Adolescent Hypertension Induced by Obesity and the Efficacy of Comprehensive Intervention
Received: 01-Dec-2021 / Manuscript No. CMB-21-42568 / Editor assigned: 03-Dec-2021 / PreQC No. CMB-21-42568 (PQ) / Reviewed: 30-Dec-2021 / QC No. CMB-21-42568 / Revised: 04-Jan-2022 / Manuscript No. CMB-21-42568 (R) / Accepted Date: 04-Jan-2022 / Published Date: 11-Jan-2022 DOI: 10.4172/1165-158X.1000220
Abstract
Background and Objective: With the development of economy, people's quality of life has been improved, obesity caused by over-nutrition has increased among teenagers, and the age of patients with obesity induced hypertension has been younger and younger.
Methods: In order to effectively prevent and treat adolescent hypertension, this study collected the data of age, height, weight, demographic characteristic, waist circumference, hip circumference, knowledge of hypertension and blood pressure of 1000 students at Grade 7 ~ 9 in XX middle school through questionnaire and physical examination, and the relationships between the above factors were analyzed. Students with obesity induced hypertension were given comprehensive intervention. Blood pressure, blood lipid, blood glucose and body mass index were detected before and after treatment.
Results: Obesity index of students with hypertension were significantly higher than those of normal students. Age, waist circumference and body mass index significantly affected the risk of hypertension. After comprehensive intervention, the blood pressure, blood lipid, body mass index and glycosylated albumin of students with hypertension decreased, glucagon increased, and no significant changes were found in other blood glucose indexes.
Conclusion: Obesity increases the risk of hypertension, and comprehensive interventions can effectively prevent and treat adolescent hypertension.
Keywords
Hypertension; Comprehensive intervention; Adolescents; Obesity
Introduction
The prevalence of obesity among adolescents in both developing and developed countries has increased at the same rate over the past decade. In China, with the rapid development of economy, the prevalence of general obesity and abdominal obesity among adolescents increased from 6.1% and 4.9% to 13.1% and 11.7% respectively from 1993 to 2009. The prevalence of overweight and obesity among 7-18-yearold students from 1985 to 2010 increased from 0.2% to 8.1%, and the prevalence of overweight and obesity increased rapidly [1]. Adolescents obesity can not only bring about inconvenience to life, but also greatly increase the risk of hypertension; in addition, obesity can also induce other cardiovascular diseases [2]. Studies have shown that obesity is associated with morbidity and long term mortality, and overweight or obese children are more likely to be associated with a number of other risk factors for vascular disease, including dyslipidemia, essential hypertension and metabolic syndrome, and Childhood Weight Status can be an important predictor of adult obesity, hypertension and even mortality. Adolescents suffering from hypertension will not recover as time goes on, but will increase the incidence of metabolic syndrome [3]. Hypertension will seriously affect the structure and function of organs, which is likely to cause irreversible permanent damage. For hypertension which has complex pathogenesis and is affected by many factors, there is no favorable specific medicine but developing good living habits under the assistance of comprehensive intervention means and applying reasonable drug means are very likely helpful for hypertension [4]. Kar S and Khandelwal B [5], Cheung, et al. [6] and Nam, et al. [7] estimated the prevalence and sociodemographic correlation of obesity and hypertension among school-age children (11-19 years old) in Gangtok, Sikkim, India and found that the prevalence of obesity, overweight and hypertension were 2.04%, 14.5% and 5.62% respectively and average fast food intake, screen time and limited outdoor activities were significantly associated with obesity. Obesity as a predictive factor for hypertension has an improved accuracy among white Hispanic white adolescents and has a decreased accuracy among African American adolescents. In this study, we comprehensively analyzed the relationship between age, height, weight, waist circumference, demographic characteristic, hip circumference, knowledge of hypertension and blood pressure in 1,000 students in grade 7-9 of XX Middle School through questionnaire survey and physical examination. Then, the obese and hypertensive patients were selected for comprehensive intervention treatment. The same examination of blood pressure, blood lipid and BMI were performed before and after treatment.
