Alcohol and Substance Use among Patients in Palliative Care
Received: 25-Jun-2021 / Accepted Date: 20-Sep-2021 / Published Date: 27-Sep-2021 DOI: 10.4172/2165-7386.1000427
Abstract
There has been a growing concern about alcohol and substance use and abuse as well as abuse of prescription drugs among patients in hospice and palliative care. Literature reveals that it is likely that similar risk factors for substance abuse in persons in the general public may also exist among the terminally ill. Substance abuse among such patients could interfere with effective pain and symptom management regimes that are employed in palliative care. Numerous studies have been conducted on prevalence of substance abuse in the general public as well as special populations such as persons with disability. However, very little has been documented regarding drug use and abuse in persons with advanced chronic conditions such as patients in palliative care settings. Prevalence of alcoholism and other substances among patients in palliative care has scarcely been reported in Kenya. This study adopted a descriptive survey targeting patients with advanced cancer in an outpatient palliative care setting. Questionnaires and interviews were used to establish the prevalence of drug use among patients, the main drugs of abuse as well as risk factors for drug abuse in these patients. Purposive sampling was used to obtain a total of 50 patients within an outpatient palliative care facility. The results indicated that alcohol and tobacco were the most abused substances among patients. Those who abused tobacco either smoked or used chewing as a mode of administration. A few respondents used other substances such as artane while others chewed betel. The study recommended use of rigorous assessment to identify patients with previous or current history of substance abuse in order to employ suitable interventions. Addressing substance abuse in these settings could allow the accomplishment of appropriate palliative care services as well as maintenance of self-dignity and enhancement of quality of life for the patients and their significant others.
Keywords: Palliative care; Drug abuse; Substance abuse
Introduction
Substance and other drug use is a widespread problem within the larger population. It is estimated that a quarter of a billion (5%) of the global population aged between 15 to 64 years used drugs in the year 2015 [1]. According to the National Survey on Drug Use and Health [2] 86.4 % of people aged 18 years and above reported using alcohol. In Kenya, approximately 37.1% of the population has used one substance of abuse [3]. In addition, drug use has also been reported among special populations, with about 35% of persons with disability (PWDs) having used drugs [4]. These statistics are likely to be a reflection of some special populations within the clinical settings such as patients in hospice and palliative care (HPC) settings. The main focus of palliative care is to offer a holistic approach that provides patients with relief from symptoms, pain, and stress of life-limiting illnesses. The goal is to enhance the quality of life (QOL) for both the patient and the family. This is in line with the (SDGs) whose 3rd goal is ensure healthy lives and enhancement of wellbeing of persons of all ages. However, the use or abuse of illicit drugs and other substances in these settings may complicate patient care and symptom management. Consequently, the main objective of care may not be adequately achieved.
The prevalence of substance use disorder (SUD) in HPCs is not clear. Studies indicate a rising trend in drug and substance abuse within the general public, meaning that this is likely to be the case within hospice settings. In the recent past, there has been a growing concern about alcohol and substance use and abuse among patients in HPCs as well as diversion of prescription drugs. Affirms that substance abuse incidences are as common among persons suffering life limiting illnesses as in the general population [5]. In the United States (U.S.) statistics show estimated base rates of 6 to 15% of substance abuse in palliative care [6]. Other estimates indicate 34 % of illicit drug use in patients suffering chronic pain [7] and 28 % of alcohol use in palliative care [7]. Findings from a study on SUD in men with advanced stage prostate cancer indicated a prevalence of 10.6% [8]. Despite these trends the issue of alcohol and other substance use and abuse is an understudied phenomenon in HPCs in Kenya.
Coast Hospice supports patients and families facing life limiting illnesses particularly cancer and HIV&AIDS within the coastal region of Kenya. The goal of the hospice team is to be sensitive and responsive to the special requirements of each individual and family. Most patients in hospices in Kenya present with advanced disease [9]. Thus, majority of these patients have a heavy symptom burden, with approximately 75% experiencing moderate to severe pain [10]. The intense pain may necessitate constant and higher doses of opioids or other medication for pain and symptom relief. The challenges of drug use and abuse in hospices are numerous. Literature reveals that it can be challenging for caregivers to manage or deal with patients with a history of substance use disorder or those recovering from the same [11]. Some of these patients may fear using opioids for pain relief even when suffering intense pain. In some cases, the use of opioids for severe pain in terminally ill patients may not adequately contain the pain while in other cases, half of the patients do not respond at all [10]. Moreover, the physical, psychological and emotional distress that comes with these conditions may weigh down the coping mechanisms of these patients as well as their caregivers. Consequently, this could pose a risk for maladaptive coping including use or abuse of alcohol and other drugs.
