Again, Dental Impaction and Infection, What to do?
Received: 06-Mar-2017 / Accepted Date: 24-Mar-2017 / Published Date: 31-Mar-2017 DOI: 10.4172/2161-119X.1000300
Keywords: Dental impaction; Wisdom teeth; Pericoronatis; Dental infection; Conservative treatment; Surgical extraction; Surgical exposure; CBCT
254790Introduction
GP dentist, Orthodontist and Oral surgeon specialist are frequently faced with teeth eruption anomalies during the eruption phase of the adult dentition as tooth impaction and related infection.
What are Impacted teeth?
• Impacted teeth are classically defined as retained in the maxillary or the mandibular jaws beyond the normal date of eruption.
• Impaction teeth are considered ectopic as beyond the normal site of eruption.
• Impaction teeth are surrounded by the follicular bag without communication with the oral cavity.
Impacted teeth are also descripted as unerupted teeth.
Some other authors describe this situation as Teeth retention when they are considered:
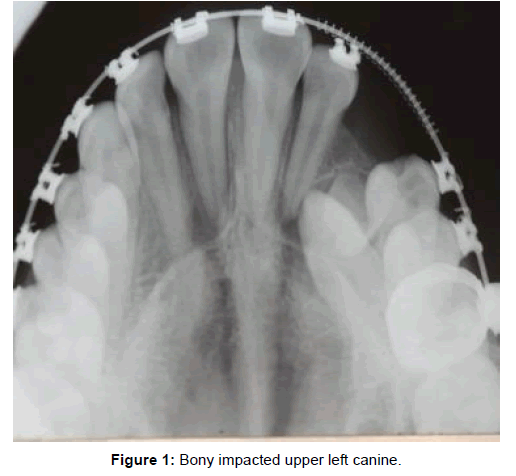
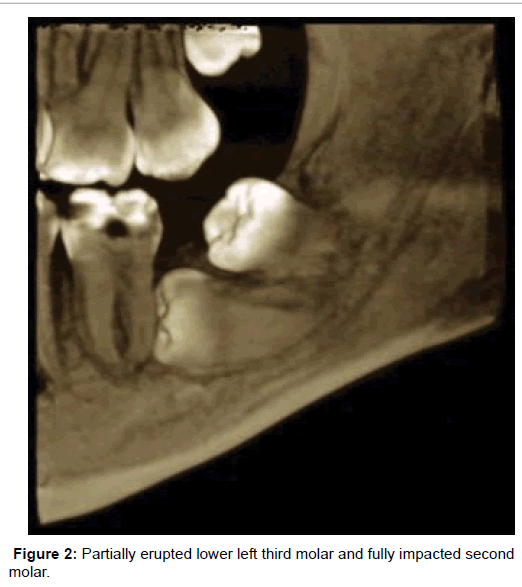
• Bony Impacted : Physiological or pathological as intra osseous.
• Partially Erupted: Sub mucosal or soft tissue impaction (Figures 1 and 2).
What are the Causes of Impacted Teeth?
• Failure of a tooth to erupt into the oral cavity after the complete development of its root.
• Related pathology (mesiodens, odontoma, cyst, tumor).
What is the Impacted Teeth Geometry?
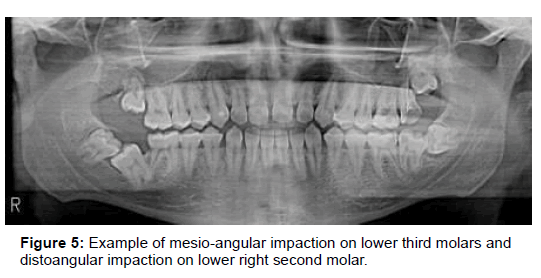
It is the direction of Impaction of the tooth that can be (Figure 5):
1. Mesio angular
2. Disto angular
3. Vertical
4. Horizontal
How to Confirm a Positive Diagnosis of an Impacted Tooth?
These steps are required:
• Proper clinical dental examination (chief complain, missing teeth).
• Dental history (episodes of Pain, swelling and infection).
• Medical update (age of the patient).
• Diagnostic radiological aids (or sudden radiological discovery).
