Case Report Open Access
Adjunct Therapy with Ketogenic Diet to Infant Bacterial Meningitis
Jiaying Feng, Jianxiang Liao*, Lili Pan, Dezhi Cao, Tieshua Huang, Jing Duan, Sufang Lin and Aizhen Yu
Shenzhen Children’s Hospital, China
- *Corresponding Author:
- Jianxiang Liao
Shenzhen Children’s Hospital, China
Tel: 5145016426
E-mail: liaojianxiang@vip.sina.com
Received date: June 27, 2016; Accepted date: June 29, 2016; Published date: June 30, 2016
Citation: Feng J, Liao J, Pan L, Cao D, Huang T, et al. (2016) Adjunct Therapy with Ketogenic Diet to Infant Bacterial Meningitis. J Preg Child Health 3:267. doi:10.4172/2376-127X.1000267
Copyright: © 2016 Feng J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Background: Bacterial meningitis is still a common disease in China, and has long hospital stay of about one month and high incidence of fatality and sequelae. We assumed that ketogenic diet (KD) could increase the low glucose in the cerebral spinal fluid, provide energy to brain, shorten the hospital stay and decrease the incidence of its fatality and sequelae, because of its action of anti-microorganisms, inflammation, antiseizure and neuroprotection. Method: Reviewing the patient’s charts. This is a retrospective case study of two consecutive early infant cases with bacterial meningitis. Results: After consulted to an infant who was with meningococcal bacterial meningitis and had left severe occipital encephalomalacia, came the infant girl with bacterial meningitis, because of three days fever and a 30 minutes seizure. Blood culture got pneumonia streptococcus and cerebral spinal fluid (CSF) smear gram stain positive bacteria. The glucose was 0.02 mmol/L and cell count was 326*10^6/L in her CSF, even if the blood glucose was 3.8 mmol/L. She was treated with routine treatment: antibiotics and dexamethasone. On day 2, her frequent focal seizures originated from the left side brain because of the magnetic resonance scan demonstrated subdural emission were deterioratedlasted 11 days, PICU stay 2 days. Informed consent was gotten and medical ethnic permission was approved. On day three of admission KD was initiated by fasting for 29 hours, then her blood betahydroxybutyric acid level reached 2.3 mmol/L, and then with 2:1 Qitong (Zeneca, China) liquid ketogenic diet. 3 days later the ratio of KD increased to 3:1. On day 7, three days after ketosis the glucose in cerebral spinial fluid increased quickly from 0.02 mmol/L to 1.98 mmol/L and white cell counts and protein decreased significantly within one week as well. The blood glucose level was 3.94 ± 0.51 mmol/L (n=30), range 2.8-5.3 mmol/L, median 3.9 mmol/L, 95% CI 3.75-4.13 mmol/L. The blood ketone body (beta-hydroxybutyric acid) level was 1.5 ± 0.82 mmol/L (n=21), range 0.5-3, median 1.2 and 95% CI 1.13-1.88 mmol/L. On day 9 and day 10 of admission the blood betahydroxytutyric acid level was 2.28 ± 0.58 (n=8, range and median, 1.4-3.0,2.4) mmol/L, blood glucose level was 4.13 ± 0.32 (n=8, range and median, 3.7-4.8, 4.10). From day 11, frequent monitoring of blood glucose and ketone body was discontinued. 29 days later she was discharged from hospital. The KD was discontinued after 3 months. The blood sugar and ketone bodies was monitored about every 6 h in hospital, then ketone bodies were monitored two times weekly. After 5.5 months the MRI scan showed mild atrophy of the left brain. Follow-up was performed 1, 3, 6, 12 and 24 months. No symptomatic hypoglycemia and other significant complications happened. No more seizures happened. Her physical and neuropsychological development is similar to that of her same age children at last follow-up. Conclusion: KD might be a safe and effective adjunctive therapy for bacterial meningitis, increasing the glucose in cerebral spinal fluid quickly and inhibiting the inflammation process. It might reduce the complications and sequalae of bacterial meningitis. Further investigations including clinical trial with more cases need to be performed.