Use of illicit drugs among this population can pose serious challenges in pain and symptom management which is the primary focus in palliative care. In addition it can cause adverse interaction issues with the medication prescribed for treatment of the chronic and life limiting illnesses which are common in these settings. Thus drug use may impede the quality of life (QOL) of these patients leading to more complexities in management of their physical and psychosocial needs.
Hospice programs began in the late 1970’s, while in Kenya the first hospice (Nairobi Hospice) was opened in 1990 [12]. The Kenya Hospices and Palliative Care Association’s (KEHPCA), an umbrella body that oversees the programs in Kenya, aims to promote and support culturally acceptable and affordable quality palliative care throughout Kenya [13]. This goal may not be achieved satisfactorily if issues related to substance abuse among patients are not adequately addressed. Furthermore, alcohol and drug abuse are documented by the Government of Kenya as a major threat to the lives of her citizens [14]. This applies to the population in hospices as well. It is paramount that issues related to drug use in hospices are recognized and addressed.
Method
This study adopted a cross sectional descriptive survey targeting patients with advanced cancer in an outpatient hospice care facility. Purposive sampling was used to obtain a total of 50 patients. Questionnaires were used to establish the trend of drug use as well as the demographic characteristics of the participants. Assessment of alcohol was done using the CAGE questionnaire. In addition, participants were asked whether they had ever used or were still using drugs or any other substances. An interview schedule was used to determine the perceived effects of substance use. Descriptive statistics were used to summarize the demographic data and trends of alcohol and other substances used by patients in the hospice.
Results
Characteristics of respondents
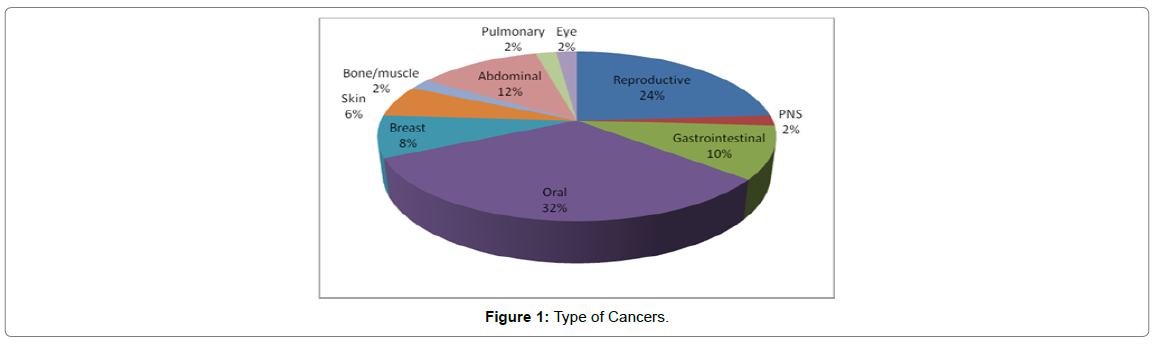
A total of 50 patients registered with the Coast Hospice participated in the study. The socio-demographic characteristics of the respondents are summarized in the Table 1 and Figure 1.
| Characteristic | Frequency | Percentage |
|---|---|---|
| Gender | ||
| Male | 28 | 56 |
| Female | 22 | 44 |
| Age in years | ||
| 20-30 | 3 | 6 |
| 31-40 | 6 | 12 |
| 41-50 | 10 | 20 |
| 51-60 | 15 | 30 |
| 61 and above | 16 | 32 |
| Total | N=50 |
Table 1: Gender and Age of the Respondents.
Generally there were slightly more males (56%) compared to the female respondents. The mean age of the participants was 57.7 years, with the majority being 50 years and above.
Type of cancers among respondents
Analysis of the types of cancers among the respondents was done and summarized in Figure 1. The results indicated that majority (32%) of the respondents had oral cancer which affects the regions around the mouth. 24 % suffered cancer related to the reproductive organs such as cervix and prostrate. Few respondents had cancer of the eye, bone, peripheral nervous system (PNS) and pulmonary regions.
