Advent of Surgical Navigation in Oral and Maxillofacial Surgery and Application of Different Navigational Systems in Various Surgical Procedures: A Review
Received: 02-Jan-2018 / Accepted Date: 11-Jan-2018 / Published Date: 18-Jan-2018 DOI: 10.4172/2376-032X.1000225
Abstract
Advances in imaging techniques can greatly improve the treatment outcome and enhance the success rate of surgical procedures. This review article updates the information on surgical navigation system and its application in maxillofacial surgery. The indications, treatments and outcome of surgical navigation in surgery are also discussed. Electronic searches of the MEDLINE/PubMed database were performed to identify relevant human studies published in the English-language literature from 1980 to the present. The key words derived were traumatology, orthognathic surgery, cancer, reconstruction surgery, skull base surgery and foreign body removal. These were used in combinations for the final search strategy. The search generated 53 articles and surgical navigation is considered to be a useful tool for surgical planning, execution, evaluation and research. The largest number of studies and patients are identified in the field of traumatology, oncology and management of developmental deformities and pathologies. Based on the existing literature, we propose that the surgical navigation appears to be a very promising in addition to the surgical armamentarium. Planning details of the surgery in a 3D virtual environment and execution with real-time guidance can significantly improve precision and result in better prognosis for the patient. Among factors to be considered are the financial investments and the learning curve.
Keywords: Augmented reality; Computer assisted navigation system; Cranio maxillofacial surgery; Phantoms
Introduction
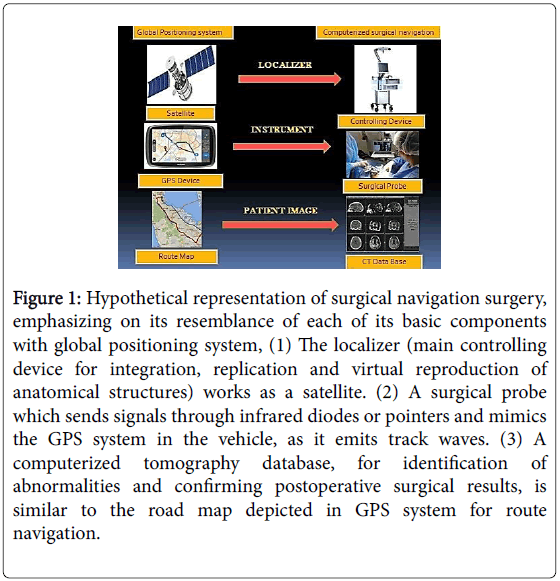
The scope of surgical management of deformities in the craniomaxillofacial region, whether they are congenital, developmental or acquired, is to reestablish facial symmetry and restore form and function [1,2]. Diagnostic imaging plays an important adjunct, to achieve these goals. Advances in imaging techniques have greatly improved the treatment outcomes and enhanced the success rate of surgical procedures. However, few problems are still faced by surgeons, notably accurate repositioning of skeletal structures in optimal three dimensional planes, restoration of ideal orbital volume, compromised visualization of deeper structures, removal of foreign bodies and assessment of variations in abnormal growth patterns. This owes, to the dependence of two dimensional imaging to treat a three dimensional problem. Thus computer-assisted navigational surgery was introduced in maxillofacial surgical practice [3-6]. It was first applied by Watanabe in 1987 [7], in neurosurgical procedures. It allows direct access to specific targeted areas through smaller incisions, thus making surgery less invasive, reliable and reducing overall operation time. Surgical navigation hypothetically resembles the global positioning system (GPS) used in automobiles and has three components: A localizer, which is similar to the satellite in space, a surgical probe, which represents the track waves emitted by the GPS in the vehicle and a computerized tomography (CT) scan data set, which is analogous to a road map (Figure 1). Apart from CT scan, the data set can also use magnetic resonance imaging and positron emission tomography [8].