Keywords
Bacterial meningitis; Ketogenic diet; Hospital stay; Complications; Sequelae; Encephalomalacia; Pneumonia streptococcus
Introduction
Although with meningococcal and pneumococcal vaccination, and the use of corticosteroids, the incidence of bacterial meningitis decreased, but not its sequelae and mortality have been changed significantly [1,2]. Childhood bacterial meningitis is still the common central nervous system diseases. Long hospital stay, usually a month or so, complications and mortality is still high. Existing treatment mainly anti-infectious, symptomatic and supportive [3], however the pathophysiology of bacterial meningitis ----inflammatory process is not emphasized enough, this might be one of the reasons which leads to long disease course of bacterial meningitis.
Ketogenic diet (KD) is a high fat, low carbohydrate, protein and other nutrients suitable formula diet [4], can inhibit the growth of pathogenic microorganisms [5,6], inhibit inflammation and immune reaction [7,8], substitute glucose to supply brain energy [9], protect the brain from different kinds of damage [10]
The glucose level in cerebrospinal fluid (CSF) of bacterial meningitis is low. The bacterial meningitis is easy to cause the subdural effusion, ependymitis, hydrocephalus and other complications [11]. The glucose transporter 1 deficiency [12] which caused by genetic abnormality the CSF glucose level is low, often cause various types of epileptic seizures and developmental retardation, ketogenic diet therapy is the effective treatment. We assume that based on the existing conventional treatment the ketogenic diet therapy can improve the brain energy metabolism, reduce bacterial meningitis inflammation and shorten the course of the disease, reduce the complications and sequelae.
Clinical Data and Methods
Design
This is a retrospective study, to compare 2 consecutive cases of infants with bacterial meningitis, about the clinical data, treatment and complications. Patients admitted to the hospital in January 2014 and March respectively. This study was approved by Shenzhen Children's Hospital Medical Ethics Committee. Ketogenic diet therapy for patients was performed with guardian’s written and informed consent. Bacterial meningitis diagnostic criteria [13]: 1, clinical features: fever, convulsions, consciousness change, the fontanelle upheaval and other manifestations of intracranial pressure; 2, tests: Cerebrospinal fluid, blood evidence of a bacterial infection, if the bacteriology examination is negative, CSF white blood cells is needed to be 500 × 10^6/L or more.
Treatment
Routine treatment: anti-infection, antibiotics began with experience treatment: Coccus infection with penicillin, vancomycin and bacillus infection treated with amoxyllin, ceftriaxone, meropenem, etc. After admission dexamethasone was administered intravenously, 0.15 mg per kilogram of body weight, once every 6 h for 3 days [14], 15 min before or at the same time with antimicrobial drugs. Successively with valproic acid, oxcarbazepine were used as anticonvulsants. Other treatment was symptomatic and supportive.
Ketogenic diet therapy
Procedure initiated with a fasting until reaching the state of ketosis, 2:1 KD was started, then 3:1 instead to 2:1 for a stable ketosis. KD food was Qitong (Zeneca, Shenzhen Biotechnology Company Ltd.), a liquid vegetable protein drinks. Once every six hours monitoring the blood glucose and blood ketone bodies, and ketone bodies was checked when urination. Monitoring at least for one week, after stable blood ketone and blood glucose reached for at least 48 h, the monitoring frequency decreased [15]. The first appointment was one month after discharge, according to the disease state and KD therapy the consequent follow-up interval was 1-3 months. Ketosis monitoring at about 2 times a week, paying attention to patients’ nutrition and ketosis, monitoring the growth and development.
Statistical processing
Our research data mainly used descriptive statistics, calculated with Excel 2016 software. Statistical variables included blood glucose and blood ketone bodies.
Results
From January to March, 2014 our hospital had 2 consecutive cases of infant bacterial meningitis. The first case was a 55 days old male infant, admitted for 3 days fever and 3 times seizures. He responded well within two weeks and was supposed to discharge in the near future after a brain magnetic resonance imaging test since he otherwise looked normal. It was shocked by finding the unexpected occipital large encephalomalacia. Reviewing the chart the CSF glucose levels were low, but the blood glucose was normal. Given he had convulsions we were wondering whether he also complicated simultaneously with glucose transporter 1 deficiency, ketogenic diet therapy was suggested, hoping to reduce sequela, protect the brain, but the parents refused to the KD therapy and then discharged. After half a month there came the second case, she was a 49 days old female infant of bacterial meningitis. The CSF glucose was only 0.02 mmol/L with clinical suspicion of glucose transporter 1 deficiency. Proposed KD therapy was made on the basis of routine bacterial meningitis treatment. The KD was initiated on day 3 of admission (Table 1). The diagnosis of GLUT 1 deficiency was excluded in both patients.
