Ageing with Spinal Cord Injuries and Preventing Complications
Received: 17-Apr-2018 / Accepted Date: 25-Apr-2018 / Published Date: 28-Apr-2018 DOI: 10.4172/2165-7025.1000389
Abstract
Spinal cord injury (SCI) is relatively common high-cost injury that results in tremendous change in an individual’s life. The spinal cord injury (SCI) affects many body systems (sensory, motor, autonomic, nervous system) and in the clinical picture that reflects as of paraplegia or quadriplegia. In addition to the musculoskeletal system, many other systems are impaired after SCI including cardiopulmonary, integumentary, genitourinary and gastrointestinal system. Psychosocial impact of SCI is just as great as physical impact. This publication defines ageing issues with SCI and highlights changes that occur in different body systems, gives all necessary recommendations, physiotherapy and rehabilitation interventions and describes what it is important to be done to live life not only the best as you can, but also to live healthier life as long as you can.
Keywords: Musculoskeletal system; Physiotherapy; Rehabilitation
Introduction
The young individual with spinal cord injury can experience different reduction in some functional capacities and reserves, and more accelerated ageing development. Patterns and trauma mechanism are different in those in younger patients. Patients in older age who survive spinal cord injury can have important neurological and functional recovery which requires constant active rehabilitation with results in prevention of ageing related complications in SCI.
Health care team, caregivers and individuals need to know all expected changes associated with SCI as the individual ages.
Physical therapist plays a role across continuum of care from the acute hospital through rehabilitation to community reintegration. Physical therapist should use standardized outcome measures as part of their examination and evaluation process. The POC should be individually tailored to the patient’s presentation, concerns and goals. Rehabilitation interventions may be compensatory or recovery based depending of the presentation of the patient. Education is a critical component, and the patient who can no longer perform certain activities should be able to self-direct their care. Rehabilitation is an important cornerstone of recovery. People with SCI no matter at what level, can lead a productive, healthy and high-quality life.
Overview
To define characteristics of ageing in able bodied people-normal ageing
To highlight changes with ageing and SCI in body systems
To explore prevention of ageing related complications in people with SCI.
To define importance of physical therapy and rehabilitation in ageing with SCI
Ageing of able bodied people
Ageing definition: Ageing is “a persistent decline in the age-specific fitness components of an organism due to internal physiological degeneration” [1].
There are many descriptions of the characteristics of ageing through the years. Some authors describe aging of the able bodied people as involving 3 processes. These processes are the physiologic changes of the body, changing social roles, and self-realization. Article had mainly focused on the physiologic ageing changes [2,3].
Over the past decades life expectancy in general population is increased significantly - average life expectancy 1970: 70,8 y/o 2000: 76,9 y/o Women>Men [4].
Physiological aspects of ageing
Cardiovascular changes: Increased blood pressure (systolic and diastolic); A lack of blood vessels elasticity; A decrease in stroke volume capacity.
Musculoskeletal changes: Decrease in muscle mass; Muscle strength declines; Maximum power output; Degenerative joint changes [5].
Neurological changes: Loss of neurons in central nervous system,
Short-term memory is decreased
Speed and of motor activities loss,
Rate of central information processing is getting slower.
Balance in strength is decreased as well as coordination and agility.
Pulmonary system: Elasticity of the lung tissues is decreased.
Flexibility of the chest wall is less and muscle strength decreased.
Changes in vital capacity and maximum voluntary ventilation.
Other systems: The GI tract malfunction in absorption process, dilated colon, rectal fissures, hemorrhoids.
The endocrine system a reduction of hormones, such as human growth hormones and testosterone, immune response systems become less effective.
The integumentary system skin loses elasticity and becomes thinner, skin tears and bruise are evident.
Urinary system loses of glomerular function, renal insufficiency.
Body systems fortunately have huge functional reserve capacity and for most of the people decline in these body systems is not a major nuisance until later stage of life.