Figure 1: Hypothetical representation of surgical navigation surgery, emphasizing on its resemblance of each of its basic components with global positioning system, (1) The localizer (main controlling device for integration, replication and virtual reproduction of anatomical structures) works as a satellite. (2) A surgical probe which sends signals through infrared diodes or pointers and mimics the GPS system in the vehicle, as it emits track waves. (3) A computerized tomography database, for identification of abnormalities and confirming postoperative surgical results, is similar to the road map depicted in GPS system for route navigation.
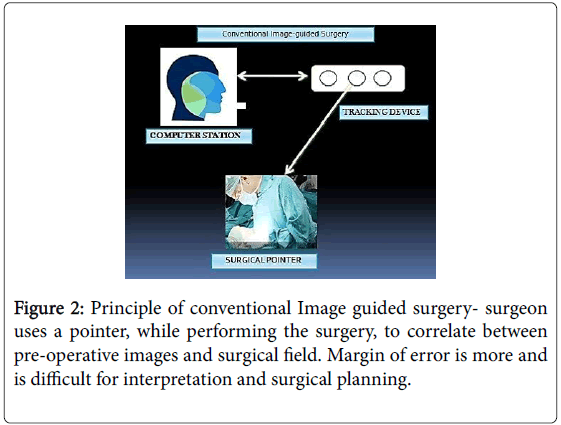
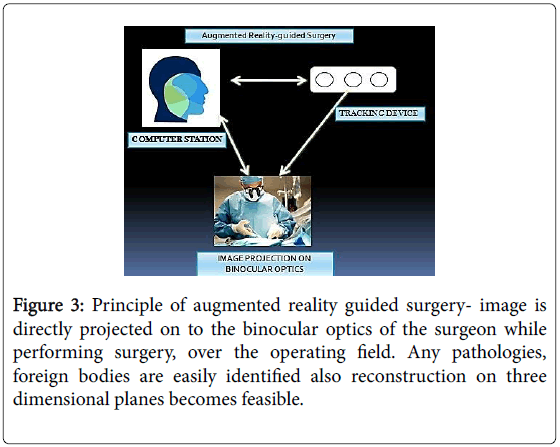
In conventional technique the surgeon uses the pointer to establish correlation with pre-operative image data and the surgical field (Figure 2), but it is difficult to orient the images, thus augmented reality system was developed, which projects the images directly on the surgical site and is based on monocular projection in the operating microscope, headup displays, projection on to purpose built semitranslucent screens placed between the operating scene and the surgeon, or by projection into the binocular optics of a tracked surgical microscope (Figure 3). There are several types of surgical navigation systems available today.
Optical Tracking System
In this system, localized points in the surgical field can be viewed in three dimensional positions, through three or two linear cameras. The points are either infrared emitting diodes or passive high reflecting spheres. This system provides high accuracy, however only drawback is that the line of sight between the cameras and tracked points should not be obstructed [9,10].
Screen-Based Systems
Columbia scientific SIM/Plant software (Columbia scientific, USA)
This software helps the surgeon, in visualization of implants being inserted surgically, through CT scan images. It also provides a 3 dimensional picture of maxillofacial regions with accurate locations of vital structures and helps in the measurement of quality of bone [11,12].
VISIT surgical navigation software (Vienna, Austria)
This software aids in simulation of dental implant positions during treatment planning phase. Intraoperatively the drill is visualized by oblique reformatting beside the drill part and the images are changed according to the tracking system. VISIT is popularly used in placement of dental and extraoral implants in maxillofacial region [13,14].
Vector vision (Brainlab, Munich, Germany)
This system uses passive marker technology, thus any surgical instrument can be immediately integrated in the operation virtually. The position of the instrument is located and controlled relatively to their positions on preoperative images. This system allows imageguided microscopy, functional mapping, automatic image fusion, which helps in guiding osteotomies and removal of foreign bodies [15,16].
Stryker leibinger navigation system (Stryker, Leibinger, Freiburg, Germany)
In this system a two-way communication takes place between the wireless instrument and navigation system. The surgeon can control patients image data through the handpiece, therefore eliminating the need of touch screen controls [17,18].