| Items | Without KD, case 1 | With KD, case 2 |
|---|---|---|
| Ages at onset | 55 days | 49 days |
| Fever duration | 5 days | 20 days |
| Epileptic seizures lasted | 2 days | 7 days, one attack for 30 min |
| Other critically ill indications | Breathing machine assisted for 5 days, thrombocytopenia | Stay in PICU for 2 days because of frequent seizures |
| Bacteria | Meningococcal coccus | Streptococcus pneumoniae |
| CRP on admission, mg/L | 171.8 | 110.5 |
| Head CT scan on admission | none | Mild subdural effusion on the right; subdural effusion on the left, mild bleeding, left ventricle enlarged mildly |
| MRI on admission | none | Bilateral subdural effusion, prominent on the left and mild left high signal |
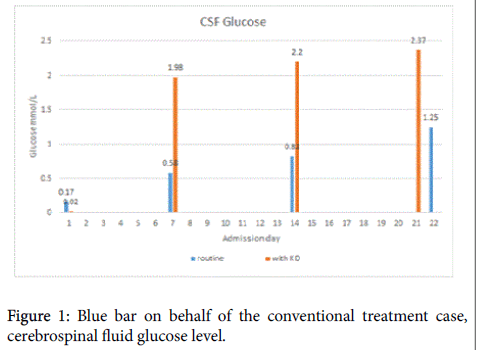
| Profile of CSF glucose | By 3 weeks of admission, from 0.17 to 1.25 mmol/L | By 1 week of admission, ketosis lasted for 3 days, from 0.02 to 1.98 mmol/L |
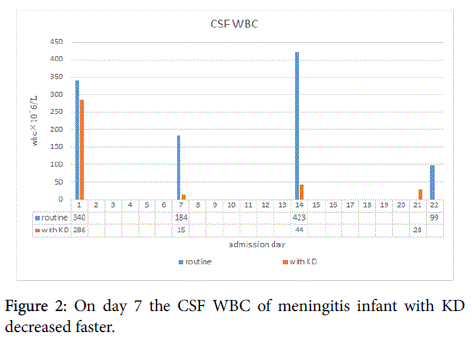
| Profile of CSF white blood cells | Decreased 46% within one week | Decreased 95% within one week |
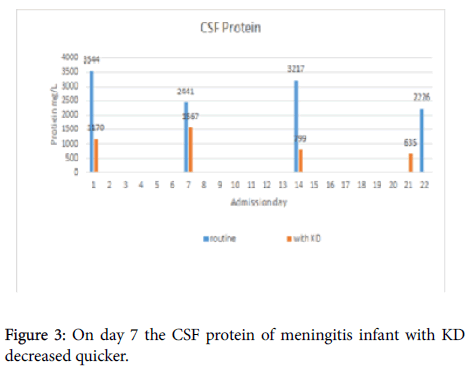
| Profile of CSF protein | Decreased 37% within one week | Decreased 46% within one week |
| Inflammatory indexes(WBC, CRP and PLT) | Extent changed less | Extent changed vigoriously |
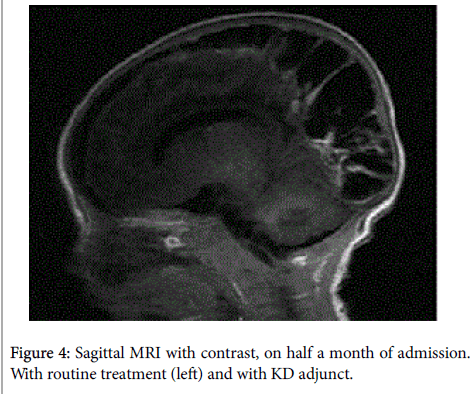
| Head MRI, on half a month of admission | Bilateral occipital large encephalomalacia occurred with edge multiple bleeding, edge and generalized cerebromeningeal intensified on contrast | Severe left subdural effusion, with alongside brain damage, meningeal intensified on contrast, mild focal atrophy and enlarged left cerebral ventricle |
Table 1: Comparison of clinical features in two consecutive patients.