As we all known that obesity could lead to hypertension, hypertension will severely affect the structure and operation functions of important organs. The damage caused by hypertension to target organs may last for a lifetime, or the damage to target organs may be aggravated because of hypertension in adulthood. There are no comprehensive and convincing studies about the pathogenesis of hypertension in the world [8]. According to the relevant survey report, the prevalence of hypertension caused by obesity among adolescents is increasing, and it is very likely to develop into adult hypertension.
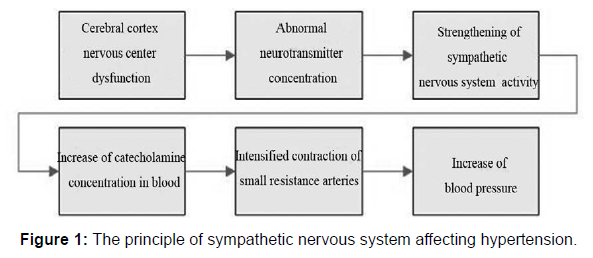
The pathogenesis of hypertension is complex. Abnormal sympathetic nervous system, vascular function and fat may be the causes of hypertension, but in most cases, there are many reasons working together. The single cause of hypertension is rare. The effect of sympathetic nervous system on hypertension is shown in Figure 1.
Firstly, abnormal changes of central nervous system in the cerebral cortex produces wrong signals, which leads to abnormal secretion of tissues which secretes abnormal neurotransmitter, including adrenaline and dopamine leading to the enhance of the activity of sympathetic nervous system, which in turn increases the concentration of catecholamine in blood and enhance the contraction of resistance arterioles.
The effect of vascular dysfunction on hypertension was related to renin-angiotensin-aldosterone system (RAAS) [9]. When RAAS was activated for some reasons, the activity of renin and aldosterone would increase dramatically, thus promoting the production of angiotensin in the relevant tissues. Angiotensin could promote the contraction of small arteries and ultimately increase blood pressure.
The effect of abnormal fat on hypertension was related to adipokines, such as leptin and adiponectin [10]. Leptin was a polypeptide that could activate the sympathetic nervous system when entering blood to increase blood pressure. However, the effect of leptin on blood pressure was related to population characteristics, such as race or body type. Adiponectin was a glycoprotein, which played an important role in lipid and blood glucose metabolism. Moreover, it could improve NO level by eliminating endothelial cell dysfunction, which might be used for inhibiting the activity of sympathetic nervous system to achieve antihypertensive effect.
Methods
Analysis of object
The 1000 students aged 7 to 9 in Nantong middle school were investigated from September 2019 to March 2020 in First People’s Hospital of Nantong. There were 525 female and 475 male, with an average age of (15.7±0.12) years old. 1000 students were randomly selected for empirical analysis. No family history was reported, and no serious illness occurred in the past year. Assess the prevalence of obesity and associated metabolic abnormalities. This group completed anthropometric, blood pressure and clinical examinations, fasting venous blood testing, and standard questionnaires to form the baseline population for the follow-up cohort for this study. Participate in a unified medical examination after the investigators and their parents or guardians have signed informed consent.
Obesity and hypertension state
Height and weight measurement: The subjects took off their shoes and coats and stood on a height and weight scale in a standard upright position. The body was naturally straight during the test. The tester read the height and weight strictly according to the standards.
The height was in centimeters (cm) and the weight was in kilograms (kg). Because different people had different heights, it was inaccurate to judge obesity by weight alone. Therefore, it was necessary to connect height with weight, i.e. body mass index (BMI), to measure whether a person was obese. The metric formula was as follows [11]:
BMI = (Weight in Kilograms / (Height in Meters x Height in Meters))
According to the standards for growth and development of children released by WTO, BMI ≥ 25 kg/m2 was evaluated as overweight and BMI ≥30 kg/m2 was evaluated as obese.