Functional consequences of ageing
Over the past years some authors reported that man at age of 65 years can expect to live more than 80% of his remaining life without disabilities. 11% of adults at age 75 to 84 years require assistance with activities of daily living. Percentage of the elderly individuals who can expect to live in an institution is 5%. Percentage of the individuals with 85 years and older who requires some assistance with ADL is 23% [6]. At age 85 years, up to 60% of individuals may need assistance with instrumental activities of daily living (IADL) [7].
Ageing with SCI
Majority of individuals with SCI are young at the time of their injury and as a result, they experience a various reductions of the functional capacities and reserves.
That can lead to premature and accelerated process of ageing, which is affecting as well some body systems (cardiovascular, musculoskeletal, and respiratory). Consequences are often that, individual often requires assistance with ADL [8].
Ageing concerns and health risks
Health risks include: High blood pressure,
Cholesterol disorders,
Diabetes mellitus,
Overweight/obesity,
Infections, primarily pneumonia from pressure sores and Bladder cancer.
Individuals with SCI are facing with overweight and obesity as they age. This study was done on 162 patients with SCI and as we can see 27.5% of the patients are overweight and 5% are obese, but in general population with SCI this percentage goes up to 75 %. These things become more evident as individual ages [9,10].
Demographics and etiology
Approximately 11.000 new cases of SCI occur in the US every year. Between 225,000 and 228,000 individuals with SCI are currently living in the US [11].
The age at the injury over the past decades has steadily increased. In the 1970s, the average age of the injury was 28.7 years. Between 2005 and 2008 this increased to 37.1 years. In recent years that increased to 42.4 years. Reason of this might be due to the ageing of the population (life expectancy in able bodied people is increased) and falls as cause of injury are more common. The majority of individuals with SCI are male (78.3%), versus 21.7% female [12].
Life expectancy
Life expectancy has increased over the years but is still less than that for individuals without SCI. Factors that influence life expectancy are age at onset and level and extent of neurological injury. Individuals who suffered incomplete neurological SCI have a longer life expectancy than those with a complete injury, and person with injuries that are more caudal also have greater life expectancy.
A 20 year old healthy individual without a SCI has a life expectancy of additional 58.6 years (total life expectancy 78.6 years). A person who experiences a SCI at age 20 with a neurologically incomplete injury has a life expectancy of additional 52.6 years, a person with complete paraplegia an additional 45.2 years, low tetraplegia (C5-C8) an additional 40.0 years and a person with high tetraplegia (C1-C4) an additional 35.7 years. Mortality rate is also significantly higher during the first year after injury [13].
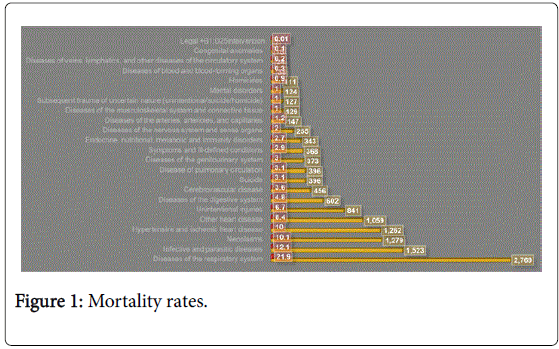
Mortality rates
Development of cardiovascular and respiratory complications are primary causes of death for the persons with long term spinal cord injury. These conditions now exceed urinary complications which were previously one of the primary causes of death (Figure 1) [14].
Age related complications in SCI
Cardiovascular system: One of the primary causes of morbidity and mortality. Some of the risk factors include; sedentary lifestyle, overweight/obesity, lipid disorders, coronary artery disease (CAD) and diabetes/glucose intolerance [15]. Sedentary lifestyle and physical inactivity are big risk factors in developing CVD, Perceptually 22.4% of deaths in SCI are from coronary artery disease (CAD) (Table 1). Individuals with SCI who have some cardiovascular conditions are twice as likely to die [16].
| Gastrointestinal complication | ||
|---|---|---|
| Decline in gut motility (especially colon and rectum) | Problems associated with GI tract dysfunction increase with age after SCI | The frequency of GI complications and problems is greatest in individuals aged 60 years or older or whose injuries are at least 30 years old. |
| Decreased acid secretion. Increased water absorption from colon |
Seventy four percent of patients with SCI develop hemorrhoids, 43% develop abdominal distention, 43% experience autonomic dysreflexiarelated to the GI tract, and 20% develop difficulty with bowel evacuation. Higher incidence of colorectal cancer [12]. |
|
Table 1: Age related complications in SCI.