Anti-infection treatment
For case 1, beginning with penicillin add meropenem, after the bacterial culture and drug sensitive experiment antibiotics changed to penicillin and ceftriaxone since the etiology was meningococcal coccus and drug sensitive test results indicated penicillin, ceftriaxone, erythromycin, or cefoperazone sensitive. For case 2, vancomycin plus ceftriaxone were administered. Then came the blood culture results: streptococcus pneumoniae, sensitive to penicillin, ceftriaxone, vancomycin, etc. Successively penicillin and ceftriaxone plus with meropenem.
Ketosis, cerebrospinal fluid and inflammation index changes (Figures 1-3). State of ketosis monitoring: on 3 day of hospital admission KD therapy was initiated with fasting, about 29 h passed, blood ketone body beta-hydroxybutyric acid level 2.3 mmol/L reached--state of ketosis. Then fed with a 2:1 KD liquid, Qitong liquid vegetable protein drinks, gradually add quantity, after 3 days the KD ratio was titrated to 3:1 to for seizure control was not ideal. The blood glucose level was 3.94 ± 0.51 mmol/L (n=30), range 2.8 to 5.3 mmol/L, the median 3.9 mmol/L, 95% confidence interval of 3.75 to 4.13 mmol/L (95% CI 3.75 to 4.13 mmol/L). Blood ketone body beta-hydroxybutyric acid concentration was 1.5 ± 0.82 mmol/L (n=21), range 0.5 to 3.0, the median 1.2 mmol/L, 95% confidence interval was 1.13 to 1.88 mmol/L (95% CI, 1.13 to 1.88 tendency/L). On days 9 and 10 in hospital, the blood levels was 2.28 ± 0.58 mmol/L (n=8, range and median values are respectively, 1.4-3.0, 2.4 mmol/L). The blood glucose level was 4.13 ± 0.32 (n=8, range and median values, respectively, 3.7-4.8, 4.10) mmol/L. From the 11th day of hospitalization blood ketone bodies and glucose monitoring were no longer frequently. He discharged on hospital day 29, ketosis monitoring at least 2 times a week later, according to whether ketosis is stable or not to determine monitoring frequency. The patient maintained on the KD therapy for 3 months (Figure 1). Blue bar on behalf of the conventional treatment case, cerebrospinal fluid glucose level after 1 week from 0.17 mmol/L increased to 0.58 mmol/L, by 3 weeks up to 1.25 mmol/L. Orange bar represented case with both the routine treatment and plus ketogenic diet therapy, cerebrospinal fluid sugar level from 0.02 mmol/L, by 1 week increased to 1.98 mmol/L when the state of ketosis was only 3 days, and by 3 weeks up to 2.37 mmol/L.
Case 1 with meningitis was critically ill at beginning, with and thrombocytopenia, needing breathing machine assisted, after the rescue, he was in a stable condition, ready to discharge from the hospital after an MRI scan. Results showed a big occipital encephalomalacia, with contrast showed the lesion’s edge reinforcement and evidence of bleeding. When consultating author found CSF glucose level was low, the blood sugar was not low, although there are recovery after treatment, but still need exclude glucose transporter 1 deficiency, and advised parents to have ketogenic diet therapy, hoping to increase the level of sugar in the cerebrospinal fluid, or give the brain ketone bodies as an energy, at the same time auxiliary to anti-infection, inhibiting the inflammatory reaction, but the parents refused.