Trends of alcohol and other substance use among respondents
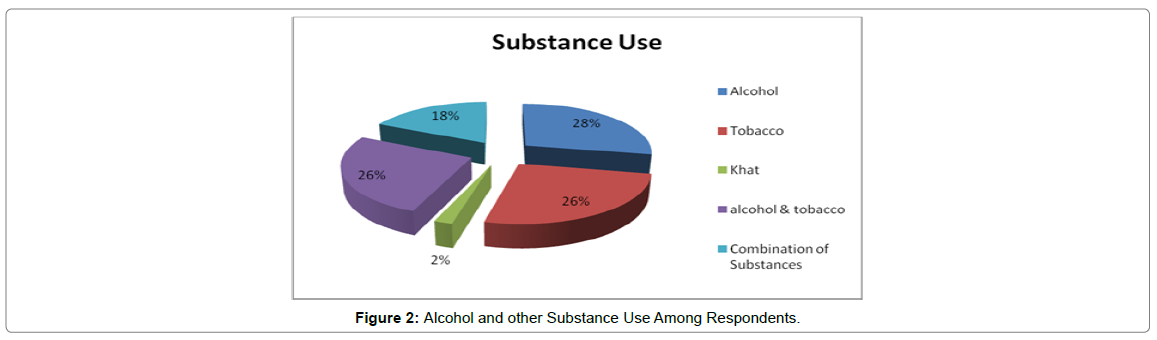
The results indicate that alcohol and tobacco were the most abused substances among patients. A smaller percentage of the respondents used khat and a combination of substances including artane and betel nuts. The results are summarized in Figure 2.
Those who abused tobacco either smoked or used chewing as a mode of administration. A significant number of respondents (26%) used both alcohol and tobacco while a few respondents used a combination of other substances such as artane, bhang, and betel nuts. This concurs with the findings of studies by NACADA which found that, the common substances of abuse in Kenya and particularly in the coastal region include among others alcohol, tobacco, bhang and Khat [15]. In addition, similar results were found in a study by NACADA on drug abuse among people with disabilities [4].
Gender and substance use
The study showed that the most abused substances among both genders were alcohol and tobacco as shown in Figure 3.
Use of tobacco was found to be higher in females (69.2%) compared to males (30.8%). Majority of the females chewed tobacco, while alcohol use was higher in males (64.3%) than women as shown. Combined use of various substances (alcohol, tobacco, khat, bhang, betel nuts and artane) was similar across the genders (50%).
Age and substance use
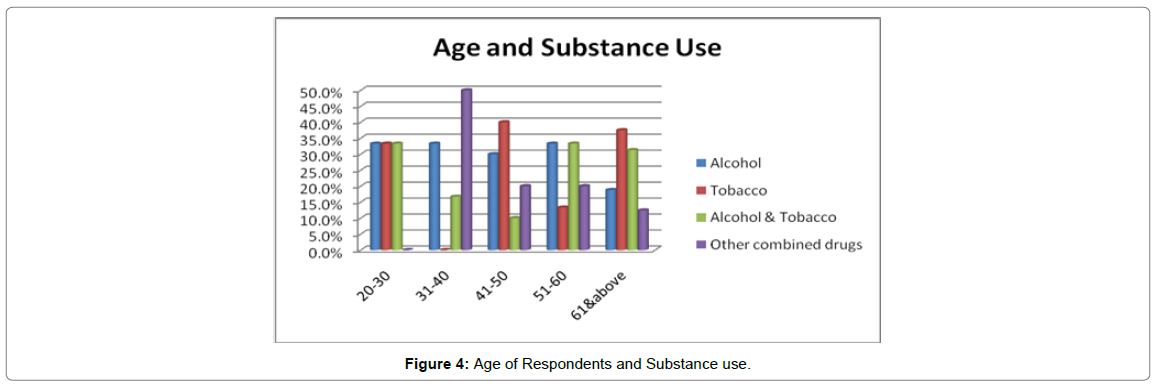
Alcohol was highly used among respondents aged between 20 and 60 while tobacco was used by majority of the respondents aged between 20-30 (33.3%), 41-50 (40%), and 61+ (37.5%) respectively. Combined use of various substances was exhibited across different ages with the highest (50%) being between 31-40 years while respondents between 20 -30 years did not use combined substances as shown in Figure 4.
Perceived effects of drug use among respondents
An interview with the care givers was used to determine the perceived effects of drug and substance use among the patients. The findings were drawn upon the main themes that emerged during the interview process.