Recommendations: Primary care physician should be involved when cardiovascular problems are more evident.
Weight monitoring must be regularly, blood pressure, diet, physical activity, reduction of smoking and alcohol consummation [17].
Respiratory system complications: Ventilatory failure reduced ability to take deep breaths and worsened by tobacco use, pneumonia, poor secretion management or atelectasis. Sleep apnea occurs more often in SCI than the general population.
Recommendation: Assessment of the lung vital capacity and respiratory function must be periodical, especially with higher lesions, cough assistance, breathing exercises and encourage cessation of smoking.
Urinary system complications: Urinary bladder - less storage capacity. In women “urethral incompetence”, more frequent urination, increase residual urine, urinary infection (↑ after 60 y), slightly increased risk of bladder cancer and urinary incontinence.
Kidney decline in kidney function, especially after age of 40-50 years. Exacerbated with pre-existing kidney dysfunction, males with SCI have a lower risk of prostate cancer due to impaired testosterone levels compared to the general population.
Recommendations: Urinary tract deterioration must be screened yearly, then later every two years.
Musculoskeletal system complications: Muscle mass reduction and loss of strength reduction occurs, flexibility and endurance is changed, bones become osteoporotic and degenerative signs in the articular cartilage are present (often related to various joint physical stresses throughout life), overuse syndrome (OS); and bone fracture (shoulder, arm, wrist).
Recommendations: equipment evaluations and upgrade must be regular and long-term, constant education, physiotherapy, occupational therapy and exercising program.
Nervous system complications: Nerve entrapment problems are often, (63% of paraplegic individuals have entrapment neuropathies). Around two thirds of people with SCI have compressive neuropathies in the upper extremities, and 50% with median neuropathy. Around 25% have neuropathy bilaterally (upper extremities) [18].
Recommendations: Health care providers needs to assist and review of medications when is necessary.
Age related skin complications in SCI: Collagen is decreased, skin elasticity is changed, decubitus ulcer occurs and decreased circulation reduces blood flow. Around 15% of individuals with SCI develop a decubitus ulcer and 20 years post-SCI 30% develops decubitus ulcer.
Recommendations: repositioning/pressure relief manoeuvres, cushioning, skin monitoring, self-inspection and education.
Gastrointestinal system
Recommendations: Regular bowel routine must be done on appropriate time. Rectal stimulation is necessary as well as a high fiber diet. Fluid intake must be good and when is necessary use of laxatives and similar agents in Table 2 [19].
| Endocrinology complication | ||
|---|---|---|
| Diabetes mellitus | Four times higher than in general population | 22% have diabetes, 34% glucose intolerance [4]. |
| Low growth hormone and testosterone [13] | Low total serum testosterone occurring at an earlier age in men with SCI and with age-related decreases progressing at a faster rate. | Reduced capacity for cellular repair. Reduced capacity for maintaining lean muscle mass and strength. Prolong healing and soft-tissue repair following injuries. |
Table 2: Endocrine system.
Endocrine system
Recommendations: Education is important to balanced diet and to maintain good body weight.
Mental health changes: Function of the brain changes over time as individuals age, and that is not different with individuals with SCI, but some cognitive changes can be associated with SCI related to concomitant traumatic brain injury and sleep apnea.
People with SCI, aged between mid-twenties to late forties, are more likely to have depression comparing to those who are younger or older than that [20].
Some younger people can easier adapt to certain life changes with SCI, and older people can adapt psychologically quicker. As ageing process continues, some physical limitations can be present and that can lead to dependency on carers.
