Case Report Open Access
Acute Gastrointestinal Bleeding with Hypovolemic Shock Induced by Gastrointestinal Stromal Tumor Coincident with Neurofibromatosis Type 1: A Case Report
Gha Na Jo1, Kang Hong Lee2 and Byung Kyu Ahn2*
1Department of Surgery, Hanyang University Medical Center, Seoul, Korea
2Department of Surgery, Hanyang University College of Medicine, Seoul, Korea
- *Corresponding Author:
- Byung Kyu Ahn, MD, PhD
Address: Department of Surgery
Hanyang University College of Medicine 17 Haengdang-dong
Seongdong-ku, Seoul 133-792, Korea
Tel: +82-2-2290-8460
Fax: +82-2-2281-0224
E-mail: bkahn@hanyang.ac.kr
Received date: May 15, 2015; Accepted date: June 06, 2015; Published date: June 12, 2015
Citation: Na Jo G, Lee KH, Ahn BK (2015) Acute Gastrointestinal Bleeding with Hypovolemic Shock Induced by Gastrointestinal Stromal Tumor Coincident with Neurofibromatosis Type 1: A Case Report. J Gastrointest Dig Syst 5:299. doi:10.4172/2161-069X.1000299
Copyright: © 2015 Na Jo G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License; which permits unrestricted use; distribution; and reproduction in any medium; provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
We report a case of young patient diagnosed as Neurofibromatosis type 1 (NF-1) five years ago. A 42-year-old male was admitted due to sudden onset of gastrointestinal bleeding. Contrast enhanced computed tomography (CT) scan revealed a lobulating unenhanced mass, originating from the small bowel in the pelvic cavity. The patient developed a fulminant gastrointestinal hemorrhage and emergency operation was performed. On operation, multilobulated submucosal mass was observed on the serosal surface of proximal ileum and this tumor with hemorrhagic and cystic change was the source of bleeding. Histopathological examination revealed this tumor was 5.5 cm × 5 cm × 4 cm in size and small bowel gastrointestinal stromal tumor (GIST) with moderate risk malignant potential. Immunohistochemical examination showed that C-kit and CD34 were positive. In neurofibromatosis, GISTs are more frequent and we should pay attention to gastrointestinal manifestation in such patients.
Keywords
Neurofibromatosis type 1; Gastrointestinal stromal tumor; Gastrointestinal bleeding; Hypovolemic shock
Introduction
Neurofibromatosis type 1 (von Recklinghausen's disease, NF-1) is an autosomal-dominant neurocutaneous disorder characterized by abnormal skin pigmentation (café au lait spots and axillary freckling), cutaneous and plexiform neurofibromas, skeletal dysplasias, and Lisch nodules (pigmented iris hamartomas) [1-4]. Gastrointestinal stromal tumor (GIST) is the most common mesenchymal tumor of the gastrointestinal tract and can present in a variety of diverse symptoms from vague abdominal pain to massive gastrointestinal bleeding [3-6]. The incidence of GIST is approximately 1.5:100,000 [5,7]. However, recent studies have pointed out that GISTs are more common among NF-1 patients, with an increased incidence of 3.9~25% [8]. We report the case of a 42-year-old male patients with NF-1 who presented with lower gastrointestinal bleeding caused by an ileal GIST.
Case Report
A 42-year-old male was admitted to our hospital with sudden onset of gastrointestinal bleeding and chest discomfort through the emergency room. His medical history revealed that the patient has never been hospitalized with gastrointestinal symptoms. The patient has been diagnosed, based on pathological findings of excised masses on upper extremities, as NF-1 five years ago.
On arrival, he had a normal body temperature of 37.1°C, moderate tachycardia of 124 beats/minute and low blood pressure of 80/50 mmHg. Physical examination findings were normal except for multiple neurofibromas on his trunk and extremities. When admitted, laboratory investigations showed that white blood cell count 15,800/mm3 (segmented neutrophils 89.4%), hemoglobin 8.8 g/dL, and platelets 318,000/mm3. Blood chemistry results were albumin 3.9 g/dL, total bilirubin 1.9 mg/dL, AST/ALT 29/30 IU/L, and BUN/creatinine 38/0.8 mg/dL. There were no significant findings for electrolytes or urinalysis. Chest and abdominal films showed no abnormal finding.