Poor pain and symptom management
There was a likelihood of poor pain and symptom management for patients who used or abused drugs and other substances. One caregiver stated: “Most of the patients we see with drug problems always complain of pain and other related symptoms despite our efforts to manage their conditions, which is sometimes frustrating”. Symptom and pain management are the key pillars of palliative care [16]. This is because majority of the patients in hospices present with advanced disease and they suffer a variety of symptoms as well as intense pain. Thus, abuse of drugs is likely to interfere with the medicine regimens offered in these facilities. In some cases the patients may not respond well to the pain medication. Literature indicates that approximately 30- 50% of patients in hospice care receive inadequate pain relief [7]. In cases where the care providers are uncertain of the patient’s drugs of abuse, symptoms management can be challenging [14]. In addition the situation may be even more challenging particularly if the care givers are inadequately training to handle addictions, thus resulting in poor management of the patients.
Higher dose of medication for pain relief
Additionally, the patients who abuse drugs are likely to require higher doses of medicines for pain relief. This may be due to the craving pain caused by withdrawal symptoms which the patient may mistake as cancer pain. There is a possibility that the course of the disease can be altered as the chemicals in the drugs of abuse interact with the medication used for symptom management [14]. Consequently, more or even stronger pain relief medicine may be required to manage these changes as one caregiver said: “Some of these patients are not totally open about their struggles with drugs, but we notice that they need more medication frequently, so we increase their dosages gradually or even change their drug regimens”.
Increased financial burden
When patients’ needs for medicine increases, it may have a snowballing effect leading to higher costs of providing this medicine, thus creating a financial burden both to the hospice and the patient. Majority of the patients the hospice come from poor backgrounds and they are expected to cost share in the purchasing of medicine with the hospice. So when their need for alcohol or other drugs is added on to their routine budget, it increases the financial difficulties which can be heavy for their families who carry the burden of care.
Depression and suicidal tendencies
Patients in hospices suffer a myriad of complex symptoms with physical, psychological, social as well as spiritual dimensions. Some of the participants reported feeling depressed after using drugs. A variety of consequences have been recorded in literature including but not limited to emotional anguish, anxiety, anger, and depressive moods [14,16]. Use of drugs could magnify the levels of distress particularly because these patients in end life care are faced with impending death. Drug abuse is likely to increase suffering and sometimes suicidal tendencies may result.
Effects on the patients’ family
Addiction and drug abuse is likely to increase family conflicts with the patient. Hospice care generally operates more like a family since the team incorporates the family in caring for the patient. Persons who abuse drugs have a tendency to exhibit extreme behaviours. Some commonly reported consequences of drug use include legal problems and financial burden [16] which impacts the family negatively. Additionally, drug addiction or abuse is likely to have adverse effects on the patient thus adding on the disease burden. This may complicate and increase the burden of care on the family. Subsequently, conflicts are likely to arise and at times the patient is abandoned by family members. A care giver affirms: “Some of the patients are abandoned by their families especially if they are abusing drugs and are unwilling to quit” He adds: “others are influenced by their own family members to take drugs when we find out we try to counsel both the patients and their families on the risks of mixing these drugs with medication”.
Strategies to address drug use and abuse
The suggested strategies to curb drug abuse include:
1. Use of a comprehensive approach that includes various classes of drugs and different non-pharmacological modalities for pain and symptom management such as: relaxation therapy, music, guided imagery, biofeedback among others.
2. To ensure that patients have medication available when they need it.
3. To encourage care providers to exercise professional responsibility to prescribe controlled substances appropriately. Pain must be adequately managed, regardless of past and current addictions in order to prevent self-medication and drug abuse.
4. Intensive counseling to reduce psychosocial suffering, reduce the possibility that somatization of that suffering will result in increased pain expression, and discourage the use of alcohol or drug abuse as a solution to psychosocial suffering.
Conclusion
In this study, use of alcohol and other substances was assessed among patients in the hospice. The findings showed that there is a relatively high prevalence of alcoholism and tobacco use among these patients. Other drugs such khat, betel nuts and artane are also use especially as a combination. Therefore, alcohol and drug use is real in hospice settings. Most of these patients come to the hospice through referrals from other clinical settings. It is not clear whether the assessment or diagnosis were made in their first encounters in those settings. What is emerging is that alcoholism and use of other substances is underdiagnosed and undertreated. Drug and substance use among these patients poses a real challenge in managing them and it impedes appropriate pain and symptom management.
Recommendations
From the findings, the study makes the following the recommendation:
1. The study recommends use of rigorous screening and assessment to identify patients with previous or current history of drug and substance abuse in order to employ suitable interventions.