Once symptoms and signs of the stress and anxiety occur health care providers need to support people with appropriate manner. They need to help them to maintain social connections, physical activity and hobby or occupation.
Psychosocial, caregiver problems and falls prevention: Activities may need to be modified as ageing occurs. Adaptive equipment or technology can help to reach independence. Family and carers mental and physical health should be regularly assessed. It is not always recommended that family member or a spouse is taking care of the patients with SCI.
Falls can increase with age. It is important to take a full history and assessment must be done with clinical testing and physical assessments. We need to identify all factors, related to ageing that can increase the risk of falling [20].
Physical therapy and rehabilitation efforts in ageing with SCI.
The overarching goal of physical rehabilitation is for the patient to become as independent as possible and to achieve the functional mobility necessary for everyday living, work and recreation.
Good rehabilitation is essential for recovery, longer and healthier ageing with SCI. Nowadays, rehabilitation in rehab center has been reduced which case wasn’t before. Rehabilitation with the 4-6 months was not unusual in the 70s and 80s. Today, patients are send home in some cases after 45 days post injury. Reason is mainly because today rehabilitation advanced more. Focus is more to reach independence for injured individuals with SCI, and this created longer life expectancy, but also created more negative impact on mental health and physical inactivity which resulted in higher percentage of overweight and obesity as it was described before in this book. Patients cannot expect to fully meet the challenges of their life if they haven’t been working enough on shape by a good PT, and other members of the rehabilitation team.
The spinal cord injury rehabilitation team includes many skilled professionals following: neurologist and neurosurgeon, orthopedist/ orthopedic surgeon, physiatrist and rehabilitation specialists, primary care physician, urologist, internists, physical therapist, occupational therapist, speech and language pathologist, psychologist/psychiatrist, recreational therapist, social workers, dietitian and other specialty doctors.
Family members and careers are very important in rehabilitation process and they can give physical and emotional support in the following days, months, and years after the injury.
This chapter describes what is important to do for better ageing with SCI from physical therapy and rehabilitation perspective (what we need to know about acute phase of the recovery, why is important to set goals, how we can improve patients emotional system, what are main rehabilitation procedures, importance of education and how to help patient to achieve independence in ADL and to maintain certain level of functional and mental recovery to be able to work, have hobby or sport activities to have higher quality of life.)
Physiotherapy in acute stage of recovery
Respiratory care: Respiratory care will vary according to the level of injury and individual respiratory status. Primary goals of management include ventilation increased effectiveness of cough, and prevention of chest tightness and infective substitute breathing patterns.
Individuals with cervical injuries at and above C5 often require ventilator support using an intermittent positive pressure ventilator (IPPV).
It’s important to do deep-breathing exercises for diaphragmatic breathing, glossopharyngeal breathing (for patients with high level cervical lesions who are dependent on a mechanical ventilator, as well as for the patients who are mid to high cervical level injury, who are not dependent on mechanical ventilation. Air shift maneuver can be done (this technique provides patient with an independent method of chest expansion).
Similar to the other muscles strength training can improve respiratory muscles strength and endurance. Inspiratory muscles can be trained using relatively inexpensive hand held devices, which increase the resistive or threshold inspiratory load on muscles of inspiration (photo1. Inspiratory muscle trainers).
Patient who are not able to produce a functional cough should be thought to perform a self-assisted cough. Abdominal binder may improve respiratory function and coughing. Manual stretching and compliance of the thoracic wall can be facilitated by manual stretching chest wall muscles in supine.
Skin care: Prevention is the most effective for skin care, this entails positioning, consistent and effective pressure relief, skin inspection and education.
Early strengthening and ROM: ROM exercises are recommended to be completely daily (exceptions are those that are contraindicated or require selective stretching). Depending on the location of the SCI some motions can be contraindicated (motions of the trunk and some motions of the hip).
Early mobility interventions: Early mobility interventions can be done once radiographic findings have established stability of the fracture site, or early fracture stabilization methods are completes the patient is cleared for upright, functional activities. The patient will typically experience, symptoms of postural hypotension (dizziness, nausea, ringing in the ears, loss of vision, loss of consciousness).
