Airway Stenting: An Overview upon a Single Centre Series
Received: 28-Mar-2017 / Accepted Date: 20-Apr-2017 / Published Date: 27-Apr-2017
Abstract
Endobronchial stents are widely used to treat stenosis of the airway that are not suitable for surgery. Procedure will be successful for well selected patients for whom surgical resection is not recommended. However an ideal stent does not exist and complications are reported in all series. The correct indication and the good choice of stents are mandatory. An overview on a single centre experience is briefly discussed.
Keywords: Stent; Airway; Palliation
32005Introduction
Stents are increasingly used in the management of various central airway disordres, among these benign and malignant stenoses. In well selected cases airway stents can improve pulmonary symptoms [1], quality of life [2] and even survival [3,4], expecially if stenting is part of a multimodality therapy [5]. Surgical intervention, altough a mainstay of treatment, may not suite patients who present the clinician with advanced malignancy and require only a good palliation. So far silicone [6,7] and metallic [8] stents have been widely used with good results.
Materials and Methods
Since 1989 to 2016 at our Institution 310 stents were deployed. 79% were silicone stent, 13% were Nitinol stent, 1% steel and 7% other stents. Indications were: endobronchial cancer (64%), inflammatory stenosis (17%), external compression (7%), tracheo-esophageal fistula (7%), relapse of endobronchial cancer (2%), temporary stenting (2%) and bleeding in the main bronchi (1%). All the stents were deployed with the rigid scope.
Results
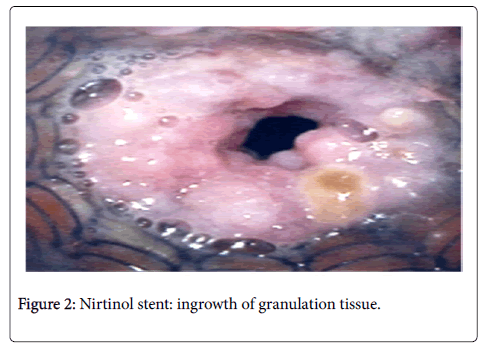
The most important outcome on a patient-basis is that the larger is the diameter of the airway in which the stent is deployed; the better is the result in terms of improved breathing. Complications with silicone stents were: displacement, infection, ageing (Figure 1), granulomas, bleeding, obstruction, chest pain, perforation of the airway. Complications with Nitinol stents were: granulation tissue ingrowth (Figure 2), difficult/impossible removal. One patient died in 1st P.O. day because of pulmonary embolism.
Discussion
In our experience we preferred silicone stents and Nitinol stents. For what silicone stents regards, they represented the first choice for endobronchial cancer and for surgical inflammatory stenosis of lower trachea and bronchi. Nitinol not covered/covered stents were used in case of stenosis of the airway with different diameters or angulation and when migration of previous silicone airway stent was reported.
Conclusion
Endobronchial stenting represents an important advance in the management of inoperable tracheo-bronchial stricture. These patients do not undergo surgery but receive palliation with endotracheal stents, debridement, external beam radiation or brachytherapy [9]. So far there is no single ideal stent for all kinds of stenosis and no data have shown an absolute benefit of one stent rather than another [10,11]. Stents in the airway can improve pulmonary symptoms, quality of life and also survival.
Nitinol stents can be deployed if florid inflammatory tissue is not present in the airway. In this case in fact normal re-epithelization will occur and the endobronchial lumen will remain patent. On the contrary granulation tissues will ingrowth the stent. In case of covered nitinol stents granulomas will arise at the ends of the prosthesis and cause obstruction of the airway. In general uncovered metallic stents are used in patients with predominantly extraluminal compression [12], while silicone-covered metallic stents may be favored in patients with intraluminal tumors. Silicone stents age and the more they remain in site the more they become stiff with recurrent infections. In fact airway colonization tends to be associated with secretion retention [13]. This will require the removal of the silicone stent also after several years.
Acknowledgments
Special thanks to Dr. L. Toniolo who has been the Chief of Thoracic Surgery Unit and Respiratory Endoscopy of Castelfranco veneto Cirty Hospital until 2011.
References
- Eisner MD, Gordon RL, Webb WR (1999) Pulmonary function improves after expandable metal stent placement for benign airway obstruction. Chest 115: 1006-1011.
- Cynthia SC, Litle V, Yun X, Weiser T, Swanson SJ (2008) Airway stents. Ann Thorac Surg 85: S792-796.
- Colt HG (2000) Functional evaluation before and after interventional bronchoscopy. Interventional Bronchoscopy Progr Respir Res 30: 55-64.
- Santos RS, Raftopoulos Y, Keenan RJ, Halal A, Maley RH (2004) Bronchoscopic palliation of primary lung cancer: Single or multimodality therapy? Surg Endosc 6: 931-936.
- Freitag L (2000) Tracheobronchial stents. Interventional Bronchoscopy Progr Respir Res 30: 171-186.
- Madden BP, Datta S, Charokopos N (2002) Experience with ultraflex expandable metallic stents in the management of endobronchial pathology. Ann Thoracsurg 73: 938-441.
- Stockton PA, Ledson MJ, Hind CR, Walshaw MJ (2003)Broncoscopic insertion of Gianturco stents for the palliation of malignant lung disease: 10 year experience. Lung Cancer 42: 113-117.
- Monnier P, Mudry A, Stanzel F (1996) The use of covered Wallastent for the palliative treatment of inoperable tracheo-bronchial cancers. A prospective, multicenter study. Chest 110: 1161-1168.
- Tojo T, Iioka S, Kitamura S (1996) Management of malignant tracheobronchial stenosis with metal stents and Dumon stents. Ann Thorac Surg 61: 1074-1078.
- Marc N, Denis P, Meysman M, Ingeborg C, Walter V (1999) Bacterial colonization of central airways after stenting. Am J Respir Crit Care Med 160: 672-677.
Citation: Colaut F (2017) Airway Stenting: An Overview upon a Single Centre Series. J Tuberc Ther 2: 105.
Copyright: ©2017 Colaut F. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 2923
- [From(publication date): 0-2017 - Jul 05, 2025]
- Breakdown by view type
- HTML page views: 2100
- PDF downloads: 823