Waist circumference and hip circumference measurement: The waist and hip circumferences of the subjects were measured using an elastic tape. When measuring waist circumference, the elastic tap was encircled one round above the navel. On the premise of not cutting into the skin, the tape was as close to the skin as possible, and the reading was accurate to one digit before the decimal point. When measuring hip circumference, the tape was encircled one round around the widest part of the hip. The subjects were in an upright position, and the reading was accurate to one digit after the decimal point [12].
Blood pressure test: The subjects sat quietly. The arterial blood pressure of the right upper arm was measured by the calibrated mercury sphygmomanometer. The right upper arm was kept at the same level as the heart, and the upper arm was tightly warped with the cuff. The interval of three measurements was 1 minute. The error between readings was less than 4 mm Hg, and the average was taken as the final result. Hypertension was affected by sex, age and height. According to the criteria published by the American Hypertension Education Project Youth Working Group, hypertension was determined when the mean systolic blood pressure (SBP) or (and) mean diastolic blood pressure (DBP) was greater than or equal to P95.
Body fat percentage (Fpeixenteige, FFMP)
TBF-300A body fat / weight measuring instrument (Japanese TANITA company) was used for measurement. Children under investigation took off jackets, shoe boxes, hats, etc., wore light underwear, and stood barefoot on induction metal plates while keeping their readings.
Hypertension and comprehensive intervention
Laboratory detection: The obese and hypertensive students were selected and forbidden to eat for 12 h overnight. 4 mL of fasting venous blood was collected from each student on the next morning. The plasma was separated by high-speed centrifugation, and then triglycerides, total cholesterol, blood glucose, glycated hemoglobin, glycated albumin, insulin and glucagon in plasma were detected by a fully automatic biochemical analyzer. The operation was conducted once before and after the comprehensive intervention.
Comprehensive intervention
Comprehensive interventions were provided for obese and hypertensive students. The intervention methods included, but were not limited to, text message guidance, home visit guidance and relevant knowledge lectures [13]. For example, public brochures were issued to explain the causes and consequences of hypertension and how to prevent it. Family visit was conducted every half month to monitor students’ compliance with doctor's orders; if they did not comply, then timely intervention was given. The content of intervention was as follows: Psychological counseling was provided to the patients to stabilize their emotions and actively face the intervention treatment.
Under the premise of ensuring a balanced diet, try to limit sodium intake and prohibit excessive eating. Moreover, the patients were asked to exercise reasonably according to their physical conditions. The guardians help the patients to correct bad habits and maintain a reasonable rest. Reasonable weight control plans were formulated according to the actual situation of different patients.
Statistical Analysis
Relevant data were analyzed using SPSS 20.0 software. The count results were expressed as. The student t-test was performed to analyze the difference between two groups and one-way ANOVA was applied to compare the difference between multiple groups. Each assay was repeated at least three times and the average was statistically analyzed. Multivriate regression analysis was utilized to indicate the relationship between obesity and hypertension related factors.
Under the premise of ensuring a balanced diet, try to limit sodium intake and prohibit excessive eating. Moreover, the patients were asked to exercise reasonably according to their physical conditions. The guardians help the patients to correct bad habits and maintain a reasonable rest. Reasonable weight control plans were formulated according to the actual situation of different patients.
Result
Analysis of obesity and hypertension state
As shown in Table 1, the average weight of the hypertension group and normal group was (63.49 ± 13.22) kg and (2.59 ± 10.21) kg respectively, with (P = 0.001), which show a statistically significant difference. The waist circumference of the hypertension group and normal group was (75.44 ± 10.92) cm and (68.73 ± 8.15) cm respectively, with (P < 0.05), which show a statistically significant difference. The hip circumference of the hypertension group and normal group was (92.10 ± 7.98) cm and (85.95 ± 7.91) cm respectively, with (P < 0.05), which show a statistically significant difference. The BMI of the hypertension group and normal group was (22.12 ± 4.02) kg/m2 and (19.58 ± 3.34) kg/m2 respectively, with (P < 0.05), which show a statistically significant difference. The waist-hip ratio of the hypertension group and normal group was (0.83 ± 0.08) and (0.81 ± 0.07) respectively, with (P < 0.05), which show a statistically significant difference. The waist-to-height ratio of the hypertension group and normal group was (0.46 ± 0.07) and (0.44 ± 0.06), with (P < 0.05), which show a statistically significant difference. It was found that the obesity indicators of the hypertension group were larger than those of the normal group, and the differences were statistically significant.