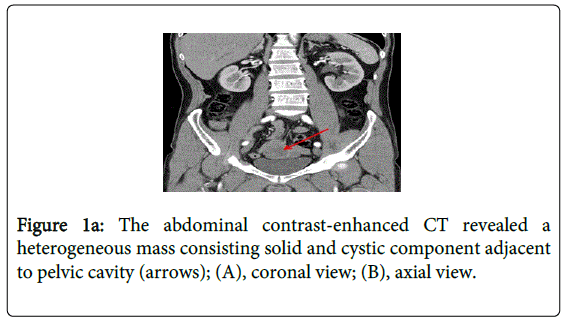
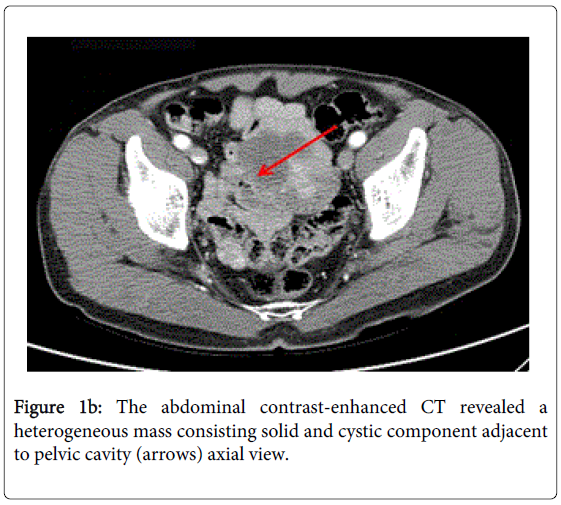
After blood transfusion, the amount of bleeding was gradually reduced and he remained hemodynamically stable for first 24 hours. The source of bleeding could not be identified by gastrofiberscopy, colonofiberscopy and bleeding scan. Abdominal computed tomography (CT) scan revealed a lobulating unenhanced mass, originating from the small bowel in the pelvic cavity (Figures 1a and 1b). However, the patient developed a fulminant gastrointestinal hemorrhage and hemoglobin level was rapidly decreased from 11.7 g/dL to 7.5 g/dL even transfusion of packed red blood cell (PRC) 5 units over the next 20 hours.
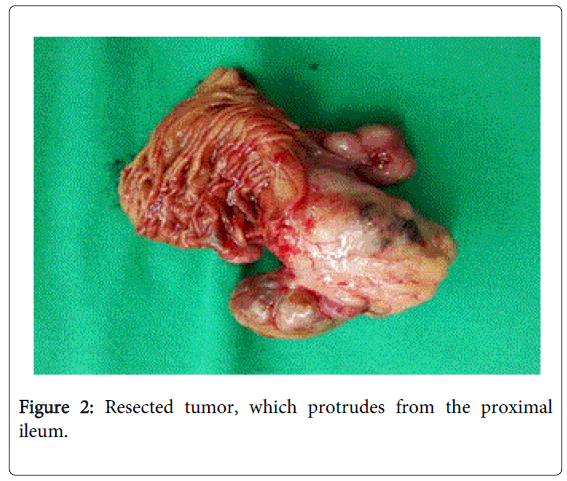
Emergency laparotomy was performed. At surgery, multilobulated brownish mass, which was the source of bleeding, was found on the serosal surface of proximal 40 cm from ileocecal valve. Segmental resection of the small bowel and side-to-side anastomosis was performed. Grossly, resected tumor was 5.5 cm × 5 cm × 4 cm in size with hemorrhagic and cystic change (Figure 2).
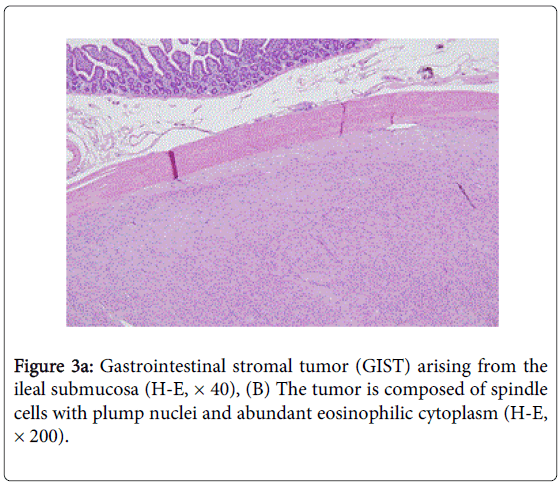
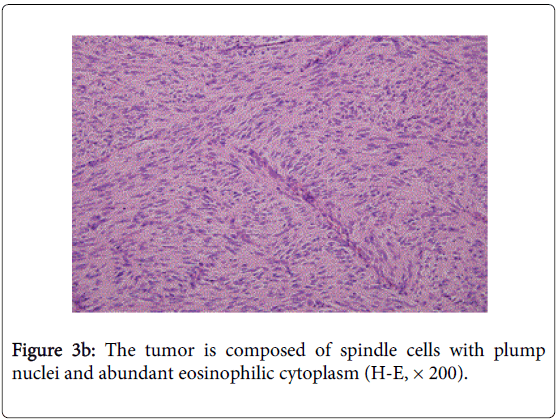
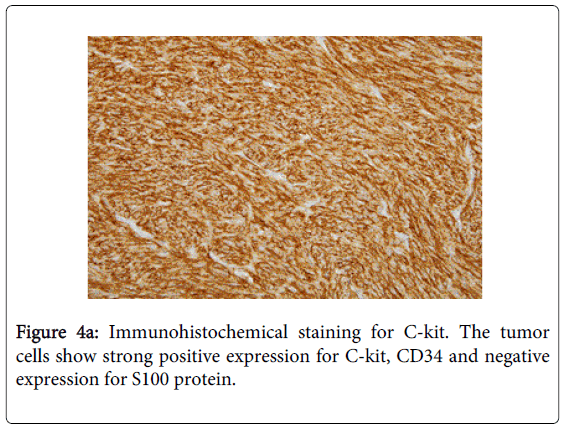
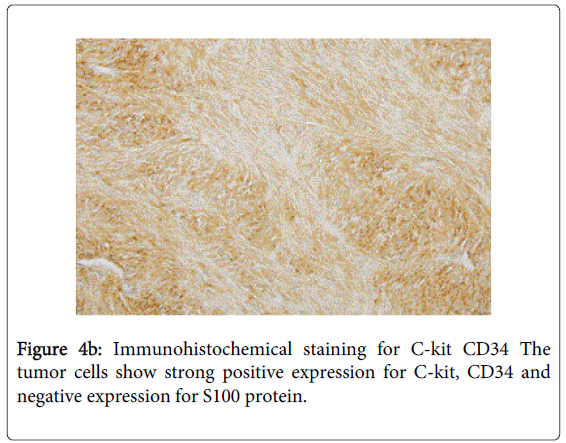
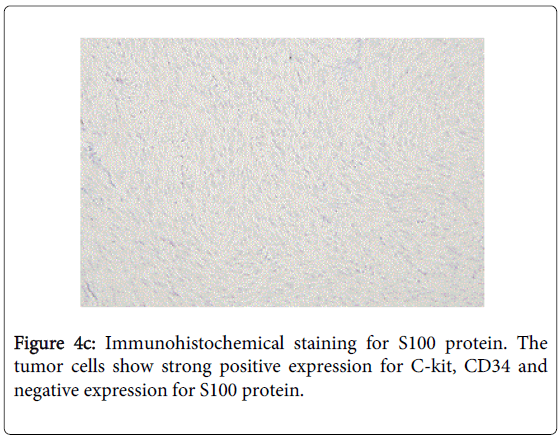
Histopathological examination revealed this multiple submucosal masses were small bowel GIST with moderate risk malignant potential (Figures 3a and 3b). Immunohistochemical examination showed that C-kit and CD34 were positive for tumor cell (Figures 4a-4c).
After operation, the patient recovered uneventfully and was discharged 9 days later. No adjuvant treatment was performed, and there had been no evidence of recurrence during 1 year.
Discussion
NF-1 is an autosomal dominant hereditary disease that may affect the gastrointestinal tract in up to 25% of patients [1,5,8]. Hyperplastic lesion of intestinal neural tissue, GIST, endocrine cell tumor of the duodenum or periampullary region, and a miscellaneous tumors are included in NF-1 associated disease entities [4].
