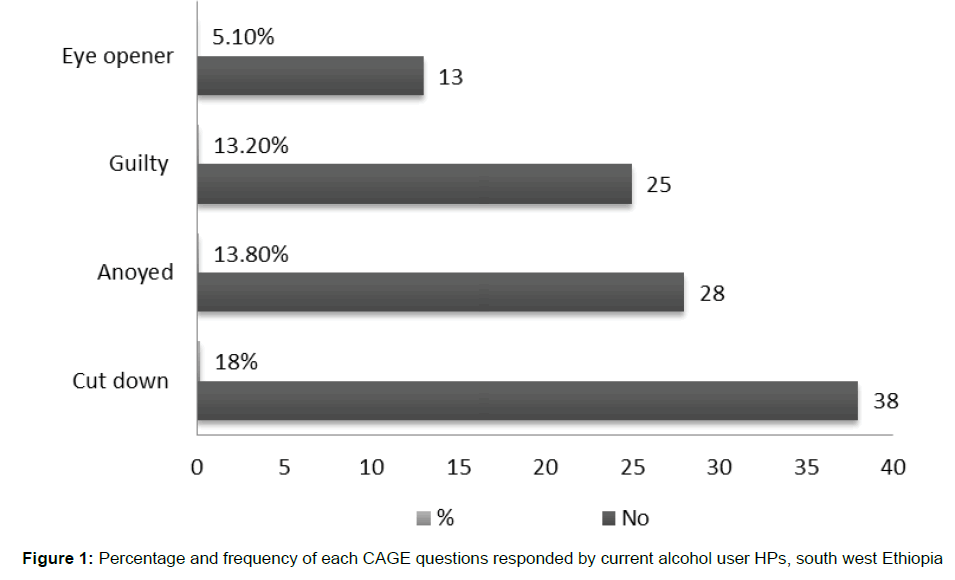
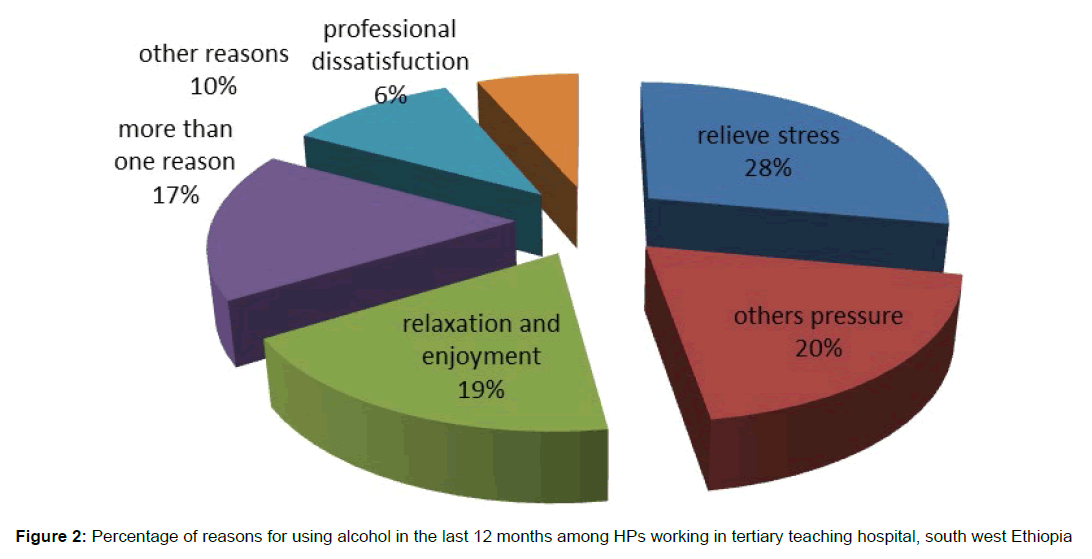
Result: Off the total participants (n=334), 41.7% and 34.4% were ever and current users of alcohol respectively. Prevalence of AUD was 8.1%. Eighteen percent of current alcohol users felt the need to cut down. Few of them (5.1%) had the need of alcohol in the morning as an eye opener. The main reason given by participants for alcohol use was “to get relief from stress and exhaustion” (26.1%) followed by “peer pressure” (18.3%), and “for relaxation” (17.4%). Based on the results the results of this study, the odds of AUD were lower among those with higher education, no psychological distress, and no current khat use among HPs in Northwest Ethiopia.