• Histological aids like biopsy in case of related odontogenic or non odontogenic Cyst or Tumor.
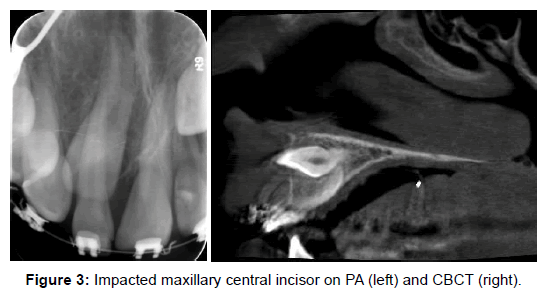
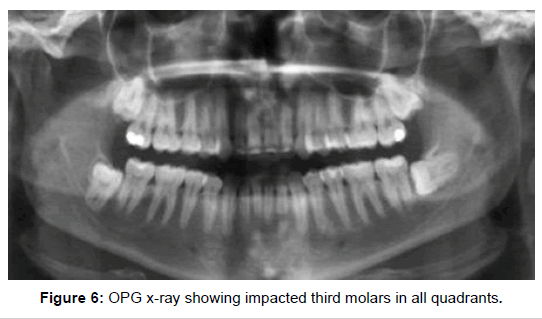
The Diagnostic Radiological Aids like Two D Dimensional X-Ray as
• Intra oral peri apical radiograph
• Occlusal radiograph
• Panoramic view
These 2 D X-rays are acceptable tools but not accurate 100% (Figure 6).
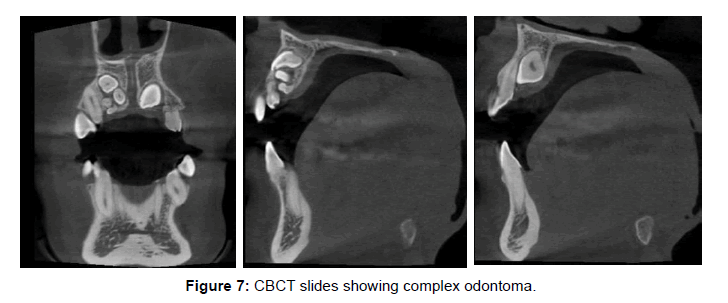
So Three D dimensional X-ray is needed as:
• CT scan but they are costly with high radiation doses.
• CBCT has less radiation doses, are easier and more comfortable for patient (same like OPG Machine), also cheaper and better image quality (Figure 7).
The Advantages of the CBCT Views are
• Location of the Impaction tooth in all directions.
• Relationship with the adjacent teeth and the anatomical landmarks.
• Extension of the cyst or the tumor lesion.
• Cortical bone quality and expansion.
• Location of anatomical landmarks (Inferior alveolar nerve- IAN, Maxillary Sinus, Mental Foramen–MF, Naso-Palatin artery, Subortbital Nerve….)
The Clinical Applications of the CBCT for a Predictable Surgical Removal are
• Impact of the impaction on the adjacent teeth: blocking or displacing eruption.
• No interference of superimposed anatomical structures.
• Information about size, shape and position of the impaction (Crown/Roots).
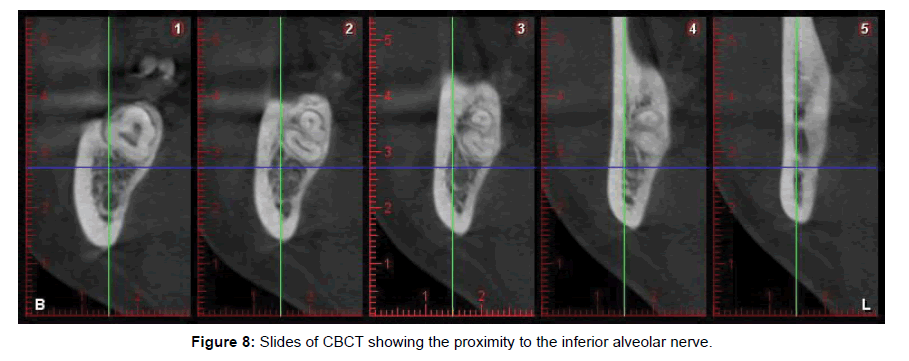
• Information about root resorption, root tips with IAN or MF for nerve injury inquiry!
