Research Article Open Access
Active Weight Bearing Tibio-talar Motion and Meniscal Translation in the S.T.A.R Prosthesis-A Radiographic Comparative Study of the S.T.A.R. Toward the Opposite Normal Ankle Joint
Hakon Kofoed*The Orthopaedic Clinic, Frederiksberg University Hospital, Capital Region of Denmark
- *Corresponding Author:
- Hakon Kofoed
30 Norasvej, Charlottenlund, Denmark
Tel: +4521782799
E-mail: hakon.kofoed@gmail.com
Received Date: December 13, 2012; Accepted Date: December 28, 2012; Published Date: January 02, 2013
Citation: Kofoed H (2013) Active Weight Bearing Tibio-talar Motion and Meniscal Translation in the S.T.A.R Prosthesis-A Radiographic Comparative Study of the S.T.A.R. Toward the Opposite Normal Ankle Joint. Clin Res Foot Ankle 1:101. doi: 10.4172/2329-910X.1000101
Copyright: © 2013 Kofoed H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Background: The kinematics of meniscal bearing artificial ankle joints is not well documented after the implantation of the prosthesis. Purpose of the study To investigate the active weight-bearing tibio-talar motion and the translation of the meniscus radiographically after mean 36 months in patients with unilateral traumatic ankle osteoarthritis.
Methods: Straight lateral radiographic views under image intensification of the replaced ankle and the opposite normal ankle were performed during active weight-bearing. The tibio-talar motion of both ankles, as well as the translation/rotation of the meniscus in the replaced ankles was measured.
Results: The total range of motion in normal ankles was mean 59° (33.7–68.7). The motion in the replaced ankles was mean 37.2° (16.7–53.3), p<0.02. Normal extension was mean 24° (3.7–37.7). Replaced ankle extension was mean 14.7° (2-26.7), p<0.02. Normal plantarflexion was mean 31° (19.7–51), in replaced ankles plantar flexion was mean 22.3° (12.3–34), p<0.02. The translation of the meniscus was 0.7 mm (-1.5 to 1.2). This could also be calculated to be a rotation of 3.9°. The translation of the meniscus is most probably a combination of gliding and rotation.
Conclusions: The active weight-bearing motion of the replaced ankle is about 2/3 of the normal ankle motion. Functionally this is a satisfactory result. After 36 months the translation of the meniscus is rather small suggestion that the replaced ankle has reached a steady state of conformity.
Keywords
Total ankle replacement; Active weight-bearing motion; Meniscal translation
Introduction
Radiographic measurements of flexion-extension of the ankle joint have shown clinical measurements to be unreliable [1,2]. The true motion in the tibio-talar junction is therefore best judged by radiography. Modern ankle replacements with mobile bearings have been claimed to give better mobility than the previous two-component Fixed Bearing (FB) designs [3,4]. The meniscus-bearing principle allows for gliding as well as rotation of the meniscus during the arc of motion. In a previous study we investigated the radiographic passive mobility of a Meniscal- Bearing (MB) ankle replacement preoperatively and at 12 months follow-up. The gain in motion was 80% [5]. Only one other study has examined the active weight-bearing motion of ankle replacements [2]. That study did not take into consideration that the rotation of the meniscus would influence the measured anterior-posterior gliding of the meniscus. Clinical measurements of ankle joint motion are biased by the mobility of the neighboring joints. In the normal ankle joint the clinically measured active weight-bearing mobility in the ankle exceeds that of the passive motion [6]. We therefore compared radiographic measurements of active weight-bearing motion in unilateral ankle replacements with active weight-bearing measurements of the opposite normal ankle.
Materials and Methods
Fifteen consecutive cases wit unilateral osteoarthritis of the ankle joint secondary to trauma were treated with a MB ankle joint replacement, Scandinavian Total Ankle Replacement (S.T.A.R., Waldemar Link, Germany).
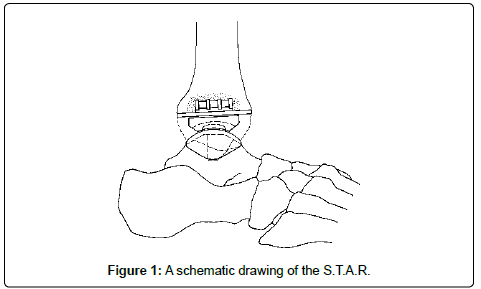
The average Age of the patients was 55 years (range 30-74). The operative technique has been described previously [7,8]. Figure 1 shows the principle of the ankle prosthesis. It consists of a metal talus cap that also resurfaces the lateral and medial facets of the talus, and is near anatomical in its shape. The tibial component is flat. On its back it carries two cylinders for insertion into the distal tibial subchondral bone. A polyethylene meniscus–congruent toward both the tibial and the talus surfaces–is inserted between the metal components. The arrangement allows for near physiological kinematics of the ankle joint. The stability of the joint depends on the malleoli, the ligaments and the contour of the prosthetic surfaces.