Conclusion: HPs identified to have prevalence of AUD the same to the general population. Prevention, treatment, and rehabilitation of AUD find to be crucial. Addressing enabling factors found to be important in this era of alcohol beverage promotions by companies.
Keywords: Alcohol use disorder, Health professionals, South west Ethiopia
Introduction
The use of psychoactive substances has become one of the raising public health and socio-economic problems worldwide (Deressa & Azazh, 2011). Alcohol found to be the most commonly used drug in Africa followed by tobacco and khat in East Africa predominantly (Gureje et al., 2007). Adult per capita of alcohol consumption has been grown by 25% from 2001-2005 in Africa (World Health Organization, 2011).
Substance use remains public concern of all segment of Ethiopian population particularly among adults. Ethiopia, one of the oldest independent African countries registered a dramatic increment in alcohol consumption per capita in the last few decades (Deressa & Azazh, 2011; World Health Organization, 2011).
Harmful use of alcohol is a major global contributing factor to high mortality, morbidity and physical injury. It has physical health impacts such as alcohol dependence, liver cirrhosis, cancers and injuries; and to others accident and violence are very commonly associated with harmful alcohol drinking habits (World Health Organization, 2011). Alcohol and alcohol related morbidity and mortality is a major public health problem attributable to more deaths than all the other drugs combined globally (Physicians and Lawyers for National Drug Policy, 2008).
Health Professionals (HPs) are not immune to substance abuse. Like most people, they can experience the same situations that contribute to Alcohol Use Disorder (AUD) such as low social support, low self-esteem, family problems, psychological disorders and stress. There are also particular factors that put HPs at a greater risk of AUD such as professional stress; of contact with people who are seriously ill and dying, and long hours of practice (Counsel On Drug Abuse, 2009).
Alcohol is mostly used for recreational purposes by medical and paramedical society. Residents and attending physicians use drugs of abuse for performance enhancement and as selftreatment for various reasons, such as, pain, anxiety, or depression (Baldisseri, 2007).
Substance induced impairment among HPs is reported to grow in recent times. Any physical, psychological and social impairment of HPs could place the public at increased risk for errors (Kenna & Lewis, 2008).
Alcohol is the most commonly abused drug by HPs (Gureje et al., 2007; Kenna & Lewis, 2008; LaGuire, 2014). American Medical Association (AMA) in 2014 reported approximately 14% of HPs develop AUD which is equivalent with the general population (LaGuire, 2014). Another study in University of Rhode Island revealed 25% prevalence of recent alcohol use among HPs (Kenna & Lewis, 2008). A study in Nigeria reported 56% ever users and 14% current users alcohol. Males were more likely than females to be users of alcohol (Gureje et al., 2007).
Some mentioned risk factors of AUD among HPs were moderate or more frequency of alcohol use, being in situations when alcohol served, feeling immune to the addictive effects of alcohol and socializing with alcohol abusers. HPs with young age and short service year as well as poor social network were highly linked with AUD (Deressa & Azazh, 2011; Kenna & Lewis, 2008; Reisdorfer et al., 2012).
Harmful use of alcohol by working forces can be harmful beyond physical health; leading to social and occupational impairment (Deressa & Azazh, 2011). However, the magnitude of AUD and its correlation has not been investigated well among HPs in Ethiopia. This study was conducted to determine the prevalence of AUD and to identify factors that influenced it among HPs working in tertiary teaching hospital south west Ethiopia.
Materials And Methods
Method
Institution based cross sectional study design was employed among HPs working in tertiary teaching hospital, south west Ethiopia. The study was conducted for a period of 1 month from January 15, 2014 to February 15, 2014. The study area was Jimma University Specialized Hospital (JUSH) which is the only tertiary care hospital in south west parts of Ethiopia.