Education
Living with a SCI requires significant adaptations and changes on the part of the patient and his or her family.
Patient must fully understand all the consequences of the injury. Patient and family/caregiver education should begin early.
Later in the recovery process it may be helpful to have the patient to meet individual with long-standing SCI.
For example person with and ASIA A T2 SCI will be able to realistically demonstrate how to transfer from the bed to a wheelchair to a person recently injured who is undergoing rehabilitation. This person may also be able to discuss the impact of SCI on everyday life in a way a physical therapist could not.
An important part of rehabilitation involves planning for discharge and community reintegration. Consideration must be given to multiple issues, including accessible housing maintaining functional skills and physical fitness, employment or further education and methods for involvement in desired social or recreational activities. Each of these issues must be addressed early and continued throughout the course of rehabilitation in consultation with the patient, family and appropriate team members.
Without education patient will not be able to make informed decisions regarding their care or informed choices regarding community reintegration.
Goals in rehabilitation and ageing with SCI
Goals should describe what are the meaningful and important things for the individual with SCI. this can increase motivation and help patient to reach his autonomy.
In the early stages people with SCI can’t fully understand all consequences that SCI brings, but once they adapt it is important to educate patient and discuss potential functional goals, where patient has to be encouraged to have his/her own goals as well.
Goals which are long termed are always based on focus on activity and social participation, but not body structure and function impairments. Goals should be specific in what patient will achieve. All issues and levels must be documented.
For some patient who suffered high level cervical SCI and who can’t perform a lot of activities, goals should be directed towards patients instruction for a caregiver to perform task appropriately.
• Example of general goals and outcomes with SCI.
• Airway clearance is improved
• Aerobic capacity is increased
• Integumentary integrity improved
• Independence in ADL
• Independence in wheelchair propulsion
• Independence in self-directing care etc.
Emotional system
Through the years clinicians have known that motivation can improve recovery from SCI and that symptoms of depression can delay functional recovery. In recent years people described with neuroscientific evidence how motivation promotes recovery from SCI. All these information tells us that we as health care providers have to work on patient’s emotional system same as on his physical impairments.
Physiotherapy interventions
The overarching goal of physical rehabilitation is for the patient to become independent as possible and to achieve the functional mobility necessary for everyday living, work and recreation.
We can achieve independent mobility on two ways: to use new movement strategies for compensation for neuromuscular impairments) or to use neuromuscular system to achieve certain tasks with movements that are similar to that before the injury.
Compensation means usage of alternative or a new strategy of movement or using technology to compensate for neuromuscular impairment to achieve certain daily task.
Recovery of function is the restoration of the neuromuscular system (efforts to try to perform motor tasks in the same manner as it was before SCI).
So improvements in body structure/function impairments, the ability to perform activities that are important to individual can be achieved through the interventions that are based on compensatory strategies, restorative strategies, or a combination of the two.
Strengthening
Strengthening innervated musculature is an important component of the physical therapy POC. Key UE muscles to strengthen include serratus anterior, latissimus dorsi, pectoralis major, rotator cuff muscles, and triceps brachii. These muscles are important for independence transfers.
Initially strengthening exercises can be done daily during early rehabilitation. A variety of methods can be used to implement strengthening exercises: pulley systems, free weights, elastic bands, weight cuffs. With very weak muscles (grade -<2) strengthening can be performed in gravity-reduced positions. On a powder board or with active assistive ROM. Strengthening can be done in a functional postures as well.
Cardio vascular/endurance training
As for the able bodied people, cardiovascular training has important health benefits for people with SCI. A number of research studies have shown that endurance training can improve aerobic fitness. Upper extremity-based exercises. Such as arm ergometry, wheelchair propulsion, and swimming are the most common method of aerobic training. Functional Electrical stimulation - induced cycling or walking is also an effective means of improving cardiovascular fitness.