| Item | Hypertension group | Normal group | P value |
|---|---|---|---|
| Weight/kg | 63.49 ± 13.22 | 52.59 ± 10.21 | 0.000 |
| Waist circumference/cm | 75.44 ± 10.92 | 68.73 ± 8.15 | 0.001 |
| Hip circumference/cm | 92.10 ± 7.98 | 85.95 ± 7.91 | 0.000 |
| BMI (kg/m2) | 22.12 ± 4.02 | 19.58 ± 3.34 | 0.002 |
| Waist-hip ratio | 0.83 ± 0.08 | 0.81 ± 0.07 | 0.003 |
| Waist-height ratio | 0.46 ± 0.07 | 0.44 ± 0.06 | 0.000 |
Table 1: The relationship of obesity and hypertension of adolescents.
As shown in Table 2, multivariate regression analysis showed that only age, hip circumference and BMI were significantly correlated with hypertension. The regression coefficients of age, hip circumference and BMI were 0.182, 0.062 and 0.096 respectively, all of which were positively correlated with hypertension. It indicated that the greater the age, hip circumference and BMI, the more likely it was to suffer from hypertension.
| Variable | Regression coefficient | Standard error | P Value |
|---|---|---|---|
| Age | 0.182 | 0.065 | 0.006 |
| Demographic characteristic | 0.123 | 0.101 | 0.123 |
| Weight | 0.211 | 0.094 | 0.233 |
| Waist circumference | 0.066 | 0.087 | 0.450 |
| Hip circumference | 0.062 | 0.015 | 0.000 |
| BMI | 0.096 | 0.028 | 0.000 |
| Relevant knowledge of hypertension | 0.111 | 0.101 | 0.125 |
Table 2: The regression analysis of hypertension related factors.
The effect of comprehensive intervention treatment
As shown in Table 3, the average systolic pressure, average diastolic pressure, BMI, body fat, trunk fat, abdominal fat, upper limbs fat and lower limbs fat of the patients with hypertension before and after comprehensive treatment were different in different parts of the patients.
| Test index | Before comprehensive intervention | After comprehensive intervention | P Value |
|---|---|---|---|
| BMI (kg/m2) | 28.6 ± 5.5 | 26.4 ± 5.2 | 0.000 |
| Average systolic pressure/mmHg | 135.9 ± 16.7 | 112.6 ± 13.3 | 0.001 |
| Average diastolic pressure/mmHg | 87.4 ± 7.6 | 71.3 ± 9.2 | 0.002 |
| Body fat/% | 36.94 ± 4.12 | 32.55 ± 4.42 | 0.004 |
| Trunk fat/kg | 13.74 ± 3.33 | 10.84 ± 3.10 | 0.003 |
| Abdominal fat/kg | 5.78 ± 1.12 | 4.57 ± 1.19 | 0.001 |
| Upper limbs fat/kg | 2.41 ± 0.77 | 2.01 ± 0.54 | 0.002 |
| Lower limbs fat/kg | 8.77 ± 2.41 | 7.24 ± 1.84 | 0.001 |
Table 3: Changes of blood pressure and body composition before and after comprehensive intervention.