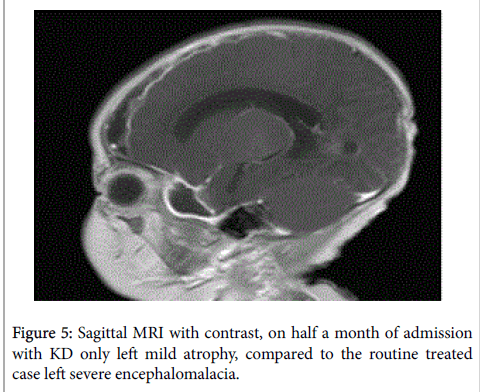
Cases 2, the next consecutive patient was a 49 days old female infant, admitted in hospital for three days fever, one severe convulsions (grand mal like lasted for about 30 min), bacterial meningitis was suspected, given conventional treatment. But fever was high to 39.8 degree’ Fahrenheit and seizures was frequent, she was transformed to PICU. Her blood glucose level was normal, but CSF glucose level very very low, 0.02 mmol/L. She was suggested under the existing guidelines for treatment, at the same time ketogenic diet therapy was added. Magnetic resonance imaging was performed on March 18, 2014. It found some brain damage, including bilateral subdural effusions, more seriously on the left, especially the left subdural effusion complicated with underlying parenchymal damage, meningeal reinforcement, then lead to the left temporal lobe and frontal, parietal lobe (subdural effusion associated with brain atrophy), but much less severe than case 1 (Figures 4 and 5).
Side effects the ketogenic diet
Within 3 days mild diarrhea happened after the ketogenic diet initiating, didn’t need to stop the ketogenic diet therapy.
Discussion
Our study compared manifestations of two infants cases with bacterial meningitis, indicated under the guidance of present bacterial meningitis treatment, the existing therapy adding on with ketogenic diet therapy, patients’ cerebrospinal fluid glucose rise rapidly, CSF white blood cells and proteins could reduce rapidly, while inflammatory indexes such as peripheral white blood cells, CRP and blood platelet could recovered more quickly than the case without ketogenic therapy. By intensive monitoring even if with a fast bedside way couldn't find hypoglycemia, especially no symptomatic hypoglycemia happened. By 5 months more after the disease onset magnetic resonance imaging scanning found only mild left brain atrophy along the area of the subdural effusion. Within 2 years of follow-up, no longer the seizures recurred. The physical and neuropsychological development level was as the same as those of her age.
Ketogenic diet therapy, first used in the treatment of epilepsy [16], also used in a variety of other diseases nowadays [17], including inhibition of bacterial growth, restraining strong immune responses, inhibition of inflammation, instead of glucose for the body's energy supply when in hunger or stress state. More still the ketogenic diet therapy might be used in prevention of epilepsy [18]. The glucose transporter 1 deficiency is caused by genetic defects, its core pathophysiology is that the glucose level in cerebrospinal fluid is low, resulting in epilepsy and development delay. The ketogenic diet therapy can control seizures, provide brain tissue with ketone bodies as an energy source, so it is the first-line therapy of the disease [19]. In bacterial meningitis cerebrospinal fluid glucose level is low, inflammatory process and inflammatory complications such as subdural effusion, hydrocephalus, ependymitis, and brain abscess are prominent manefestations, and thus resulting in encephalomalacia, developmental delay and epilepsy. Ketogenic diet therapy, due to the multiple specific mechanisms of action targeted to pathophysiology might be an optional treatment for bacterial meningitis. With more than 90 years of global practice, ketogenic diet is safe, as the adjuvant treatment of bacterial meningitis might be appropriate [20]. Many years ago ketogenic diet therapy was used to treat some infectious diseases. As far as we know there has yet no report in the literature so far about the ketogenic diet therapy for bacterial meningitis. Our case study suggested that, on the basis of existing routine bacterial meningitis treatment, adding on with ketogenic diet therapy, could promote disease recovery, reduce complications and sequlae.
Despite childhood bacterial meningitis leading to brain lesions is common, study of the mechanism and treatment is rare. In this study, through a series of magnetic resonance imaging, subdural effusion is demonstrated to occur with severe local cerebromeningeal inflammation, adjacent brain tissue damage such as blood brain barrier damage, brain tissue necrosis, which in turn leads to brain atrophy. Long-term neurologic deficit and epilepsy may occur. Other complications such as ependymitis, hydrocephalus, brain abscess, etc., are linked to inflammation and blood brain barrier damage. In the pathophysiology of bacterial meningitis there exists inflammation, characterized clinically by fever, high white blood cells, C-reactive protein and blood platelet, which is a complicated process. Too severe inflammation is harmful to the body tissue. To study the pathological complications and physiological mechanism is helpful to find new treatment targets. Therefore adrenal glucocorticoids which work on many targets inhibit inflammation and are effective in treatment of bacterial meningitis. Similarly, the ketogenic diet therapy might be effective for bacterial meningitis.