All four hundred and three HPs working in this facility included in the study. A self-administered questionnaire which was prepared in English language was used for data collection. AUD was the outcome variable. The independent variables were sociodemographic characteristics, social and psychological variables; other substances use (Khat and tobacco) habits and work-related factors. Questionnaires were distributed to all HPs who were available during the data collection period. The distributed questionnaires were collected within working days by the principal investigators.
Measures
CAGE the quick alcohol misuse screening tool was used to detect AUD. The CAGE instrument has been validated in numerous studies as a good, quick and primary indicator of AUD in primary health care settings (Cherpitel, 1997; Maisto & Saitz, 2003; Castells & Furlanetto, 2005; Dhalla & Kopec, 2007). The tool is designed to be a screening tool rather than a diagnostic instrument. Score of two positive responses to any of the 4 CAGE questions was taken as a positive test result. Using two as cutoff value, the CAGE’s sensitivity in various populations ranges from 61-100 percent, and its specificity ranges from 77 to 96 percent (Castells & Furlanetto,2005; Dhalla & Kopec, 2007). The reason why the author used CAGE is because of its simplicity to screen AUD, and it is user friendly which can be used by lay people. Burnout was detected by using Copenhagen’s burnout inventory (CBI) tool which was used and validated in different studies (Carlotto et al., 2013; Potter et al., 2010). The mean score of CBI was used to categorize burnout as cut of point, to classify as low and high burnout. The mean was included to the high burnout score. Self-report questionnaire (SRQ-20) tool was utilized to detect psychological distress. To say psychological distress a score of greater or equal to 8 in SRQ-20 items was taken. This instrument was developed by world health organization (WHO) to screen psychological distress in primary health care settings (World Health Organization division of Mental Health, 1994). Health professional refers to all trained and certified professionals including physicians, nurses, pharmacist, laboratory technologists, physiotherapist, anesthetist and others.
Statistical Analysis
Data were coded, entered and cleaned using Epi Info 7. It exported and analyzed by using SPSS version 16. Both chisquare test and bivariate logistic regression were used to test the association between outcome variable and independent variables one by one. Variables with p-value less than 0.05 in multivariate regression were considered to be risk factors of AUD.
Ethical clearance and permission was obtained from Jimma University ethical committee. Before data collection started, permission was also obtained from the hospital medical director office. Both written and oral consent were delivered to the candidates. During distribution of the questionnaire HPs were told that the information collected would be kept confidential. Only HPs who were willing to participate taken the questionnaire.
Results
Out of four hundred and three distributed questionnaires 334 were returned by study participants. Almost two third (64.7%, n=213) of them were male. HPs involved in this study were young by age with mean age of 28.6 year (SD=7.65). Half of the respondents were single (50%, n=167) in marital status. Three fourth (71.0%, n=237) were nurses and more than half (55.1%, n=183) indicated they had obtained a bachelor’s degree shown in Table 1.
| Socio-demographic characteristics | No | % | |
|---|---|---|---|
| Sex | Female | 116 | 35.2 |
| Male | 213 | 64.5 | |
| Religion | Orthodox | 156 | 46.7 |
| Protestant | 108 | 32.3 | |
| Muslim | 63 | 18.9 | |
| Others1 | 7 | 2.1 | |
| Ethnicity | Oromo | 166 | 49.7 |
| Amhara | 92 | 27.5 | |
| Wolayta | 13 | 3.9 | |
| Guragie | 10 | 3.0 | |
| Tigre | 10 | 3.0 | |
| Others2 | 43 | 12.9 | |
| Marital status | Single | 167 | 50.0 |
| Married | 114 | 34.1 | |
| In relationship | 33 | 9.9 | |
| Divorced or Widowed | 13 | 3.9 | |
| Other3 | 6 | 1.8 | |
| Profession | Nurse | 237 | 71.0 |
| Pharmacist | 29 | 8.7 | |
| Lab. Technologist | 25 | 7.5 | |
| Medical Doctor | 15 | 4.5 | |
| Others4 | 16 | 4.8 | |
| Educational status | Diploma | 138 | 41.6 |
| First Degree | 183 | 55.1 | |
| Second degree and above | 10 | 3.0 | |
Table 1 Socio-demographic characteristics of HPs working in tertiary teaching hospital, south west Ethiopia
Among study subjects, 41.7% (n=138) and 34.4% (n=115) were ever and current users of alcohol respectively. The prevalence of AUD in this study was 8.1%. Eighteen percent of current alcohol users felt the need to cut down. Few of them (5.1%) had the need of alcohol in the morning as an eye opener. Figure 1 shows percentage and frequency of each CAGE responses given by study subjects. The main reason given by participants for alcohol use was “to get relief from stress and exhaustion” (26.1%) followed by “peer pressure” (18.3%), and “for relaxation” (17.4%). Figure 2 and Table 2 shows the reasons given by study participants for alcohol use.