Optical tracking system microscope (OTS, Radionics, Tyco Healthcare Group, USA)
This optical tracking system, precisely matches the preoperative images, with the patient’s anatomy and enables the surgeon to track various instrument, during surgery. The location of the instruments and their trajectories are displayed on the screen in either two or three dimensional views [6,19].
Projected Image-Based Systems
Surgical microscope navigation system (SMN, Zeiss, Oberkochen, Germany)
This system is a medical version of navigational target locator, used by fighter pilots to fire missiles by aiming at a computer plotted image. It uses a computer driven navigational microscope to provide intraoperative three dimensional view, even before the incision is placed. It transfers scans of surgical area to the computer, which in turn projects the information onto the lens of the navigational microscope, positioned above the patient. It allows the surgeon to follow a planned surgical path, similar to a road map [20,21].
Surgical segment navigator (SSN, Carl Ziess)
It is based on infrared technology and the preoperative data is transferred to the surgical site through infrared transmitters tracked by an infrared camera. The system comprises of an infrared positioning device, two reference frames, an infrared pointer and an infrared camera. It can be used in repositioning of fractured segments, osteotomy cuts, positioning of artificial joints and implants. All data are displayed numerically and graphically on the monitor [22,23].
Microscope-assisted guided interventions (MAGI)
It basically works by projecting the images into the binocular optics of an calibrated and tracked surgical microscope, with an accuracy of 1 mm [24]. it works on the principle of stereo augmented reality system, developed by Kings College London [25]. The system consists of a Leica binocular operating microscope adapted by incorporating two purpose-built monochrome displays and an Optotrak localizer (Northen Digital Inc.). Changes in the position of the microscope are tracked using an array of 13 infrared emitting diodes mounted on a bracket rigidly attached to the microscope assembly. Patient’s position is established by tracking 6 such diodes fixed to a custom-built locking acrylic dental splint [24].
Electromagnetic tracking systems
This system is entirely wireless, thus does not have any line-of-sight restrictions like other systems. But metal instruments can disrupt the electromagnetic waves and hamper the accuracy of the procedure [26,27].
Heat mounted display system (ARTMA)
Through this system, the surgeon can see virtually images of anatomical structures directly on display of headset or endoscope. It is a type of augmented reality system [28,29].
Insta trak (GE medical systems)
This system helps the surgeon to mark critical zones preoperatively, which can be seen during the surgery. Through the development of the magnetic intelligence algorithm from the manufacturer, the system automatically detects and compensates for metal in the field, resulting in improved clinical accuracy and reliability [30,31].
Mechanical Tracking Systems
Viewing wand (ISG, Mississauga, Ontario, Canada)
It was the first frameless neuronavigation device used and consists of an articulated mechanical arm (FARO Technologies) with a handheld probe, used by the surgeon as pointer. The mechanical operating arm carries 6 joints and has 6 degrees of freedom working as a digitiser, and is interfaced to a computer graphics workstation [30,31].
Use of surgical navigation in oral and maxillofacial surgery
Surgical navigation has great potential in various specialties and provides precision based surgical procedures in areas of complex anatomy, as in maxillofacial region. Recent advances in this field have offered new prospects for orthognathic surgery, reconstruction of facial bones, implantology and Temporomandibular joint (TMJ) disorders.
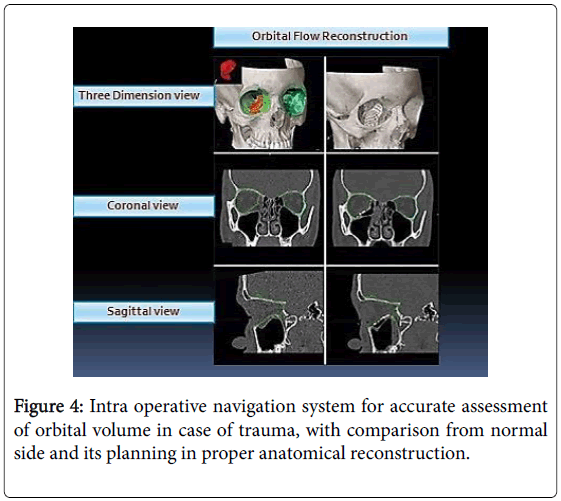
Orbital reconstruction
High velocity impacts, mostly results in shattered orbits, with increase in volume, herniation of periorbital contents into the sinus and cranial neuropathies. Despite the use of advanced biocompatible materials by experienced surgeons [32,33], it is still difficult to replace and recontour anatomical landmarks with precision and predictability [34-37]. Use of intraoperative navigation with proper preoperative planning, have ensured accurate positioning of plates in less visualized anatomic regions. Metzger et al. [38] described a semiautomatic procedure to use titanium meshes mirrored and constructed as the unaffected side, through CT scans and placed using frameless stereotaxy with three infrared cameras, controlling the pointer by integrated light emitting diodes.