As shown in Table 4, triglycerides, total cholesterol and glycated albumin in the obese adolescents with hypertension were significantly decreased after six months of comprehensive intervention compared with those before treatment (all P < 0.01); glucagon was significantly increased (P < 0.05); however, there were significant changes in blood glucose, glycated hemoglobin and insulin resistance index after treatment (P < 0.05).
| Test index | Before comprehensive intervention | After comprehensive intervention | P Value |
|---|---|---|---|
| Triglyceride (mmol/L) | 1.55 ± 0.55 | 1.33 ± 0.64 | 0.001 |
| Total cholesterol (mmol/L) | 5.51 ± 0.68 | 5.12 ± 0.75 | 0.002 |
| Blood glucose (mmol/L) | 3.96 ± 0.34 | 4.24 ± 0.55 | 0.123 |
| Glycated hemoglobin (%) | 4.78 ± 0.04 | 4.80 ± 0.05 | 0.141 |
| Insulin (uIU/mL) | 13.35 ± 1.28 | 13.54 ± 1.05 | 0.160 |
| Glycated albumin (%) | 15.71 ± 1.18 | 15.01 ± 1.27 | 0.009 |
| Glucagon (pg/mL) | 72.91 ± 12.45 | 81.88 ± 12.85 | 0.011 |
| Insulin resistance index | 2.45 ± 0.35 | 2.52 ± 0.49 | 0.125 |
Table 4: Changes of blood lipid and blood glucose metabolism of adolescents before and after comprehensive intervention.
Discussion
Many studies have shown that the risk of hypertension in adolescents is proportional to the degree of obesity, and obesity can also increase the incidence of hypertension in adults [12, 13]. The data of the subjects in this study showed that all obesity indicators in the hypertension group were higher than those in the normal group, indicating that the increase of fat and abnormal distribution could increase the risk of hypertension. The abnormal increase and distribution of adipose tissues in the body improved the demand for blood flow, and the arterial blood pressure increased to achieve such a high-circulation system [14]. On the other hand, the content of adipocyte factor such as leptin in obese people increased the excitability of sympathetic nervous system, resulting in increased blood pressure. Multivariate analysis of factors influencing hypertension showed that older people were more likely to have hypertension regardless of gender. The reason might be the increased study stress and physiological changes brought by the increase of age. Adolescents who are at the stage of rapid growth have increased blood flow, and the blood pressure is inevitably increased.
The pathogenesis of hypertension is complex, and it is influenced by many factors. Previous evidence has shown that, in addition to obesity and hyperlipidemia, daily habits, such as sleep quality, diet and lack of exercise are also factors affecting the incidence of hypertension [15]. In this study, we verified the effectiveness of comprehensive intervention measures by comparing blood pressure, blood lipid and blood glucose before and after comprehensive intervention. The results showed that the body mass index and glycosylated albumin of students with hypertension decreased, and glucagon increased after comprehensive intervention. Triglycerides and total cholesterol are blood lipids. Blood lipids are secreted by adipocytes in the body and enter the plasma. These lipids can activate the sympathetic nervous system and promote the production of catecholamines [16]. Elevated plasma concentration can strengthen the contraction of arterioles and increase blood pressure. In the present study, we found that the two kinds of blood lipids significantly decreased and the blood pressure decreased after comprehensive intervention, suggesting that there was no need to inhibit compassion. Glycated albumin was also significantly decreased. Glucagon has been reported to promote the decomposition of glycogen and raise blood glucose level. After lots of exercise, the concentration of glucagon would rise. In this study, both blood glucose and glucagon levels before and after intervention was at the normal levels, while glucagon increased after intervention. It might be because it had not decreased to the level before intervention during detection. The difference was normal in body regulation; therefore it had no significant significance in this study.
Conclusion
This study showed that obesity indicators in the hypertension group were higher than those in the normal group, and the difference was statistically significant. Age, waist circumference and BMI were the significant positive factors affecting the risk of hypertension. After comprehensive intervention, blood pressure, BMI and body fat were significantly reduced in patients with hypertension. After comprehensive intervention, glycated albumin in the blood lipid and glucose of the patients with hypertension was significantly decreased, and glucagon was significantly increased.
Limitations of Study
The limitations of this study include small sample size, short duration, and single-center design.
Acknowledgment
This work is support by the First People’s Hospital of Nantong.
Conflicts of Interest
None to declare.
Grant Support & Financial Disclosure
This work is support by the First People’s Hospital of Nantong.