| Reasons | Alcohol use in the last 12 months | |
|---|---|---|
| No | % | |
| To relieve stress and exhaustion | 87 | 26.1 |
| professional dissatisfaction | 20 | 6.0 |
| Others pressure on me | 61 | 18.3 |
| For relaxation | 58 | 17.4 |
| More than one reason | 52 | 15.6 |
| To alleviate post-khat chewing discomfort | 23 | 6.9 |
| Other reason | 33 | 9.7 |
Table 2 Reasons given by HPs for using alcohol in the last 12 months, south west Ethiopia
Table 3 shows the results of chi-square and bivariate association between the outcome variable and independent factors. Statistically significant difference (p<0.05) was seen between the outcome variable and the independent variables of not interested one’s own profession, psychological distress, current khat and tobacco use, disagreement with colleagues and bosses at work, and having poor social support. However, at multivariate logistic regression; having lower academic rank, current khat use and psychological distress found to be independent predictors of AUD as shown on Table 4.
| Selected Variables | AUD | ||||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-value | ||||||
| Academic status | Diploma | 15 | 10.9 | 123 | 89.1 | 1.10(0.13-9.28) | 0.93 |
| 1st degree | 11 | 6.0 | 171 | 94.0 | 0.58(0.07-4.99) | 0.62 | |
| 2nd degree and above | 1 | 10.0 | 9 | 90.0 | 1 | ||
| Sex | Female | 5 | 4.3 | 111 | 95.7 | 1 | |
| Male | 21 | 9.9 | 191 | 90.1 | 2.44(0.90-6.66) | 0.08 | |
| Profession | Nurse | 19 | 8.1 | 217 | 91.9 | 0.41(0.04-4.06) | 0.45 |
| Medical doctor | 1 | 6.7 | 14 | 93.3 | 0.50(0.16-1.61) | 0.25 | |
| Pharmacist | 3 | 10.3 | 26 | 89.7 | 0.66(0.13-3.28) | 0.62 | |
| Others | 4 | 14.8 | 23 | 85.2 | 1 | ||
| Professional Interest | Interested | 7 | 4.0 | 168 | 96.0 | 1 | |
| Not interested | 20 | 12.7 | 137 | 87.3 | 3.50(1.44-8.53) | 0.01* | |
| Psychological distress | Yes | 22 | 16.7 | 110 | 83.3 | 1 | |
| No | 5 | 2.6 | 187 | 97.4 | 0.13(0.05-0.36) | 0.00 * | |
| Burnout | Yes | 16 | 10.9 | 131 | 89.1 | 1 | |
| No | 11 | 6.0 | 171 | 94.0 | 0.53(0.24-1.17) | 0.12 | |
| Job Security | Secured | 17 | 7.1 | 224 | 92.9 | 1 | |
| Insecured | 10 | 11.0 | 81 | 89.0 | 1.63(0.72-3.70) | 0.25 | |
| Current khat use | Yes | 20 | 22.5 | 69 | 77.5 | 1 | |
| No | 7 | 2.9 | 237 | 97.1 | 0.10(0.04-0.25) | 0.00* | |
| Current tobacco use | Yes | 11 | 32.4 | 23 | 67.6 | 1 | |
| No | 16 | 5.4 | 283 | 94.6 | 0.12(0.05-0.28) | 0.00* | |
| Physical illness | Yes | 8 | 11.6 | 61 | 88.4 | 1 | |
| No | 19 | 7.2 | 244 | 92.8 | 0.59(0.25-1.42) | 0.24 | |
| Part time work | Yes | 10 | 10.8 | 83 | 89.2 | 1 | |
| No | 17 | 7.1 | 222 | 92.9 | 0.64(0.28-1.44) | 0.28 | |
| Prospect of promotion | Dissatisfactory | 18 | 10.7 | 150 | 89.3 | 1 | |
| Satisfactory | 9 | 5.6 | 152 | 94.4 | 0.49(0.22-1.13) | 0.10 | |
| Relationship with staffs and bosses |