GISTs in patients with NF-1 are histologically and immunophenotypically distinct from those in patients without NF-1. Sporadic GISTs only account for 1-3% of all gastrointestinal neoplasm [4,6,7]. On the other hand, recent studies have pointed out that GISTs are more common among NF-1 patients, with an increased incidence of 3.9~25% [3-6,8]. Sporadic GISTs occur predominantly in individuals over 50 years of age (the mean age of one series being 56.2 years), whereas GISTs that occur in NF1 patients usually tend to manifest at a younger age [1,6,9]. In our case, the patient was relatively young (42-year-old) male. The most common location of a GIST in non-NF-1 patients is in the stomach (60-70%), followed by the small intestine (20-30%), colon and rectum (5%), and esophagus (5%) [2,4,6]. On the contrary, NF-1-associated GISTs occur in the jejunum or ileum and is often multiple (Table 1). In our case, the GIST was located in proximal ileum with single lesion and we could not find the bleeding focus using a conventional endoscopy. In this situation, further diagnostic tools such as bleeding scan, CT angiography or capsule endoscopy should be considered.
| NF-1 associated GIST | Sporadic GIST | |
|---|---|---|
| Age | Relatively young (<50 years) | About 60 years |
| Gender | Slightly female dominant | Slightly male dominant |
| Location | Small intestine>stomach | Stomach (60-70%) |
| Small intestine (20-30%) | ||
| Colon, rectum (5%) | ||
| Esophagus (5%) | ||
| Number of tumor | Multiple | Solitary |
| Histology | Spindle cell dominant | Spindle cell (70%) |
| Epitheloid cell (20%) | ||
| Mixed (10%) | ||
| Mutation | NF-1 | c-KIT/PDGFRA |
| Malignant potential | Relatively uncommon | More common |
| Prognosis | Good | Relatively bad |
Table 1: A comparison between sporadic GIST and NF-1 associated GIST.