Ethical Approval
This study was approved by the First People’s Hospital of Nantong (Approval number: 2019032)
Authors' contributions
JZ, FH, and MX conceived and designed the analysis; JZ, FH, and FZ collected the data; JZ and FH performed data analysis; JZ, FH, and MX wrote the paper.
References
- Mayer J (2016) Hypertension and Obesity. Postgrad Med 46(5): 253-254.
- Seravalle G, Grassi G (2017) Obesity and hypertension. Pharmacol Res 122: 1-7.
- Kotsis V, Antza C, Doundoulakis G, Stabouli S, Sbraccia P, et al. (2017) Obesity, Hypertension, and Dyslipidemia. Obesity pp: 1-15.
- Yu CH (2015) Origins of Adolescent Obesity and Hypertension. Pediatr Neonatol 56(5): 285-286.
- Kar S, Khandelwal B (2015) Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J Nat Sc Biol Med 6(2): 356-359.
- Cheung EL, Bell CS, Samuel JP, Poffenbarger T, Redwine KM, et al. (2017) Race and Obesity in Adolescent Hypertension. Pediatrics 139: e20161433.
- Nam EW, Sharma B, Kim HY, Paja DJ, Yoon YM, et al. (2015) Obesity and Hypertension among School-going Adolescents in Peru. J Life Med 5: 60-67.
- Tevie J, Shaya FT (2015) Association between mental health and comorbid obesity and hypertension among children and adolescents in the US. Eur Child Adolesc Psychiatry 24: 497-502.
- Subasinghe A, Wark J, Gorelik A, Garland S (2016) The Association Between Inflammation, Obesity and Prehypertension in 16-25 Year Old Australian Females. J Hypertens 34: e243.
- Ding WQ, Yan YK, Zhang MX, Cheng H, Zhao XY, et al. (2015) Hypertension outcomes in metabolically unhealthy normal-weight and metabolically healthy obese children and adolescents. J Hum Hypertens 29(9): 548-554.
- Hothan KA, Alasmari BA, Alkhelaiwi OK, Althagafi KM, Alkhaldi AA, et al. (2016) Prevalence of hypertension, obesity, hematuria and proteinuria amongst healthy adolescents living in Western Saudi Arabia. Saudi Med J 37(10): 1120-1126.
- Babinska K, Kovacs L, Janko V, Dallos T, Feber J (2012) Association between obesity and the severity of ambulatory hypertension in children and adolescents. J Am Soc Hypertens 6(5): 356-63.
- Ren Q, Su C, Wang H, Wang Z, Du W, Zhang B (2016) Prospective Study of Optimal Obesity Index Cut-Off Values for Predicting Incidence of Hypertension in 18–65-Year-Old Chinese Adults. Plos One 11(3): e0148140.
- Bertorello AM, Pires N, Igreja B, Pinho MJ, Vorkapic E, et al. (2015) Increased Arterial Blood Pressure and Vascular Remodeling in Mice Lacking Salt-Inducible Kinase 1 (SIK1). Circ Res 116(4): 642-652.
- Colín-Ramírez E, Rivera-Mancía S, Infante-Vázquez O, Cartas-Rosado R, Vargas-Barrón J, et al. (2017) Protocol for a prospective longitudinal study of risk factors for hypertension incidence in a Mexico City population: the Tlalpan 2020 cohort. BMJ Open 7: e016773.
- Bisogni V, Pengo MF, Maiolino G, Rossi GP (2016) The sympathetic nervous system and catecholamines metabolism in obstructive sleep apnoea. J Thorac Dis 8(2): 243-254.
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Indexed at Google Scholar Crossref
Citation: Zhao J, Hong F, Lu S, Zhou F, Xu M (2022) Adolescent Hypertension Induced By Obesity and the Efficacy of Comprehensive Intervention. Cell Mol Biol, 68: 220. DOI: 10.4172/1165-158X.1000220
Copyright: © 2021 Zhao J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2612
- [From(publication date): 0-2022 - Apr 26, 2025]
- Breakdown by view type
- HTML page views: 2092
- PDF downloads: 520