Disagreement | 9 | 23.1 | 30 | 76.9 | 1 | |
| Intimate | 18 | 6.2 | 274 | 93.8 | 0.22(0.10-0.53) | 0.01* | |
| Social support | Poor | 5 | 35.7 | 9 | 64.3 | 1 | |
| Good | 22 | 6.9 | 295 | 93.1 | 0.13(0.04-0.44) | 0.01* | |
| (*) indicates that, the variable is significantly associated with the outcome variable at P-value less than 0.05 | |||||||
Table 3: Bivariate Logistic Regression: Factor associated with AUD among HPs working in tertiary teaching hospital, Ethiopia
| Selected Variables | AUD | ||||||
|---|---|---|---|---|---|---|---|
| OR (95%CI) | p-value | ||||||
| Academic status | Diploma | 15 | 10.9 | 123 | 89.1 | 1 | |
| 1st degree | 11 | 6.0 | 171 | 94.0 | 0.01(0.01-0.17) | <0.05* | |
| 2nd degree and above | 1 | 10.0 | 9 | 90.0 | 0.01(0.01-0.42) | <0.05* | |
| Psychological distress | Yes | 22 | 16.7 | 110 | 83.3 | 1 | |
| No | 5 | 2.6 | 187 | 97.4 | 0.05(0.01-0.53) | <0.05* | |
| Current Khat use | Yes | 20 | 22.5 | 69 | 77.5 | 1 | |
| No | 7 | 2.9 | 237 | 97.1 | 0.06(0.01-0.40) | <0.05* | |
| (*) indicates that, the variable is significantly associated with the outcome variable at P-value less than 0.05 | |||||||
Table 4: Multivariate Logistic Regression: Factors associated with AUD among HPs working in tertiary teaching hospital, south west Ethiopia
Discussion
This research found 8.1% prevalence of AUD which is consistent with previous study finding (Kilpatrick, 2008). AUD prevalence in this study was lower compared to previous research outcomes [Baldisseri, 2007; Kenna & Lewis, 2008; Reisdorfer et al., 2012). Those studies reported highest prevalence of AUD were (14% in USA, 18.4% in Brazil, 25% in Rhode Island) compared to the current result (8.1%). American HPs had similar prevalence of AUD with the general population of the same country (Baldisseri, 2007; Center for Behavioral Health Statistics and Quality, 2015). Availability and access to a variety of alcoholic beverages is much higher in America than this study area. Whenever access for alcohol products is so easy, then prevalence and incidence of alcohol use increases in the same way proportionally in the general population including among HPs (LaGuire, 2014). The discrepancy observed between Brazilian and the current study may be because of Brazilian study was a population based and the study subjects were adults with high socio-economic status who were residents of Florianópolis, a city with high Human Development Index (Reisdorfer et al., 2012). Further Brazilian study used Alcohol Use Disorders Identification Test (AUDIT) to detect AUD which probably raises the prevalence compared to CAGE. The authors of research from Rhode Island mentioned as they used “The composite instrument” as limitation of their study and the reason for higher prevalence was the tool they used among HPs.