Maxillofacial reconstruction
Defects causing discrepancies in mandibular continuity or palatal integrity, due to tumor resection or trauma, results in psychological distress and severe debilitating conditions for the patient. Free fibular osteocutaneous flap, has been used by surgeons throughout the world, since it was introduced by Hidalgo [39,40], to reconstruct maxillomandibular defects and has proven to be a highly successful and reliable option. Despite its wide acceptance, two school of thoughts lures upon, its method of fixation.
Tumor resection
Intraoperative navigation has been proposed as a means to delineate resection margins during extirpative tumor surgery in the craniomaxillofacial skeleton [41-43]. Several reports have highlighted the value of this technology in improving the precision in which tumors are resected, while minimizing the amount of uninvolved tissues. In addition, surgery involving the skull base, pterygomaxillary fossa, or infratemporal fossa, including temporomandibular joint (TMJ) ankylosis release [44], may be performed with an added degree of safety with respect to surrounding vital structures (Figure 4). Finally, osteotomies may be accurately positioned based on a presurgical image so that preformed implants, bone grafts, or free flaps may be inset into the defect in an effort to increase operative efficiency and accuracy.
Orthognathic surgery
Preoperative computer imaging and intraoperative navigation are useful for planning complex surgical movements of the craniofacial skeleton. Using recently designed Computer-aided design/ Computeraided manufacturing (CAD/CAM) software, osteotomies may be planned and the jaws or other anatomic structures can be virtually repositioned in any plane of space [45-48].
Discussion
The benefits of image-guided surgery have been reported in a number of studies, with improved results. In implantology the surgeon is no longer restricted to two-dimensional images therefore complications such as damage to the inferior dental nerve and perforations can be avoided. An accuracy of 1-2 mm was reported by Wanschitz et al. [49] in image-guided implantology using VISIT surgical navigation software. Template systems, designed to transfer a preoperatively defined implant position on to the surgical site, are also reported to produce accurate results. The use of a template eliminates errors in manual insertion and matches planning to prosthetic requirements. Implant operations can be simulated using Columbia Scientific SIM/Plant software. The three-dimensional implant positions can be transferred by computer to a milling machine, which mills the implant coordinate positions into the template. These positions will dictate the location, angle, and depth of insertion of the implant.
Image guidance has also been used to improve the accuracy of osteotomies. SSN (Zeiss) was the first highly precise system to transfer laboratory-planned data concerning the repositioning osteotomy to the surgical site. It has been applied for repositioning osteotomies of the orbital walls, where it displays hidden levels of bone, which may not be visible with a bicoronal approach, and helps to navigate the complete structure. The Viewing Wand has been reported to achieve 2 mm accuracy in 40 operations, including osteotomies and resection of tumours of the mid-facial area [50]. Satisfactory results have been recorded with the ARTMA head-mounted display system in secondary reconstruction of post-traumatic deformities of the zygoma. This system can also be used to superimpose virtual osteotomy lines on the maxilla to guide the oscillating saw in orthognathic operations. Application of image guidance to surgical oncology is currently most successful in tumours associated with the bony structures of the maxillofacial region because of the lack of deformation of soft tissues. Wagner et al. used their guidance system (ARTMA) to navigate instruments to an osteosarcoma in the deep infraorbital region. Insta trak system has also been used to guide orbital dissection for removal of tumours from the orbit.