Our study suggested potential use of ketogenic diet therapy to bacterial meningitis. Due to only few cases, prospective, multicenter randomized controlled clinical trial about adjunct therapy of ketogenic diet to infant bacterial meningitis is already in progress.
Acknowledgement
We thank Lei Zhang, Runqi Luo and Kewei Fang for assisting to collect some data and guidance to patients as KD dieticians.
References
- Castelblanco RL, Lee M, Hasbun R (2014) Epidemiology of bacterial meningitis in the USA from 1997 to 2010: A population-based observational study. Lancet Infect Dis 14: 813-819.
- Bijlsma MW, Bekker V, Brouwer MC, Spanjaard L, Beek VD, et al. (2014) Epidemiology of invasive meningococcal disease in the Netherlands, 1960-2012: An analysis of national surveillance data. Lancet Infect Dis 14: 805-812.
- Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, et al. (2004) Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 39: 1267-1284.
- Liao JX (2012) The clinical protocol of ketogenic diet therapy. Chinese Journal of Practical Clinical Pediatrics 29: 2-4.
- Robb DC (1933) The ketogenic diet in the treatment of infections of the urinary tract. Br Med J 2: 1158-1162.
- Wilson CM (1933) The treatment of chronic E. coli infections of the urinary tract by a ketogenic diet. Postgrad Med J 9: 96-99.
- Youm YH, Nguyen KY, Grant RW, Goldberg EL, Bodogai M, et al. (2015) The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med 21: 263-269.
- Ni FF, Li CR, Liao JX, Wang GB, Lin SF, et al. (2016) The effects of ketogenic diet on the Th17/Treg cells imbalance in patients with intractable childhood epilepsy. Seizure 38: 17-22.
- Kossoff EH (2015) Commentary: Breaking down the barriers to using dietary therapy for refractory epilepsy. Epilepsia 56: 1335-1336.
- Kim DY, Davis LM, Sullivan PG, Maalouf M, Simeone TA, et al. (2007) Ketone bodies are protective against oxidative stress in neocortical neurons. J Neurochem 101: 1316-1326.
- Quagliarello V, Scheld WM (1992) Bacterial meningitis: pathogenesis, pathophysiology and progress. N Engl J Med 327: 864-872.
- Kass HR, Winesett SP, Bessone SK, Turner Z, Kossoff EH (2016) Use of dietary therapies amongst patients with GLUT1 deficiency syndrome. Seizure 35: 83-87.
- Kim KS (2010) Acute bacterial meningitis in infants and children. Lancet Infect Dis 10: 32-42.
- Odio CM, Faingezicht I, Paris M, Nassar M, Baltodano A, et al. (1991) The beneficial effects of early dexamethasone administration in infants and children with bacterial meningitis. N Engl J Med 324: 1525-1531.
- Suo C, Liao J, Lu X, Fang K, Hu Y, et al. (2013) Efficacy and safety of the ketogenic diet in Chinese children. Seizure 22: 174-178.
- Freeman JM, Kossoff EH (2010) Ketosis and the ketogenic diet, 2010: Advances in treating epilepsy and other disorders. Adv Pediatr 57: 315-329.
- Kossoff E, Freeman J, Turner Z, Rubenstein J (2011) Ketogenic diets: Treatments for epilepsy and other disorders. 5th edition New York: Demos Medical Publishing.
- Gama IR, Filho EMT, Oliveira SL, Bueno NB, Melo IT, et al. (2015) Effects of ketogenic diets on the occurrence of pilocarpine-induced status epilepticus of rats. Metab Brain Dis 30: 93-98.
- Kass HR, Winesett SP, Bessone SK, Turner Z, Kossoff EH (2016) Use of dietary therapies amongst patients with GLUT1 deficiency syndrome. Seizure 35: 83-87.
- Wheless JW (2008) History of the ketogenic diet. Epilepsia 49: 3-5.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13917
- [From(publication date):
June-2016 - Jul 12, 2025] - Breakdown by view type
- HTML page views : 12888
- PDF downloads : 1029