People took alcohol for a variety of reasons most commonly it is taken to cope with the physical and psychological stress, to cope up with unexpected life challenges, to relax with peers, to fulfill major obligations, and for social reasons (Kangule et al., 2011; Myadze & Rwomire, 2014). Similar reasons were reported by HPs in this study. HPs participated in this research took alcohol to get relief from stress and exhaustion predominantly (26.1%) followed by social pressure (18.3%), and for relaxation (17.4%).
The odds of AUD are 95% less likely for those with no psychological distress compared to those with psychological distress (P<0.05, AOR=0.05, 95%CI=0.01-0.53). It is consistent with the outcome of several study findings of which AUD and psychological distress commonly co-exist (Kilpatrick, 2008; Gyawali et al., 2016; Asrat et al., 2015). These research outcomes agree with the statement of ‘high psychological distress symptoms are common among individuals with AUD.
The odds of AUD are 94% less likely for those with no current kaht use habit compared to current khat users. The possible relationship between current khat use habit and AUD is consistent with previous research results (Deressa & Azazh, 2011). Concordant use of alcohol and khat is observed as these studies found out. Current khat abusers are at increased financial problems associated with the use, greater problems with occupational functioning and higher rates of mental health problems, higher psychological distress and poorer quality of life (Asrat et al., 2015). Because of inadequate standardized treatment option in Ethiopia, they remain untreated (Asrat et al., 2015). So, they may probably prefer to cope up with maladaptive behaviors such as harmful use of alcohol.
This study identified educational status as directly associated with AUD (p<0.05). HPs who had highest educational background showed lower risk of AUD compared with diploma graduates. It is consistent with similar study in Mumbai, India (Kangule et al., 2011) which reported as educational status increases a chance of using any form of substance decreases proportionally. Different reasons may explain the result. Behavior and attitude of individuals towards alcohol use is determined by level of knowledge and understanding about its effects in one’s own life. Individuals with lower educational attainment may have lesser knowledge and poorer coping skills to deal with their stress and thereby increase risk of AUD (Gyawali et al., 2016). Furthermore, alcohol is taken out of home in bars, groceries and hotels with groups and a great deal of time spent specifically to this study area. General Practioners (GPs) and specialized physicians are highly preoccupied with high burden of patients not only in the institution but also in private health care facilities. So that time is limited to spend outside for alcohol use. However, it contradicts with the outcome of a research which found out higher rates of drug abuse among physicians with certain areas of specialization in USA (Baldisseri, 2007). A study in USA screened physicians only for addition to alcohol. Further it incorporated large sample size with different methodology. However our study under represents specialized physicians because of its low response rate by them. Probably high income of USA physicians compared to the Ethiopians ones may also explain the reason of high prevalence of AUD among HPs in USA.
This study is limited in several ways. Social support was not assessed with standard and validated tool. It was one of the limitation of this study. Lower response rate from physicians and high academic status (Masters degree and specialized physician) HPs probably under represented by the result. Mostly studies conducted at HPs showed low response rate due to several reasons (Deressa & Azazh, 2011; Kenna & Lewis, 2008; Reisdorfer et al., 2012).
Conclusion
Alcohol use has been public health problem among HPs with significant occupational, social and economic implications. Addiction of by HPs should be of major concern to the profession and to society. This result identified almost the same prevalence of AUD with the general population. This reflects that HPs are equally vulnerable for AUD regardless of their knowledge. Its prevalence is higher among females, nurses, and with HPs with lower educational status. Based on the results of this study, the odds of AUD were lower among those with higher education, no psychological distress, and no current khat use. Having these factors, stockholders need to focus mainly on preventions of alcohol use among HPs. At the same time designing effective strategies for the treatment and rehabilitation of HPs with AUD found to be very crucial.
Acknowledgement
I would like to acknowledge Jimma University for it fruitful support.