Future Prospective
Computer-assisted navigation system has various areas for further evaluation and improvement. Reducing high costs of the system and time required for getting accustomed with it, is first and foremost. The markers used for detecting geometrical center are prone to give false recordings due to sterilization and reuse, recognition of such flaws are required and amended. Reconfiguration, rebooting and aborting navigation are few methods to solve, if errors are encountered, however, the correlation between these problems and model type has not been yet investigated.
Conclusion
This review provides the reader with updated information and knowledge regarding the recent literature on surgical navigation. Navigation-assisted technology in craniomaxillofacial surgery increases reliability by facilitating correct safety margins and protecting vital structures. In addition, it increases the precision of radiotherapy planning and it facilitates the reconstruction process. However the costs for the navigation systems are very high, and the time for preparation for the surgery is longer in comparison with conventional technique. However, the navigation procedure gives more security, particularly in complex cases and also may result in a better clinical outcome for the patient. Further development of software programs may reduce the preoperative planning time and time spent during the operation.
Conflict of Interest
We have no conflict of interest.
Ethics Statement
Ethics approval not required.
References
- Gruss JS, Bubak PJ, Egbert MA (1992) Craniofacial fractures. An algorithm to optimize results. Clin Plast Surg 19: 195–206.
- Manson PN, Hoopes JE, Su CT (1980) Structural pillars of the facial skeleton: An approach to the management of Le Fort fractures. Plast Reconstr Surg 66: 54–61.
- Schmelzeisen R, Gellrich NC, Schramm A, Schon R, Otten JE (2002) Navigation-guided resection of temporomandibular joint ankylosis promotes safety in skull base surgery. J Oral Maxillofac Surg 60: 1275.
- Gellrich NC, Schramm A, Hammer B, Rojas S, Cufi D, et al. (2002) Computer-assisted secondary reconstruction of unilateral posttraumatic orbital deformity. Plast Reconstr Surg 110: 1417.
- Bell RB (2011) Computer planning and intraoperative navigation in orthognathic surgery. J Oral Maxillofac Surg 69: 592.
- Nijmeh AD, Goodger NM, Hawkes D, Edwards PJ, Mcgurk M (2005) Image-guided navigation in oral and maxillofacial surgery. Br J Oral Maxillofac Surg 43: 294-302.
- Watanabe E, Watanabe T, Manaka S, Mayanagi Y, Takakura K (1987) Three-dimensional digitizer (Neuronavigator): New equipment for computed tomography-guided stereotaxic surgery. Surg Neurol 27: 543–547.
- Bell RB (2010) Computer planning and intraoperative navigation in cranio-maxillofacial surgery. Oral Maxillofacial Surg Clin N Am 22: 135-156.
- Koivukangas T, Katisko J, Koivukangas JP (2013) Technical accuracy of optical and the electromagnetic tracking systems. Springer Plus 2: 1-7.
- Ruppin J, Popovic A, Strauss M, Spuntrup E, Steiner A, et al. (2008) Evaluation of the accuracy of three different computer-aided surgery systems in dental implantology: Optical tracking vs. stereolithographic splint systems. Clin Oral Implants Res 19: 709-716.
- Hagiwara Y, Koizumi M, Igarashi T (1999) Application of CT imaging for dental implant simulation. J Oral Sci 41: 157-161.
- Stockman CD (1996) Using CT and SIM/ Plant to plan implant therapy. Alpha Omega 89: 35-38.
- Watzinger F (2002) Evaluation of the intraoperative position of endosseous oral implants in the edentulous mandible. Clin Oral Implants Res 13: 59-64.
- Wagner A, Wanschitz F, Birkfellner W, Zauza K, Klug C, et al. (2003) Computer-aided placement of endosseous oral implants in patients after ablative tumor surgery: Assessment of accuracy. Clin Oral Implants Res 14: 340-348.
- Gumprecht HK, Widenka DC, Lumenta CB (1999) BrainLab VectorVision Neuronavigation system: Technology and clinical experiences in 131 cases. Neurosurgery 44: 97-104.