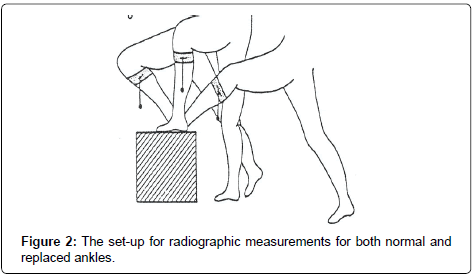
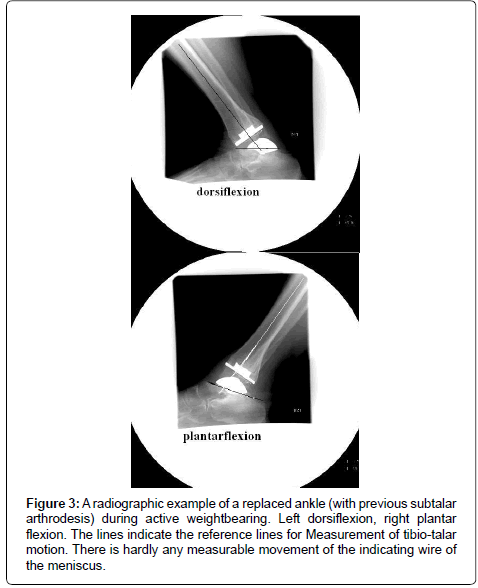
Using image intensification, the radiographic examination was performed after an average follow-up of 36 months (range 24-48).Three of the radiographic examinations failed to show a direct lateral view of the meniscus. These cases were excluded. Figure 2 shows the set-up. The patients would bend over in the knee joint as much as possible with full weight-bearing on the foot, and would afterward stretch the knee out and lean back as much as possible for maximal plantar flexion of the ankle joint. In both situations the heel was firmly pressed to the box surface. The same procedure were used for both replaced and for normal ankles. Straight lateral views were taken in order to clearly identify the marker in the meniscus of the replaced ankles. The longitudinal axis of the tibia constituted one line. Another line went from the top of the talus neck to the posterior process of the talus (Figure 3). Neutral position was sad to a line tangentially to the long axis of the tibia. From these lines the active extension and plantar flexion as well as the total range of motion could be measured for both normal and replaced ankles. The translation between the meniscus and the tibial replaced surface was measured between the tangential lines to the metal marker in the meniscus and the tibial metal plate. The metal marker thread is placed horizontally in the meniscus in a square measuring 2x2 cm. On radiographs it should present as a straight line parallel to the tibial plate. The difference in translation between the marker thread and tibial plate for maximal extension to maximal flexion was said to constitute the translation. The actual length of both the marker and the tibial plate was known and measurements were corrected accordingly. Measurements were performed independently by three investigators, and the results are displayed as the mean of these measurements.
Figure 3: A radiographic example of a replaced ankle (with previous subtalar arthrodesis) during active weightbearing. Left dorsiflexion, right plantar flexion. The lines indicate the reference lines for Measurement of tibio-talar motion. There is hardly any measurable movement of the indicating wire of the meniscus.
In a previous study 11 similar cases using the same devise were measured after 12 months for passive radiographic range of motion [5]. Passive non-weight-bearing ankle motion and active weight-bearing ankle motion could therefore be compared. In another study [6] the passive radiographic motion was measured of 100 normal ankle joints. These results constitute the normal passive radiographic tibio-talar motion.
Statistically p: 0.05 was set as the level of significance. Non-parametric statics were used for comparison of the present and previous reported results.
The study was approved by the local ethical committee. The patients gave informed consent. No funds were received for the study.