References
- Asrat, B., Girma, E., Soboka, M., & Tesfay, K. (2015). Mental distress and associated factors among health professionals working in tertiary teaching hospital, south west ethiopia. J Depress Anxiety, 4(3): 1-6. Baldisseri, M.R. (2007). Impaired healthcare professional. Crit Care Med, 35(2): 108. Carlotto, M.S., Pizzinato, A., Rocha, K.B., & Oliveira-Machado, R.D. (2013). Prevalence and factors associated with burnout syndrome in professionals in basic health units. Ciencia &Trabajo, 15(47): 76-80. Castells, M.A., & Furlanetto, L.M. (2005). Validity of the CAGE questionnaire for screening alcohol-dependent inpatients on hospital wards. Rev Bras Psiquiatr, 27(1): 54-7. Center for Behavioral Health Statistics and Quality. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15-4927, NSDUH Series H-50), September 2015. Cherpitel, C.J. (1997). Brief screening instruments for alcoholism. Alcohol Health Res World, 21(4): 348-351. Counsel On Drug Abuse. (2009). Health Professionals & Substance Use. CODA Report, Toronto, Canada; page 505. Deressa, W., & Azazh, A. (2011). Substance use and its predictors among undergraduate medical students of Addis Ababa University in Ethiopia. BMC Public Health, 11: 660. Dhalla, S., & Kopec, J.A. (2007). The CAGE questionnaire for alcohol misuse: A review of reliability and validity studies. Clin Invest Med, 30(1): 33-40. Duresso S.W., Matthews, A.J., Ferguson, S.G., & Bruno, R. (2016). Is khat use disorder a valid diagnostic entity? Addiction, 111(9): 1666-1676. Gureje, O., Degenhardt, L., Olley, B., Uwakwe, R., Udofia, O., Wakil, A., et al. (2007). A descriptive epidemiology of substance use and substance use disorders in Nigeria during the early 21st century. Drug Alcohol Depend, 91(1): 1-9. Gyawali, B., Choulagai, B.P., Paneru, D.P., Ahmad, M., Leppin, A., & Kallestrup, P. (2016). Prevalence and correlates of psychological distress symptoms among patients with substance use disorders in drug rehabilitation centers in urban Nepal: A cross-sectional study. BMC Psychiatry, 16(1): 314. Kangule, D., Darbastwar, M., & Kokiwar, P. (2011). A cross sectional study of prevalence of substance use and its determinants among male tribal youths. Int J Pharm Biomed Sci, 2(3): 61-64. Kenna, G.A., & Lewis, D.C. (2008). Risk factors for alcohol and other drug use by healthcare professionals. Subst Abuse Treat Prev Policy, 3(3): 1-8. Kilpatrick, D. (2008). Understanding substance abuse in adolescents: A primer for mental health professionals. The National Child Traumatic Stress Network, 1-19. LaGuire, T. (2014). Work place impairment of the health care professionals. Quantum Units Education, 1-8. Maisto, S.A., & Saitz, R. (2003). Alcohol use disorders: Screening and diagnosis. Am J Addict, 12: 512-525. Myadze, T.I., & Rwomire, A. (2014). Alcoholism in Africa during the late twentieth century: A socio-cultural perspective. International Journal of Business and Social Science, 5(2). Physicians and Lawyers for National Drug Policy. Alcohol and Other Drug Problems: A Public Health and Public Safety Priority. Brown University center for Alcohol and Addiction Studies, April 2008;page 64. Potter, P., Deshields, T., Divanbeigi, J., Berger, J., Cipriano, D., Norris, L., et al. (2010). Compassion fatigue and burnout: Prevalence among oncology nurses. Clin J Oncol Nurs, 14(5): E56-62. Reisdorfer, E., Buchele, F., Pires, R.O., & Boing, A.F. (2012). Prevalence and associated factors with alcohol use disorders among adults: A population-based study in southern Brazil. Rev Bras Epidemiol, 15(3): 582-94. World Health Organization division of Mental Health. (1994). User’s Guideline to the Self Reporting Questionnaire. World Health Organization Geneva. World Health Organization. (2011). Global status report on alcohol and health. Geneva, Switzerland.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 5793
- [From(publication date): 0-2018 - Dec 20, 2024]
- Breakdown by view type
- HTML page views: 5073
- PDF downloads: 720