Bed mobility skills
Bed mobility skills are necessary to promote independence in functional mobility. Bed mobility skills include rolling, transitioning supine to/from sitting on the edge of the bed and LE management.
Independence in these skills is also necessary for dressing positioning in bed, and skin inspection.
Sitting balance: Are important for transfers, dressing, and wheelchair mobility. Sitting posture will vary with lesion level. Patient with low thoracic lesions can be expected to sit with a relatively erect trunk. Individuals with low cervical and high thoracic lesions maintain sitting balance by forward head displacement and trunk flexion.
Transfers: There are 3 components to the sit-pivot transfer (example bed to/from wheelchair in a seated position): preparatory phase, lift phase, descent phase. During the preparatory phase, the trunk flexes forward, leans laterally, and rotates toward the trailing arm. The lift phase starts when the when the buttocks lift off the sitting the sitting surface and continues while the trunk is lifted hallway between the two surfaces. The descent phase denotes the period when the trunk is lowered to the other seated surface from the halfway point until the buttocks are on the other surface.
There are 3 basic floors to wheelchair techniques: backward approach, forward approach, and sideways approach.
Activity based upper extremity trainings
For people with a cervical SCI the recovery of UE function is a primary goal. Interventions aimed at improving functional use UE have primary been compensatory in nature. For example, patient with active wrist extension are thought how to manipulate and pick up objects using a grasp, use the hand as a hook, and use different type of orthoses, to feed themselves. More recently, researches have begun to explore the use of massed practice interventions to promote functional recovery and corticomotor and spinal reorganization.
Locomotor training
To be able to walk is a common goal for most individuals with SCI. There are a lot of factors that influence success or failure in attaining this goal.
Patient must have adequate muscle strength, alignment of the posture, range of motion, and adequate cardiovascular endurance to become functional ambulators. Becoming functional ambulatory following a complete SCI is very difficult. Walking with orthoses and assistive devices is slower and requires more energy than walking before injury. Many individuals with motor complete SCI who learn to walk with these devices may not continue walking once they stop rehabilitation. Patient with motor incomplete SCI (Asia C and D) are more likely to regain functional ambulation skills than those with complete and sensory incomplete injuries.
Health and wellness
Just as with people without SCI, regular exercise is an important part of a healthy lifestyle. Patient should be provided a comprehensive home exercise program (HEP) that incorporates stretching, balance, aerobic and strengthening exercises. Aerobic exercises such as UE ergometer should be done 3-5 days in a week for a total 20-60 minutes per session. Strengthening exercises 2-4 days a week, intensity 8-10 repetitions. When developing the exercise program attention should be paid to the unique precaution associated with people with SCI such as the possibility of overuse injuries (particularly in the shoulders), AD, thermal deregulation and exaggerated heart rate response to exercise.
Neurotechnologies
People with SCI also benefit from recent advances in neurotechnologies designed to improve function and quality of life. Neurotechnologies can fall into four main areas: Neuromodulation (use of electrical stimulation, to improve control of an intact portion of the nervous system), neural prosthesis (use electrical stimulation to replace or improve function of a paralyzed or weak limb), neurorehabilitation (applying technologies to promote normal recovery of impaired body functions) and neurosensing and diagnostics (technologies to monitor the nervous system or diagnose condition).
Brain computer interface devices (BCI) acquire brain signals (electroencephalogram EEG) and translate them into commands that are relayed to output devices that perform an action such as control a mouse on the computer screen. People with high cervical SCI with little motor function are able to use BCI to use a computer, play videogames, potentially to drive a power wheelchair and a control a robot.
Robotic devices can be used during LT to move the Les in stepping pattern to promote recovery of walking ability. Exoskeleton robots are been developed that will allow people with complete SCI to walk with assistance from the robot. These examples offer existing ways of how technology is being used and glimpses of the future of rehabilitation that provide exciting opportunities to increase activity levels, improve social participation and enhance the quality of life for people with SCI.
We need to use equipment and technology to improve function, we also need to use technology to open up peoples worlds, we never lived in a world like today where technology can be in home and finally we need to look at the employment and other important domains.