Which Guidelines to Recommend for Removal of Impacted Teeth?
• Scenarios where is not advisable: Asymptomatic, deeply bone seating and risk of anatomical damage.
• Scenarios where is advisable: Orthognatic surgery indication and Pericoronatis.
• Strong indications for removal: Unrestorable caries, frequent Pericoronatis, cellulitis, and cyst related [1,2].
What are the Clinical Indications for Removal of Wisdom Teeth? [3]
• Unrestorable caries.
• Non treatable pulpal +/- apical pathology.
• Cellulitis or abcess.
• Internal or external resorption of the tooth or the adjacent one.
• Fracture of the tooth.
• Follicle pathology as Pericoronatis, cyst or tumor.
• Periodontally involved Wisdom or associated with periodontally involved adjacent tooth.
• Before maxillary molar retraction for Orthodontic treatment.
• To facilitate restoration of adjacent tooth as class II or Crown in second molar.
• Prophylactic Removal for medical or surgical conditions:
• Patient with risk of bacterial Endocarditis.
• Patient planning for Organ Transplant.
• Patient planned for Chemotherapy.
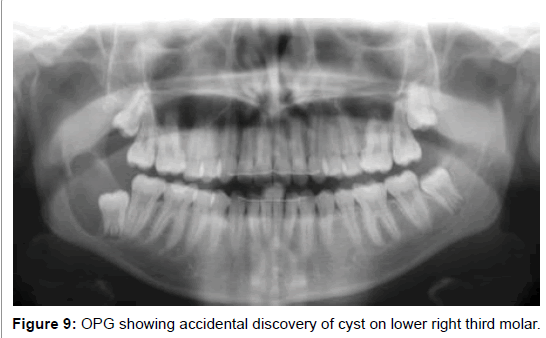
• Patient to receive radiotherapy (Figures 8 and 9).
When Two EPISODES of PERICORONATIS is confirmed in a year, an appropriate indication for Surgical Removal is considered.
What is the Frequency of Impaction of The Permanent Teeth?
Impaction teeth from the most frequent to the least frequent are [4]:
• Lower third molars
• Upper third molars
• Maxillary canines
• Maxillary and mandibular premolars
• Maxillary incisors
• Mandibular canines
• Mandibular incisors
• Upper and lower first molars followed by second molars.
What is the Management of Impacted Teeth?
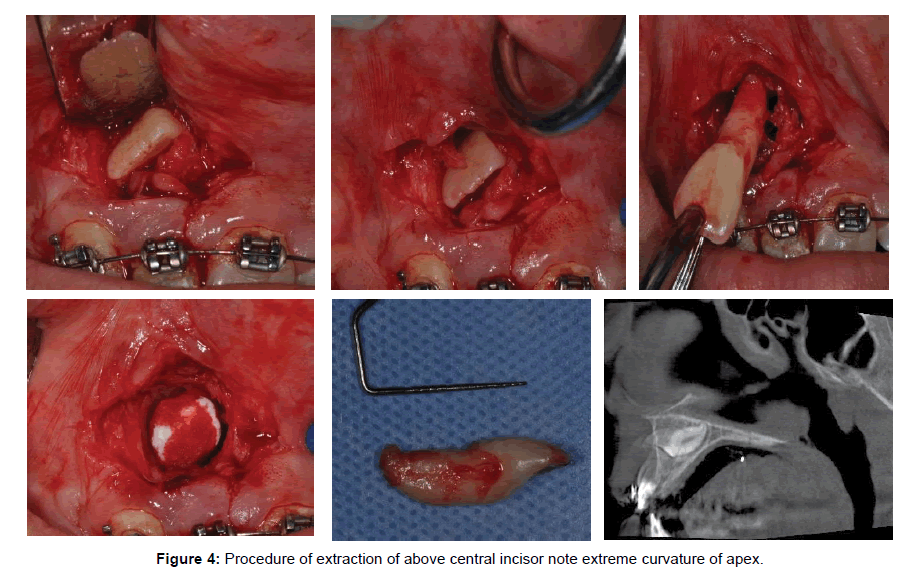
After a positive diagnosis of an impacted tooth is confirmed, a prediction Prognosis for conservative or surgical removal for this unerupted tooth will be decided. Options will be the following:
• Surgical removal.