2. Screening needs to be incorporated in the routine clinical care in hospices.
3. In addition, it is critical that the staff are adequately prepared and trained to use the appropriate tools and to conduct comprehensive assessment. This will ensure proper diagnosis and appropriate interventions including referrals.
4. Furthermore, the multidisciplinary team could be expanded to include professional mental health experts such as psychologists and counselors who will then compliment the palliative care team. Addressing substance abuse in these settings could allow the accomplishment of appropriate palliative care services as well as maintenance of self-dignity and enhancement of quality of life for the patients and their significant others.
5. Network with rehabilitation institutions to help in treating those struggling with drug addiction.
6. One of the main goals of the SDGs focuses on strengthening prevention and treatment of substance abuse. It is therefore imperative that specialized care is accorded to this population.
7. Given the challenges highlighted within the palliative care teams, there is need to work closely with families of these patients to minimize the burden of care. It is critical that the palliative care teams in these settings are adequately trained and prepared to be competent in order to reduce these challenges.
8. The Government through the Ministry of health should integrate hospice and palliative care and this calls for budget allocations to ensure adequate training as well expansion of the multidisciplinary team to accommodate experts in the addiction field.
Conflicts of Interest
All authors confirm that there is no conflict of interest.
References
- Furtos R (2018) World Drug Report 2017: 29.5 million people globally suffer from drug use disorders, opioids the most harmful. United Nations | Office on Drugs and Crime
- Ahrnsbrak R, Kroutil L, Harter R, Tice P, Hunter D (2016) 2015 National Survey on Drug Use and Health: Summary of the Effects of the 2015 NSDUH Questionnaire Redesign: Implications for Data Users, Pp: 1-44.
- Baseline Survey Report (2016) Status of Alcohol and Drug Abuse in the Coast Region, Kenya. National Authority for the Campaign of Alcohol and Drug Abuse [NACADA].
- Kathungu B, Mwaura LW, Wambugu B (2013) Report On Alcohol, Drugs And Substance Abuse Among Persons With Disability In Nairobi, Coast And Central Regions Kenya. NACADA
- O’Brien CP (2021) Managing patients with a history of substance abuse. Canadian Family Physician. College of Family Physicians of Canada 60: 248.
- Starr TD, Rogak LJ, Passik SD (2010) Substance abuse in cancer pain. Curr Pain Headache Rep 14: 268-75.
- Schenker Y, Arnold R (2015) The Next Era of Palliative Care. JAMANetwork 314: 1565-566.
- Chhatre S, Metzger DS, Malkowicz B, Woody G, Jayadevappa R (2014) Substance use disorder and its effects on outcomes in men with advanced-stage prostate cancer. Cancer 120(21): 3338-345.
- Ali Z (2016) Kenya Hospices and Palliative Care Association: integrating palliative care in public hospitals in Kenya. Ecancermedicalscience 10: 655.
- Fabbro ED (2014) Assessment and Management of Chemical Coping in Patients With Cancer.Journal of Clinical Oncology 16: 1734-738.
- Ebenau A, Dijkstra B, Hurrne CT, Hasselar J, Vissers K, et al. (2020) Palliative care for patients with substance use disorder and multiple problems: a qualitative study on experiences of healthcare professionals, volunteers and experts-by-experience. BMC Palliat Care 19: 8
- Kenya Hospices and Palliative Care Association [KEHPCA] (2016) Annual Report 2015.
- Sanger SC (2012) End-of-Life Care & Addiction: A Family Systems Approach, by Suzanne Young Bushfield and Brad DeFord. Social Work in Health Care 51: 271-274
- National Authority for the Campaign of Alcohol and Drug Abuse [NACADA] (2016) National Survey on Alcohol and Drug Abuse among Secondary School. Natl Surv alcohol drug Abus among Second Sch students Kenya.
- Macleod R, Vella-Brincat J, Macleod S (2016) The Palliative Care Handbook guidelines for clinical management and symptom control (8th Edn). The Palliative Care Handbook 8: 1-163.
Citation: Musili PM, Kimotho SK, Ouma CA, Amisi E Njoroge NM (2021) Alcohol and Substance Use among Patients in Palliative Care. J Palliat Care Med 11: 427. DOI: 10.4172/2165-7386.1000427
Copyright: © 2021 Musili PM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2611
- [From(publication date): 0-2021 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 2023
- PDF downloads: 588