Professional rehabilitation and SCI
Importance of work for people for people with SCI is very important. Not only because they can get health insurance, income and other benefits but also to enhance life satisfaction, to interact to with others and self-esteem. There are certain findings in research that people who are occupied and employed after SCI have more chance to live longer and healthier than those who are not working [20].
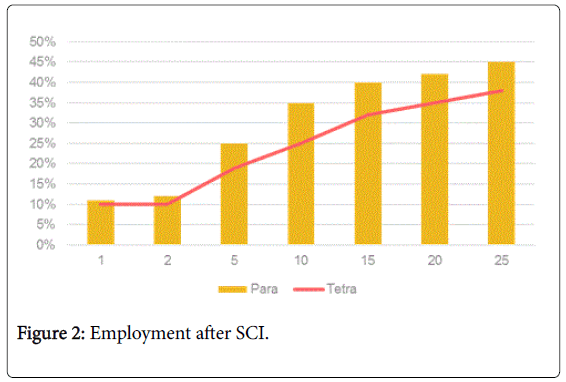
Percentages of employment in recent years are improving but it still takes at least 25 years after injury to reach 40% of the employment for the individuals with SCI. There are minor differences between paraplegia and tetraplegia. Persons with SCI have more barriers (that are not only physical) to overcome to be able to work than those without disabilities (Figure 2).
Health care providers must prepare patient physically and mentally to be able to work something that he is able with his impairment. This can be one of the patient’s long-term goals, but must be realistic and achievable.
On the table below we can see that number of unemployed people with SCI is becoming less as years go by after the injury, but there is still big difference between working population with SCI (Table 3).
| Post-Injury Year | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Occupational Status | 1 | 5 | 10 | 15 | 20 | 25 | 30 | 35 | 40 | Total |
| Working | 2,963 | 2728 | 2076 | 1556 | 1290 | 1035 | 747 | 377 | 75 | 12847 |
| Homemaker | 400 | 263 | 178 | 107 | 67 | 52 | 58 | 25 | 6 | 1156 |
| On-the-job-training | 32 | 19 | 8 | 3 | 6 | 1 | 0 | 0 | 0 | 69 |
| Sheltered Workshop | 13 | 5 | 7 | 2 | 1 | 3 | 0 | 0 | 0 | 31 |
| Retired | 1662 | 1064 | 652 | 439 | 316 | 316 | 391 | 302 | 88 | 5230 |
| Student | 3662 | 2014 | 505 | 176 | 96 | 39 | 14 | 9 | 0 | 6515 |
| Unemployed | 13149 | 6233 | 3623 | 2321 | 1745 | 1214 | 818 | 378 | 76 | 29557 |
| Other. Unclassified | 1679 | 707 | 473 | 348 | 286 | 274 | 257 | 101 | 17 | 4142 |
| Unknown | 600 | 265 | 136 | 85 | 44 | 22 | 14 | 2 | 0 | 1168 |
| Total | 24160 | 13298 | 7658 | 5037 | 3851 | 2956 | 2299 | 1194 | 262 | 60715 |
Table 3: Number of unemployed people with SCI.
NSCISC, annual report 2016
Most of the people with SCI who had to work far from the house after they had injury and retired after some years, say that they find their jobs increasingly demanding. Most of them who have jobs like this retire in their fifties because their jobs become physically difficult, but mentally they feel too young to retire. In that stage majority are saying that they would like to have a nice part time job that they can do from home, because they don’t feel completely happy not working.
Individuals with SCI who are working still in their fifties claim that they are more tired because they are working, but they don’t have any other difficulties related to work.
Tiredness can be related because they have more things to do in one working day than able bodied people. Basically their working day starts a lot earlier, they make sure to have bowel and bladder care, moving takes more time, which means to get up in 4 in the morning and couple of hours is just to get to the door. This is why employment of this population must be adjusted.
Conclusion
Process of ageing has more severe negative impact on people with SCI comparing to able bodied people.
Development of medical complications and loss of social role are leading cause of depression and social isolation.