• Surgical exposure and orthodontic forced eruption.
• Abstention or Observation.
Informed consent should be explained and signed by the dental surgeon, the patient and the witness staff. Common and serious per and post-operative complications should be explained to Patients. Surgical Treatment will be decided under local or general anesthesia [5].
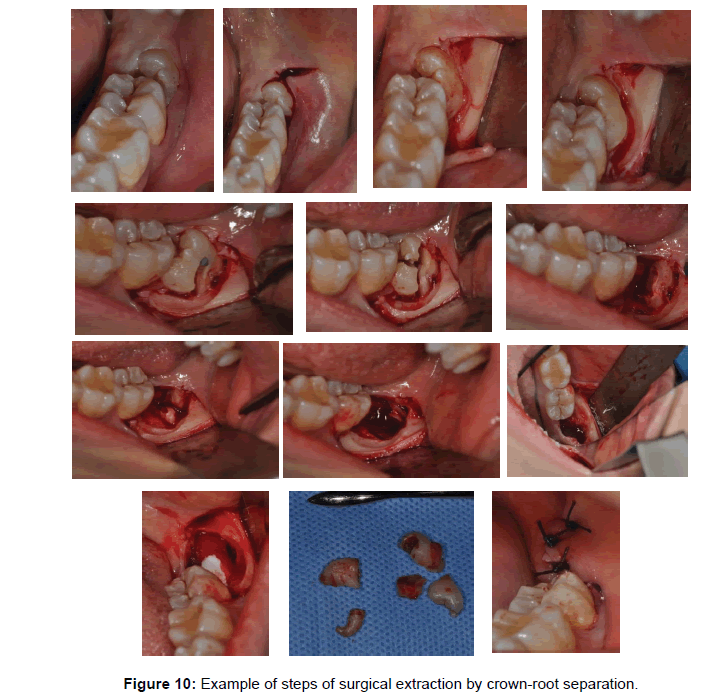
Surgical exposure and orthodontic Traction decision will be a joint venture with the treating Orthodontist. Some considerations should be taken into account as the available space or inadequate to reposition the impacted tooth into position. Also to decided which surgical technique to select as closed or open orthodontic traction. Adequate periodontal tissue quality at final tooth positioning should be, considered for healthy periodontium (Figure 10).
Confirm the diagnosis of the impaction tooth. Follow the guidelines for decision making in surgical removal or No. Diagnostic radiological and histological aids are to be used when needed. Be aware when to Figure 9: OPG showing accidental discovery of cyst on lower right third molar. perform surgical removal or the need to refer to Oral surgeon. Signed consent, surgical procedure and post-operative possible complications should be explained to patient.