In the previous reports, Kazunori Tsukuda et al. [3] performed laparoscopic resection in a 79-year-old female patients with multiple GISTs associated with NF-1. They reported that laparoscopic surgery would be useful for examination and minimally invasive approach to tumors, especially on cases with vitally stable patient. Although he did not treat adjuvant medication, no recurrence occurred. In our case, the patients suddenly developed the hemorrhagic shock with massive bleeding and laparoscopic surgery was not indicated.
Ku et al. [6] described a 33-year-old woman with a spontaneously ruptured jejunal GISTs presenting with generalized peritonitis. Their patient had surgery as primary management and recovered uneventfully. However two other spontaneously ruptured GIST patients died in spite of surgical intervention [10,11]. In Han’s report [1], their patient started imatinib treatment after surgery, but stopped medication due to dyspepsia after a few months and eventually progressed after 18 months. With these cases, patients with GIST associated with NF-1 would present diverse manifestations and unexpected clinical outcomes.
Conclusion
This case is the rare presentation of ileal GIST with massive gastrointestinal bleeding in NF-1 which led to hemorrhagic shock. Patients with NF-1 have an increased risk of gastrointestinal tumors, such as GIST. Therefore, clinicians should pay attention to a medical history, physical examination and gastrointestinal manifestation in patients with these two disease entities.
References
- Han SH, Park SH, Cho GH, Kim NR, Oh JH, et al. (2007) Malignant gastrointestinal stromal tumor in a patient with neurofibromatosis type 1. Korean J Intern Med 22: 21-23.
- BajorJ (2009) Gastrointestinal stromal tumors in patients with type 1 neurofibromatosis. ClinExp med J 3: 247-254.
- Tsukuda K, Ikeda E, Takagi S, Miyake T, Muraoka T, et al. (2007) Multiple gastrointestinal stromal tumors in neurofibromatosis type 1 treated with laparoscopic surgery. Acta Med Okayama 61: 47-50.
- Kalender M, Sevinc A, Tutar E, Sirikci A, Camci C (2007) Effect of sunitinib on metastatic gastrointestinal stromal tumor in patients with neurofibromatosis type 1: a case report. World J Gastroenterol 13: 2629-2632.
- Esam A, Manish K, Osama D, Roben C (2009) c-KIT positive Gastrointestinal Stromal Tumor presenting with acute bleeding in a patient with neurofibromatosis type 1: a case report. International Seminars in Surgical Oncology 6: 1-3.
- Ku MC, Tsai CM, Tyan YS (2010) Multiple gastrointestinal stromal tumors in a patient with type I neurofibromatosis presenting with tumor rupture and peritonitis. Clin Imaging 34: 57-59.
- Kindblom LG, Meis-Kindblo J, Bümming P (2002) Incidence, prevalence, phenotype and biologic spectrum of gastrointestinal stromal cell tumors (GIST) - a population based study of 600 cases. Ann Oncol 13 suppl 5: 157.
- Yantiss RK, Rosenberg AE, Sarran L, Besmer P, Antonescu CR (2005) Multiple gastrointestinal stromal tumors in type I neurofibromatosis: a pathologic and molecular study. Mod Pathol 18: 475-484.
- Miettinen M, Fetsch JF, Sobin LH, Lasota J (2006) Gastrointestinal stromal tumors in patients with neurofibromatosis 1: a clinicopathologic and molecular genetic study of 45 cases. Am J SurgPathol 30: 90-96.
- Kitabayashi K, Seki T, Kishimoto K, Saitoh H, Ueno K, et al. (2001) A spontaneously ruptured gastric stromal tumor presenting as generalized peritonitis: report of a case. Surg Today 31: 350-354.
- Ajduk M, Mikulic D, Sebecic B, Gasparov S, Patrlj L, et al. (2004) Spontaneously ruptured gastrointestinal stromal tumor (GIST) of the jejunum mimicking acute appendicitis. Coll. Antropol 28: 937-941.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16512
- [From(publication date):
June-2015 - Jul 06, 2025] - Breakdown by view type
- HTML page views : 11870
- PDF downloads : 4642