Many of age related negative factors are preventable and should be recognized on time.
We need to use evidence that is available.
The clinical practice guidelines that are produced by the consortium for spinal cord medicine should be used by everybody, that’s the best evidence that we have now.
We need push for physical rehabilitation, advocate for more intensive rehabilitation, focus on independence, learn new skills and behavioral strategies and do our best to prepare these patients to contribute and be occupied for better quality of life.
References
- Rose MR (1991) Evolutionary Biology of Aging. Oxford University Press, New York, USA.
- Menter RR, Hudson LM (1995) Spinal cord injury clinical outcomes. Stover S, edtn The Model Systems. Aspen Pubs, New York, USA.
- Rina R (2009) Aging with a Spinal Cord Injury. University of Washington, USA.
- Clark GS, Siebens HC (1998) Geriatric rehabilitation. Rehabilitation Medicine: Principles in Practice. 3rd ed. Lippincott-Raven: Philadelphia, USA.
- Kennedy J, LaPlante MP, Kaye HS (1997) Need for assistance in the activities of daily living [abstract]. Disability Statistics 18: 1-4.
- Clark GS, Siebens HC (1998) Geriatric rehabilitation. Rehabilitation Medicine: Principles in Practice. 3rd ed, Lippincott-Raven, Philadelphia, USA.
- HitzigSL, TonackM, Campbell KA, McGillivray CF, Boschen KA, et al. (2008) Secondary health complications in an aging Canadian spinal cord injury sample. Am J PhysMed Rehabil 87: 545-555.
- NSCISC (2016) National Spinal Cord Injury Statistical Center. Complete public version of annual report 2016: 90DP0011.
- Sabour H, Javidan AN, Vafa MR, Shidfar F, Nazari M (2011) Obesity predictors in people with chronic spinal cord injury: an analysis by injury related variables. J Res Med Sci 6: 335-339.
- De Vivo MJ, Chen Y (2011) Trends in new injuries prevalent cases and ageing with SCI. Arch Phys Med Rehabil 92: 332-338.
- Susan B, Sullivan O, Schmitz TJ, Fulk GD (2014) Physical Rehalitation. 6th ed. Traumatic SCI Pg: Dempgraphics and etiology.
- Groah SL, Nash MS, Ward EA, Libin A, Mendez AJ, et al. (2011) Cardiometabolic risk in communitydwelling persons with chronic spinal cord injury. J Cardiopulm Rehabil Prev 31: 73-80.
- De Vivo MJ, Kartus PL, Stover SL, Rutt RD, Fine PR (1989) Causes of death for patients with spinal cord injuries. Arch Intern Med 149: 1761-1766.
- Ageing with Spinal Cord Injury, Hannah Withers, Research Assistant, Rehabilitation Studies Unit, Sydney Medical School Northern, The University of Sydney, Australia.
- Davidoff G, Werner R, WaringW (1991) Compressive mononeuropathiesof the upper extremity in chronic paraplegia. Paraplegia 29: 17-24.
- Charlifue S, Jha A, Lammertse D (2010) Aging with spinal cord injury. Phys Med Rehabil Clin N Am 21: 383-402.
- Playford ED, Siegert R, Levack W, Freeman J (2009) Areas of consensus and contraversy about goal setting in rehabilitation. Clin Rehabil 23: 334-344.
- Sawada M, Kato K, Kunieda T, Mikuni N, Miyamoto S, et al. (2015) Function of the nucleus accumbens in motor control during recovery after spinal cord injury. Science 350: 98-101.
- Northwest Regional Spinal Cord Injury System. Department of Rehabilitation Medicine, University of Washington, USA.
Citation: Zetica T (2018) Ageing with Spinal Cord Injuries and Preventing Complications. J Nov Physiother 8: 389. DOI: 10.4172/2165-7025.1000389
Copyright: © 2018 Zetica T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4591
- [From(publication date): 0-2018 - Nov 22, 2025]
- Breakdown by view type
- HTML page views: 3675
- PDF downloads: 916