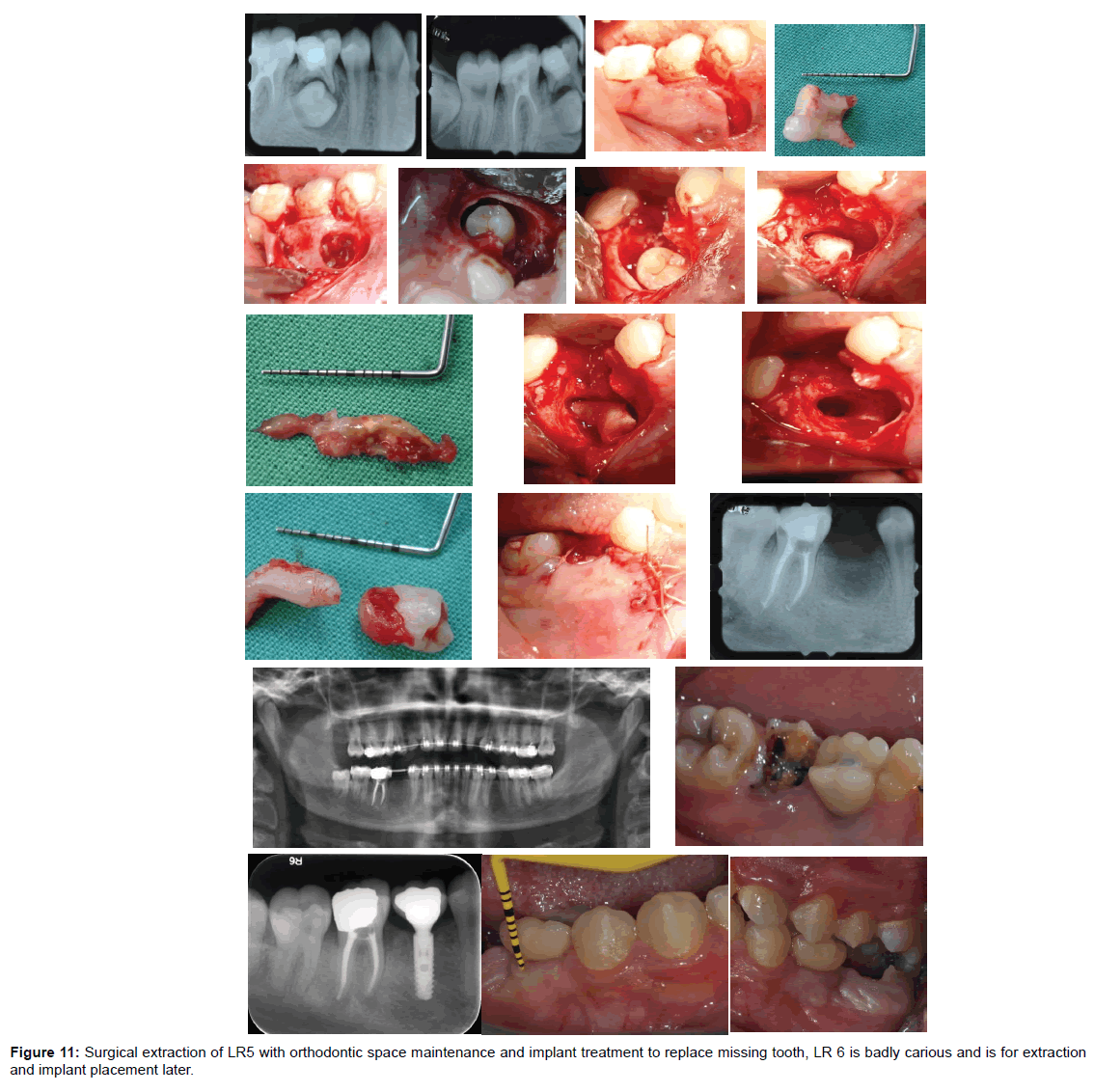
Orthodontic and surgical cooperation are need for the impacted teeth to be reposition in original site (Figure 11).
References
- McArdle LW, Renton T (2012) The effets of NICE guidelines on the management of third molar teeth. Br Dent J 213: E8.
- Abboud R (2014) The usefulness of CBCT in the assessment of teeth and teeth impactions: A clinical appraisal. JLDA 49: 1.
- Greenwood M, Corbett I (2012) NICE guidlines for the removal of wisdom teeth: Appendix 5. Dental Emergencies, Blackwell Publishing Ltd.
- Bourzgui F, Sebbar M, Abidine Z, Bentahar Z (2012) Management of dental impaction. Orthodontics-basic aspects and clinical considerations. INTECH, pp: 219-246
- Scottish Intercollegiate Guidelines Network (2000) Management of unerupted and impacted third molar teeth. A national clinical guideline. Evidence Based Dentistry 2: 44-45.
Citation: Mohamad K (2017) Again, Dental Impaction and Infection, What to do? Otolaryngol (Sunnyvale) 7:300. DOI: 10.4172/2161-119X.1000300
Copyright: © 2017 Mohamad K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7235
- [From(publication date): 0-2017 - Jul 03, 2025]
- Breakdown by view type
- HTML page views: 6377
- PDF downloads: 858