- Siessegger M, Schneider BT, Mischkowski RA, Lazar F, Krug B, et al. (2001) Use of an image-guided navigation system in dental implant surgery in anatomically complex operation sites. J Craniomaxillofac Surg 29: 276-281.
- Gui H, Yang H, Shen SGF, Bing H, Zhang S, et al. (2013) Image-guided surgical navigationfor removal of foreign bodies in the deep maxillofacial region. J Oral Maxillofac Surg 71: 1563-1571.
- Kim YH, Jung DW, Kim TG, Lee JH, Kim IK (2013) Correction of orbital wall fracture close to optic canal using computer-assisted navigation surgery. J Craniofac Surg 24: 1118-1122.
- Kato A, Yoshimine T, Hayakawa T, Tomita Y, Ikeda T, et al. (1991) A frameless, armless navigational system for computer-assisted neurosurgery. J Neurosurg 74: 845-849.
- Gaggl A, Schultes G, Karcher H (2001) Navigational precision of drilling tools preventing damage to the mandibular canal. J Craniomaxillofac Surg 29: 271-275.
- Marmulla R, Hilbert M, Niederdellmann H (1998) Intraoperative precision of mechanical, electromagnetic, infrared and laser guided navigation systems in computer-assisted surgery. Mouth jaw and facial surgery 2: 145-148.
- Marmulla R, Niederdellmann H (1999) Computer-assisted bone system navigation. J Craniomaxillofac Surg 26: 347-359.
- Marmulla R, Niederdellmann H (1999) Surgical planning of computer-assisted repositioning osteotomies. Plast Reconstr Surg 104: 938-944.
- King AP, Edwards PJ, Maurer CR Jr, de Cunha DA, Hawkes DJ, et al. (1999) A system for microscope-assisted guided interventions. Stereotact Funct Neurosurg 72: 107-111.
- Roessler K, Ungersboeck K, Czech T, Aichholzer M, Dietrich W, et al. (1997) Contour-guided brain tumor surgery using a stereotactic navigating microscope. Stereotact Funct Neurosurg 68: 33-38.
- Ewers R (2005) Basic research and 12 years of clinical experience in computer-assisted navigation technology: A review. Int J Oral Maxillofac Surg 34: 1-8.
- Fried MP, Kleefield J, Gopal H, Reardon E, Ho BT, et al. (1997) Image-guided endoscopic surgery: Results of accuracy and performance in a multicenter clinical study using an electromagnetic tracking system. Laryngoscope 107: 594-601.
- Wagner A, Ploder O, Enislidis G, Truppe M, Ewers R (1995) Virtual image-guided navigation in tumor surgery- technical innovation. J Craniomaxillofac Surg 23: 271-273.
- Wagner A, Millesi W, Watzinger F (1999) Clinical experience with interactive teleconsultation and teleassistance in craniomaxillofacial surgical procedures. J Oral Maxillofac Surg 57: 1413-1418.
- Casap N, Wexler A, Persky N, Schneider A, Lustmann J (2004) Navigation surgery for dental implants: Assessment of accuracy of the image guided implantology system. J Oral Maxillofac Surg 62: 116-119.
- Eggers G, Muhling J, Marmulla R (2006) Image-to-patient registration techniques in head surgery. Int J Oral Maxillofac Surg 35: 1081-1095.
- Dyer PV, Patel N, Pell GM, Cummins B, Sandeman DR (1995) The ISG viewing wand: an application to atlanto-axial cervical surgery using lefort I maxillary osteotomy. Br J Oral Maxillofac Surg 33: 370-374.
- Puechot B, Tanguy A, Eude M (1995) Virtual reality as an operative tool during scoliosis surgery. CVR Med 549-54.
- Blackwell M, O’Toole R, Morgan F, Gregor L (1995) Performance and accuracy experiments with 3D and 2D image overlay systems. In: DiGioia AM, Taylor R, Kikinis R, editors. Medical robotics and computer assisted surgery. Baltimore, pp: 312-317.