Results
Table 1 shows the results of active weight-bearing motion of the replaced and normal ankle joints. The motion of the replaced joints was significantly lower than that of the normal joints (p< 0.02). The replaced ankles showed 2/3 of the normal range. Plantar flexion was close to 3/4 of the normal joint, whereas extension was 3/5 of the normal joint. Table 2 shows a comparison of passive and active ankle prosthesis motion compared to passive and active weight-bearing of normal joints. In both situations active weight-bearing motion exceeded that of passive motion (p<0.05).The translation of the meniscus between maximal extension and maximal plantar flexion was measured to be 0.7 mm (range -1.5 mm to +1.2 mm) in either forward or backward position (Table 3). Theoretically, there is free rotation between the meniscus and the tibia plate. The length of the squared 2 cm metal marker in the meniscus could radiographically maximally be increased to 2.83 cm in 45° of rotation. This means 0.18 mm/degree of rotation. A measurement of 0.7 mm in AP-gliding could therefore also mean a rotation of 3.3°.
| Replaced ankles | % of normal | Normal ankle joints | p | |
|---|---|---|---|---|
| No of cases | 15 | 15 | ||
| Mean total range of motion +/- SE | 37.2 (16.7-52.3) | 64 % | 58.2 (33.7-68.7) | <0.02 |
| Mean plantar flexion +/- SE | 22.3 (12.3-34.0) | 72 % | 31.0 (19.7-51.0) | <0.02 |
| Mean dorsiflexion +/- SE | 14.7 (2.0-26.7) | 61 % | 24.0 (3.7-37.7) | <0.02 |
Table 1: Comparison of active weightbearing motion in replaced and normal ankle joints.
| Passive motion (replaced) [5] | Active weightbearing motion (replaced)** | Passive motion normal [2] | Active motion norma** | |
|---|---|---|---|---|
| No of cases | 11 | 15 (3 excluded for suboptimal radiographs) | 100 | 15 |
| Total range of motion | 27 +/- 10 | 38 +/- 10 | 46 +/- 6 | 58 +/- 11 |
** Ref current paper
Table 2: Radiographic measurements of total passive motion and active weightbearing motion in normal and replaced ankles.
| Patient No | Distance dorsiflexion | Corrected distance (A) | Distance plantarflexion | Corrected distance (B) | Meniscal translation mm (A-B) |
|---|---|---|---|---|---|
| 1 | 28.0 | 20.8 | 24.0 | 19.6 | +1.2 |
| 2 | 17.0 | 14.4 | 16.0 | 14.0 | +0.4 |
| 3 | 28.0 | 22.0 | 22.0 | 21.2 | +0.8 |
| 4 | 21.0 | 20.0 | 19.0 | 19.0 | +1.0 |
| 5 | 30.0 | 22.4 | 28.0 | 23.7 | -1.3 |
| 6 | 28.5 | 24.2 | 28.0 | 23.7 | -0.5 |
| 7 | 26.5 | 21.2 | 30.0 | 21.6 | -0.4 |
| 8 | 19.0 | 15.2 | 20.5 | 16.7 | -1.5 |
| 9 | 25.0 | 21.9 | 23.5 | 21.6 | +0.3 |
| 10 | 31.0 | 22.8 | 29.0 | 23.6 | -0.8 |
| 11 | 34.0 | 25.6 | 33.0 | 25.3 | +0.3 |
| 12 | 30.5 | 20.3 | 25.5 | 20.2 | +0.1 |
Average 0.7 (range -1.5 to + 1.2)
In the radiographs of cases 13, 14 and 15 the indicator line in the meniscus was too badly visualized to get true measurements.
Table 3: Antero-posterior translation of the meniscus.
Discussion
Normal passive range of motion in the ankle joint has been measured by radiography. Extension was mean 14°, and flexion was mean 32° [1,2]. Radiographic studies of first generation ankle replacement mobility are few [9,10], and the average total motion did not increase or exceed 20°. Based on clinical measurements it has been claimed that MB ankle replacements gave better motion than FB designs [3,4]. We have demonstrated radiographically that the gain in passive motion in the MB ankle is significant larger than that of radiographic measured passive motion in the previous FB designs [5]. Komistek et al. [2] found the weight-bearing total range of motion of a MB ankle replacement was 32.3° +/- 24.3° after one year. From a study comparing clinical measurements of passive and active weight-bearing ankle joint motion, it was found that latter exceeded the former [6]. It could therefore be anticipated that the radiographic active weight-bearing ankle motion would exceed that of radiographic passive ankle motion. Performing this we found that the weight-bearing ankle motion in normal ankles exceeded that of radiographic passive motion of normal ankles reported previously [1]. This also applied to ankle replacements where both extension and flexion under active weight-bearing exceeded that of radiographic passive motion. This positive difference between active weight-bearing and passive motion could be explained by a better use of the ankle kinematics potential. Stretching of the muscles, the ankle capsule and possibly an additional talus torque during weight-bearing could explain this difference.
The tibial-meniscus translation from maximal plantar flexion to maximal extension was measured by Komistek et al. [2] to be 2.5 mm at the one-year follow-up. They used a 3-D model fitting program from 2-D data. In their conclusion about ankle kinematics they stated that some internal rotation of the tibia takes place during the arc of motion. This is undoubtedly true, but as the ankle is the most congruent joint this would only be possible with either a widening of the ankle mortise in extension or an external rotation of the fibula. Lundberg [11] found by stereo- roentgen- photo-grammertry that the axis of rotation passed through the centre of the talus. The actual line of rotation was variable with the shape of the talus and with the talus rotation within the ankle mortise during the arc of motion. The external rotation of the allowing for internal tibial rotation has been measured to be 2.2° (range 1.4–4.8) in a cadaver study of normal ankles using stereo-video- photo-grammertry [11]. Others have found it to be about 5° in vivo [11]. This indicates that the rotation within the ankle mortise during the arc of motion is rather small. The restriction for such a rotation is naturally the malleoli, the ankle ligaments and the contour of the gliding surfaces. As the ligaments are tightened during the surgical procedure we are inclined to believe that the additional rotation in the tibio-meniscal junction is quite small. The theoretical maximal calculated rotation in the present series was found to be about 9.5°. When the natural rotation is about 5° is deducted it means that the rotation between the meniscus and the tibial plate could at most be only about 5°. Therefore the measured mean 0.7 mm translation at the tibio-meniscal joint could either be in the anterior-posterior direction, or an expression of rotation of 3.3° (0.7/0.18). A combination of the two events is the more possible explanation. The combination of these corrective movements undoubtedly allows for a better mobility than a single hinged joint, at least during loading. Most probably they also protect against prosthetic loosening as rotational stresses otherwise would have to be transferred to the bone-implant interfaces.
Comparing the active weight-bearing motion of normal ankles with that of MB replaced ankles showed that about 3/5 of normal extension and 3/4 of normal plantar flexion could be expected in ankle replacements. This is more than sufficient for a normal daily life ankle function. As only slight corrective movements occur at the tibio-meniscal junction after an average follow-up of 36 months it might indicate that the specific ankle joint has found its pattern of movement.
References
- Backer M, Kofoed H (1987) Weight bearing and non-weight bearing ankle joint mobility. Med Sci Res 15: 1309-1310.
- Backer M, Kofoed H (1989) Passive ankle mobility: Clinical measurements compared with radiography. J Bone Joint Surg Br. 71: 696-698.
- Bolton-Maggs BG, Sudlow RA, Freeman MA. (1985) Total ankle arthroplasty. A long-term review of the London Hospital experience. J Bone Joint Surg Br 67: 785-790.
- Buechel FF, Pappas MJ, Iorio LJ (1988) New Jersey low contact stress total ankle replacement: Biomechanical rationale and review of 23 cenmentless cases. Foot Ankle Int 8: 279-290.
- Elgaard T, Kofoed H (1999) Radiographic assessment of the mobility of ankle arthroplasty: a prosapective study. Foot Ankle Surg 5: 95-99.
- Giannini S, Catani F, Ceccarelli F. Protesis della tibio-tarsica. Giorn Ital di Ortop e traumatol 1994; suppl 20: 612-624.
- Helweg J, Kofoed H (1998) The fibula rotates during motion in the ankle joint. In: Current status of ankle arthroplasty (Ed. H. Kofoed), Springer publ: 59-63.
- Kofoed H (1995) Cylindrical cemented ankle arthroplasty. Foot Ankle Int 16: 474-479.
- Kofoed H, Danborg L (1995) Biological fixation of ankle arthroplasty. Foot 5: 27-31.
- Komistek RD, Stiehl JB, Buechel FF, Northcut EJ, Hajner ME (2000) A determination of ankle kinematics using fluoroscopy. Foot Ankle Int 21: 343-350.
- Lundberg A (1989) Kinematics of the ankle and foot. In vivo roentgen stereophotogrammetry. Acta orthop Scand. Suppl 223.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 14425
- [From(publication date):
May-2013 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 9850
- PDF downloads : 4575