- Edwards PJ, King AP, Maurer CR Jr, de Cunha DA, Hawkes DJ, et al. (2000) Design and evaluation of a system for microscope-assisted guided interventions (MAGI). IEEE Trans Med Imaging 19: 1082-1093.
- Hammer B, Kunz C, Schramm A, deRoche R, Prein J (1999) Repair of complex orbital fractures: Technical problems, state of the art solutions and future perspectives. Ann Acad Med Singap 28: 687–691.
- Schmelzeisen R, Gellrich NC, Schoen R (2004) Navigation-aided reconstruction of medial orbital wall and floor contour in cranio-maxillofacial reconstruction. Int J Care Injured 35: 955-962.
- Metzger MC, Schon R, Schulze D, Carvalho C, Gutwald R, et al. (2006) Individual preformed titanium meshes for orbital fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102: 442-447.
- Klug C, Schicho K, Ploder O, Yerit K, Watzinger F, et al. (2006) Point to point computer assisted navigation for precise transfer of planned zygoma osteotomies from the stereolithographic model into reality. J Oral Maxillofac Surg 64: 550-559.
- Hidalgo DA (1989) Fibula free flap: A new method of mandible reconstruction. Plast Reconstr Surg 84: 71-79.
- Wei FC, Santamaria E, Chang YM, Chen HC (1997) Mandibular reconstruction with fibular osteoseptocutaneous free flap and simultaneous placement of osseointegrated dental implants. J Craniofac Surg 8: 512.
- Schramm A, Suarez-Cunqueiro MM, Barth EL, Essig H, Bormann KH, et al. (2008) Computer assisted navigation in craniomaxillofacial tumors. J Craniofac Surg 19: 1067-1074.
- Schramm A, Gellrich NC, Gutwald R, Schipper J, Bloss H, et al. (2000) Indications for computer assisted treatment of cranio-maxillofacial tumors. Comput Aided Surg 5: 343-352.
- To EW, Yuen EH, Tsang WM, Lai EC, Wong GK, et al. (2002) The use of stereotactic navigation guidance in minimally invasive transnasal nasopharyngectomy: A comparison to the conventional open transfacial approach. Br J Radiol 75: 345-350.
- Metzger MC, Hohlweg-Majert B, Schwarz U, Teschner M, Hammer B, et al. (2008) Manufacturing splints of orthognathic surgery using a three dimensional printer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105: 7.
- Swennen GR, Mommaerts MY, Abeloos J, De Clercq C, Lamoral P, et al. (2007) The use of a wax bite wafer and a double computed tomography scan procedure to obtain a three dimensional model. J Craniofac Surg 18: 533-5339.
- Olszewski R, Villamil MB, Trevisan DG, Nedel LP, Freitas CM, et al. (2008) Towards an integrated system for planning and assisting maxillofacial orthognathic surgery. Comput Methods Programs Biomed 91: 13-21.
- Wanschitz F, Birkfellner W, Watzinger F, Schopper C, Patruta S, et al. (2002) Evaluation of accuracy of computer-aided intraoperative positioning of endosseous oral implants in the edentulous mandible. Clin Oral Implants Res 13: 59-64.
- Hassfeld S, Muhling J, Zoller J (1995) Intraoperative navigation in oral and maxillofacial surgery. Int J Oral Maxillofac Surg 24: 111-9.
- Wagner A, Ploder O, Enislidis G, Truppe M, Ewers R (1996) Image guided surgery. Int J Oral Maxillofac Surg 25: 147-151.
Citation: Kumar V, Chaudhry K, Gour S, Aeran H, Agarwal A (2018) Advent of Surgical Navigation in Oral and Maxillofacial Surgery and Application of Different Navigational Systems in Various Surgical Procedures: A Review. J Interdiscipl Med Dent Sci 6: 225. DOI: 10.4172/2376-032X.1000225
Copyright: ©2018 Kumar V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6440
- [From(publication date): 0-2018 - Nov 13, 2025]
- Breakdown by view type
- HTML page views: 5395
- PDF downloads: 1045